Different characteristics associated with intensive care unit transfer from the medical ward between patients with acute exacerbations of chronic obstructive pulmonary disease with and without pneumonia
Introduction
Chronic obstructive pulmonary disease (COPD) is the third leading cause of death worldwide (1). The rate of hospitalization due to COPD is increasing (2), and the most common cause of hospitalization is acute exacerbation of COPD (AECOPD) (3). Most patients with AECOPD can be managed on an outpatient basis, but 3–16% of these patients require hospitalization (4,5). In some cases, admission to an intensive care unit (ICU) is necessary when patients have respiratory failure, change in mental status, or hemodynamic instability. However, mortality rates are much higher for patients admitted to the ICU (6). The guidelines of the Global Initiative for Chronic Obstructive Lung Disease (GOLD) suggests potential indication for hospital admission and indication for ICU admission in patients with AECOPD (7).
Community-acquired pneumonia (CAP) is frequently observed in patients with COPD (8). The presence of COPD is related to the increased mortality of patients with CAP (9). Although controversial, it was recently suggested that CAP is not an exacerbation of COPD (10,11).
Considering the high mortality rate in the ICU, determining the risk factors of ICU transfer for patients with AECOPD initially admitted to a medical ward is important. Several studies have shown that 6–10% of patients admitted to the medical ward because of AECOPD were transferred to an ICU (12,13). In the several previous studies, patients with AECOPD caused by pneumonia had higher rates of ICU admission, application of mechanical ventilation, and mortality than AECOPD caused by non-pneumonia (12). In addition, patients admitted to the ICU had a higher pCO2 and lower pH than non-ICU patients (10). The aim of this study was to compare the clinical, laboratory, and treatment characteristics associated with ICU transfer from the medical ward between patients with pneumonic acute exacerbation (PAE) and those with non-pneumonic acute exacerbation (NPAE) of COPD.
Methods
Subjects
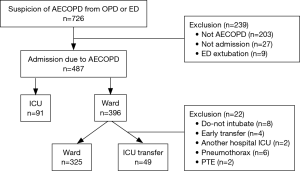
We retrospectively reviewed the medical records of 726 patients who visited the emergency department or were admitted to the medical ward from an outpatient department due to suspicion of AECOPD at Chonnam National University Hospital in South Korea between January 2008 and March 2015. A total of 487 patients fulfilled the criteria for AECOPD according to the guidelines of the American Thoracic Society. Each patient was included only once in the study, even if the patient had been hospitalized more than once. Among the 487 patients, 91 were initially admitted to the ICU, and 396 were admitted to the medical ward. Patients with do-not intubate orders (n=8), early transfer to another hospital (n=4), transfer to another hospital’s ICU due to the lack of a mechanical ventilator (n=2), pneumothorax (n=6), or pulmonary thromboembolism (n=2) were excluded. There was no patient with acute heart failure. Thus, 374 patients were analyzed in this study. The flow chart of the enrollment of patients is shown in Figure 1. Indication for hospital admission was following guidelines of the GOLD: marked increase in intensity of symptoms, severe underlying COPD, onset of new physical signs, failure of an exacerbation to respond to initial medical management, presence of serious comorbidities, frequent exacerbations, older age, insufficient home support (7).During hospitalization in the medical ward, 49 patients required ICU transfer. This decision was made according to the following guidelines of the GOLD for ICU admission (7): severe dyspnea that responds inadequately to initial emergency therapy, changes in mental status (confusion, lethargy, coma), persistent or worsening hypoxemia and/or severely worsening respiratory acidosis despite supplemental oxygen and noninvasive ventilation, the need for invasive mechanical ventilation, and/or hemodynamic instability. Among the 49 patients transferred to the ICU, 44 (89.8%) were transferred due to worsening respiratory failure, which means aggravated hypoxemia or hypercapnia, three (6.1%) were transferred due to hypotension, and two (4.1%) were transferred due to acute kidney injury. Permission was obtained from the Institutional Review Board of Chonnam National University Hospital to review and publish patient records retrospectively (the number of approval: CNUH-2015-126). Informed consent was waived because of the retrospective nature of the study.
The diagnosis of COPD was confirmed in patients with a forced expiratory volume in 1 second/forced vital capacity (FEV1/FVC) ratio <0.70 on post-bronchodilator spirometry according to GOLD criteria (7). COPD was diagnosed prior to admission (81.8%), at admission (6.1%), and during hospitalization (12.0%). AECOPD was defined as the worsening of a patient’s baseline dyspnea, cough, and/or sputum that required a change in their management (7).
We evaluated the clinical, laboratory and treatment characteristics associated with the ICU transfer of patients initially admitted to a medical ward because of AECOPD (ICU group) from patients who were managed at the medical ward during their hospitalization period (ward group). Moreover, we also compared those characteristics between PAE and NPAE groups.
Data collection
The clinical and demographic characteristics, including age, sex, smoking history, body mass index, previous medications, and comorbidities of the patients were recorded at the time of admission. The pneumonia severity index (PSI) score was determined at the time of admission for patients with PAE. Laboratory data, including the white blood cell count [WBC, normal range: (4.8–10.8)×103/µL], platelet count [normal range: (130–450)×103/µL], pH (normal range: 7.35–7.45), arterial partial pressure of carbon dioxide (PaCO2, normal range: 35–48 mmHg), arterial partial pressure of oxygen to fraction of inspired oxygen (PaO2/FiO2), and levels of hemoglobin (normal range: 12–18 g/dL), aspartate aminotransferase (normal range: 10–37 U/L), alanine aminotransferase (normal range: 10–37 U/L), total bilirubin (normal range: 0.22–1.3 mg/dL), blood urea nitrogen (BUN, normal range: 8–23 mg/dL), creatinine (normal range: 0.5–1.3 md/dL), albumin (normal range: 3.5–5.2 g/dL), and C-reactive protein (CRP, normal range: 0–0.6 mg/dL), were obtained at the beginning of the hospitalization. Systemic corticosteroid administration was defined as the oral administration of prednisone (30 to 40 mg per day) or the intravenous administration of an equivalent dose before ICU transfer or discharge. Anemia was defined as hemoglobin levels less than 13.0 mg/dL for men or 12.0 mg/dL for women (14). CAP was defined as the presence of a new pulmonary infiltration on a chest radiograph that was taken at the time of admission in patients from the community with the clinical signs and symptoms of a lower respiratory tract infection (15). Chest radiography results were interpreted by radiologists with routine clinical practice, and confirmed by pulmonologists. NPAE was defined as the signs and symptoms of a lower respiratory tract infection without radiographic pulmonary infiltration in patients with AECOPD.
Statistical analysis
The continuous variables were presented as medians or interquartile ranges (IQRs) and were compared with Mann-Whitney U-tests. The categorical variables were presented as the number or percentage and compared with Chi-squared tests. Univariate analyses were used to analyze the association of each variable with ICU transfer. To determine the predictors of referral to the ICU, a logistic regression analysis was used to perform a multivariate analysis on the variables. In addition, we performed subgroup analyses by dividing the patients into two groups: PAE and NPAE. All statistical analyses were performed with SPSS 21.0 (IBM Corporation, Armonk, NY, USA). P values less than 0.05 were considered statistically significant.
Results
Baseline characteristics of the ward and intensive care unit (ICU) groups
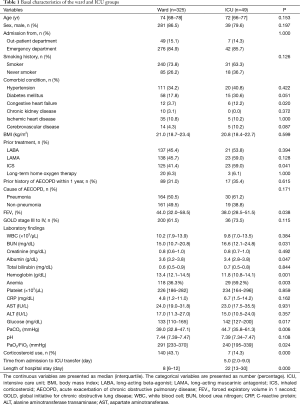
Table 1 shows the basal characteristics of the patients in the ward and ICU groups. The median age was 74 years in the ward group and 72 years in the ICU group. Males were predominant in both groups. Comorbidity with congestive heart failure was more common in the ICU group. The ward group had a higher FEV1 (%) and PaO2/FiO2 and higher levels of albumin and hemoglobin. Systemic corticosteroid administration was more common in the ward group than in the ICU group. The ICU group used inhaled corticosteroids (ICS) more frequently prior to admission and had a higher PaCO2 and higher levels of BUN and glucose at the time of admission to the medical ward. CAP was more common in the ICU group (61.2%) than in the ward group (50.5%), but the difference was not significant (P=0.171). In the ICU group, ICU mortality occurred in 15 (30.6%), and in-hospital mortality occurred in 18 (36.7%).
Full table
Comparisons between ward and intensive care unit (ICU) groups
Table 2 presents the predictors that were associated with the ICU transfer. In the multivariate analysis, prior use of ICS, high BUN levels, presence of anemia, and high PaCO2 independently increased the risk of ICU transfer from the medical ward. However, the use of systemic corticosteroids during hospitalization in the medical ward reduced the risk of ICU transfer (odds ratio, 0.18; P=0.003).
Full table
Comparisons between the pneumonic acute exacerbation (PAE) and non-pneumonic acute exacerbation (NPAE) groups
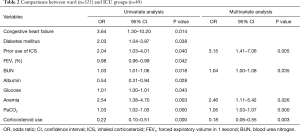
The PAE group contained 194 patients, and the NPAE group contained 180 patients, as shown in Table 3. The median age was 74 in the PAE group and 73 in the NPAE group. The frequency of ICS before admission was similar between the groups. The patients with PAE had a higher WBC count, pH, and FEV1 (%) and higher levels of BUN, creatinine, and CRP. The NPAE group had a higher PaO2/FiO2 and higher levels of albumin and hemoglobin. Treatment with systemic corticosteroids was more frequent in the NPAE group (51.1%) than in the PAE group (28.4%; P=0.000). The in-hospital mortality was higher in the PAE group (7.7%) than in the NPAE group (1.7%; P=0.007).

Full table
Characteristics associated with referral to the intensive care unit (ICU) according to the presence of pneumonia
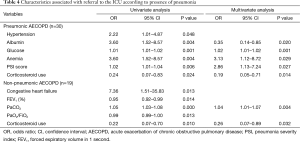
High PSI scores, the presence of anemia, and high levels of glucose increased the risk of ICU transfer from the medical ward in the PAE group (Table 4). High levels of albumin and the use of systemic corticosteroids during hospitalization in the medical ward independently reduced the risk of ICU transfer. In the NPAE group, high PaCO2 levels increased the risk of ICU transfer, and the use of corticosteroids during hospitalization in the medical ward independently decreased the risk of ICU transfer in the PAE group.
Full table
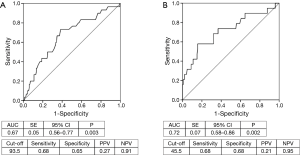
Figure 2 presents a receiver operating characteristic (ROC) curve of the PSI scores of the patients with PAE and the PaCO2 levels in the patients with NPAE.
In the subgroup analysis with patients who transferred to ICU (PAE, n=30 vs. NPAE, n=19), patients with PAE had a higher mortality (P=0.018), higher rate of anemia (P=0.017), lower levels of albumin (P=0.001) and FEV1 (%) (P=0.023), and a higher level of CRP (P=0.010) than patients with NPAE.
Discussion
In this study, we evaluated the associations of clinical, laboratory and treatment characteristics with the referral of patients with AECOPD to the ICU from the medical ward. The prior use of ICS, high levels of BUN, high PaCO2, and the presence of anemia independently increased the risk of referral to the ICU. Systemic corticosteroid administration during hospitalization in the medical ward independently decreased the risk of ICU transfer. In comparing between PAE and NPAE groups, high levels of glucose, high PSI scores, low albumin levels, and the presence of anemia increased the risk of ICU transfer in the PAE group, while only high PaCO2 levels were related to the increased risk of ICU transfer in the patients with NPAE. The use of systemic corticosteroids independently reduced the risk of ICU transfer in both groups.
A previous study showed that the characteristics of patients with both CAP and COPD differ from those of patients with CAP only (16,17). Patients with CAP and COPD have a higher prevalence of Pseudomonas aeruginosa infection and lower levels of circulating inflammatory biomarkers compared with patients with CAP only (18). This difference is partially explained by the chronic and prior use of corticosteroids in patients with both CAP and COPD. In addition, patients with CAP and COPD had higher mean PSI scores, more ICU admissions, and higher 30- and 90-day mortalities than patients with CAP only (9). Patients with both CAP and COPD have different clinical manifestations and worse clinical and laboratory parameters, including lower PaO2 values at hospital admission, higher rates of ICU admission, greater need for invasive mechanical ventilation, and higher mortality, compared with patients with NPAE (10). In a recent study, patients with NPAE had a higher FEV1, more prior episodes of pneumonia, and higher serum levels of CRP, procalcitonin, tumor necrosis factor-α, and interleukin-6 (11). In our study, patients with PAE had higher levels of inflammatory markers, including WBC counts and CRP levels, compared with patients with NPAE who had lower levels of FEV1 (%). These findings were similar to those of a previous study (11). The rate of ICU transfer did not differ in the groups, while the in-hospital mortality was greater in the patients with PAE than in the patients with NPAE. In accordance with the findings of a previous study (10), the patients with PAE had worse clinical features compared with the patients with NPAE.
In comorbid condition, there is higher presence of cerebrovascular disease in the PAE group than NPAE group. This finding could be explained by the high risk for pneumonia development in patients with cerebrovascular disease.
Systemic corticosteroid administration is a standard treatment for AECOPD (19). This treatment improves lung function and clinical symptoms and decreases the length of hospital stays and the rate of treatment failure (20,21). However, comparisons of the benefits of systemic corticosteroid administration have not been conducted in patients with PAE and NPAE. In our study, the number of patients who received systemic corticosteroids was less than the number of patients with PAE. However, the systemic corticosteroids reduced the risk of ICU transfer in the NPAE group as well as in the PAE group. In fact, there is no evidence that systemic corticosteroids worsened the outcomes in patients with CAP and COPD. Systemic corticosteroids may decrease mortality, need for mechanical ventilation, and length of hospital stay in patients with CAP (22-24). Therefore, these findings suggest that the administration of systemic corticosteroids could also reduce the risk of ICU transfer in patients with PAE.
Anemia has been reported in approximately 10–33% of patients with COPD (16,25). COPD with anemia is associated with increased mortality and morbidity (16,25,26). The presence of erythropoietin resistance with chronic inflammatory mechanisms is thought to be a result of anemia with COPD (25). In a previous study by Boixeda et al., there was no difference in the hemoglobin level between the PAE and NPAE groups (17). However, in the present study, anemia was more common in the patients with PAE, and it increased the risk of ICU transfer in those patients. In several previous studies, the correction of the anemia in patients with COPD improved their pulmonary function and respiratory symptoms (27-29). Because it is not clear whether treatment of the anemia would have reduced the amount of ICU transfer of patients with AECOPD, further studies are necessary.
The relationships of the PSI scores and PaCO2 levels with ICU transfer differed according to the etiology of AECOPD. PSI scores are often used to predict the outcomes of patients with CAP. In this study, high PSI scores increased the risk of ICU transfer in patients with PAE. The ROC curve showed that the cut-off value of the PSI score of 93.5 had an area under the curve of 0.67 (sensitivity, 0.68; specificity, 0.65; P=0.003). In contrast to the PSI score, high PaCO2 levels increased ICU transfer risk in the patients with NPAE. In the ROC, the area under the curve of PaCO2 was 0.72 (sensitivity, 0.68; specificity, 0.68; P=0.002). Boixeda et al. attributed these findings as attributing to a greater need for long-term oxygen therapy (17). However, in the present study there was no difference of using long-term oxygen therapy between the PAE and NPAE groups.
Early use of NIV for AECOPD in the general respiratory wards reduces the need for mechanical ventilation and in-hospital mortality (30). Also recently, respiratory intermediate care units (RICUs) can provide an effective NIV application to patients have been introduced in Europe (31). Moreover, RICUs have the advantages to reduce hospital mortality, need for ICU admission, and hospital stay (32). In the present study, NIV was used more in the ICU group than ward group (data was not shown). This result could be due to a more severe condition of patients with NIV use or no RICUs in our hospital. However, there was no difference in the use of NIV between the PAE and NPAE groups.
ICS has been used widely to treat patients with COPD, and recent trials have shown that ICS use is associated with increasing occurrence of pneumonia, and discontinuation of ICS use reduces the elevated risk of serious pneumonia (33-35). In the present study, prior use of ICS in patients with COPD was a risk factor of ICU transfer. However, the frequency of ICS use was not significantly different between the PAE and NPAE groups, and prior ICS use was not a risk factor associated with ICU transfer in the both groups.
There are several limitations to this study. First, because this study was a retrospective single center study, several data were missing from the data collection. As a single center study, numbers of patients who enrolled to this study was small. Although our hospital has a specialized respiratory ward, if inpatient number is higher than the beds in the respiratory ward, patients were admitted to other medical wards. Moreover, there is no RICU in our hospital. Since a better hospital organization such as more respiratory consultations and better quality organized care including RICUs may have lower mortality and better quality organized care including RICUs may have lower mortality and better outcome in patients with COPD (36,37), our findings may not be generalized to all hospitals. Second, anemia was found to be an independent risk factor of ICU transfer in patients with PAE. However, we did not describe the etiology of the anemia because the information required to evaluate the reasons for the anemia was lacking. Third, in this study, there are lack of acute physiologic variables other than arterial blood gas. Fourth, we did not evaluate the long-term outcomes associated with PAE and NPAE. Therefore, future prospective studies are necessary of patients with PAE and NPAE initially admitted to the medical ward.
Conclusions
In conclusion, after the admission to the medical ward due to AECOPD, ICU transfer can occur whenever. However, this study showed that patients with PAE and those with NPAE exhibit several differences associated with ICU transfer. Patients with PAE had a worse clinical course and exhibited higher levels of inflammatory markers, frequent anemia, and a higher in-hospital mortality, while patients with NPAE had higher PaCO2 levels. However, treatment with systemic corticosteroids could reduce the risk of ICU transfer in both patients with PAE and NPAE.
Acknowledgements
Funding: This study was supported by a grant (CRI16005-1) from Chonnam National University Hospital.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Miniño AM, Murphy SL, Xu J, et al. Deaths: final data for 2008. Natl Vital Stat Rep 2011;59:1-126. [PubMed]
- Chapman KR, Bourbeau J, Rance L. The burden of COPD in Canada: results from the Confronting COPD survey. Respir Med 2003;97 Suppl C:S23-31.
- Mannino DM, Homa DM, Akinbami LJ, et al. Chronic obstructive pulmonary disease surveillance--United States, 1971-2000. Respir Care 2002;47:1184-99. [PubMed]
- Seemungal TA, Donaldson GC, Paul EA, et al. Effect of exacerbation on quality of life in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1998;157:1418-22. [Crossref] [PubMed]
- Miravitlles M, Murio C, Guerrero T, et al. Pharmacoeconomic evaluation of acute exacerbations of chronic bronchitis and COPD. Chest 2002;121:1449-55. [Crossref] [PubMed]
- Ai-Ping C, Lee KH, Lim TK. In-hospital and 5-year mortality of patients treated in the ICU for acute exacerbation of COPD: a retrospective study. Chest 2005;128:518-24. [Crossref] [PubMed]
- Rabe KF, Hurd S, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med 2007;176:532-55. [Crossref] [PubMed]
- Soriano JB, Visick GT, Muellerova H, et al. Patterns of comorbidities in newly diagnosed COPD and asthma in primary care. Chest 2005;128:2099-107. [Crossref] [PubMed]
- Restrepo MI, Mortensen EM, Pugh JA, et al. COPD is associated with increased mortality in patients with community-acquired pneumonia. Eur Respir J 2006;28:346-51. [Crossref] [PubMed]
- Lieberman D, Lieberman D, Gelfer Y, et al. Pneumonic vs nonpneumonic acute exacerbations of COPD. Chest 2002;122:1264-70. [Crossref] [PubMed]
- Huerta A, Crisafulli E, Menéndez R, et al. Pneumonic and nonpneumonic exacerbations of COPD: inflammatory response and clinical characteristics. Chest 2013;144:1134-42. [Crossref] [PubMed]
- Groenewegen KH, Schols AM, Wouters EF. Mortality and mortality-related factors after hospitalization for acute exacerbation of COPD. Chest 2003;124:459-67. [Crossref] [PubMed]
- Ranieri P, Bianchetti A, Margiotta A, et al. Predictors of 6-month mortality in elderly patients with mild chronic obstructive pulmonary disease discharged from a medical ward after acute nonacidotic exacerbation. J Am Geriatr Soc 2008;56:909-13. [Crossref] [PubMed]
- World Health Organization. Iron deficiency anemia: assessment, prevention and control: a guide for programe managers. Geneva, 2001.
- Mandell LA, Wunderink RG, Anzueto A, et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis 2007;44 Suppl 2:S27-72. [Crossref] [PubMed]
- Boutou AK, Karrar S, Hopkinson NS, et al. Anemia and survival in chronic obstructive pulmonary disease: a dichotomous rather than a continuous predictor. Respiration 2013;85:126-31. [Crossref] [PubMed]
- Boixeda R, Bacca S, Elias L, et al. Pneumonia as comorbidity in chronic obstructive pulmonary disease (COPD). Differences between acute exacerbation of COPD and pneumonia in patients with COPD. Arch Bronconeumol 2014;50:514-20. [PubMed]
- Crisafulli E, Menéndez R, Huerta A, et al. Systemic inflammatory pattern of patients with community-acquired pneumonia with and without COPD. Chest 2013;143:1009-17. [Crossref] [PubMed]
- Celli BR, MacNee W; ATS/ERS Task Force. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J 2004;23:932-46. [Crossref] [PubMed]
- Niewoehner DE, Erbland ML, Deupree RH, et al. Effect of systemic glucocorticoids on exacerbations of chronic obstructive pulmonary disease. Department of Veterans Affairs Cooperative Study Group. N Engl J Med 1999;340:1941-7. [Crossref] [PubMed]
- Woods JA, Wheeler JS, Finch CK, et al. Corticosteroids in the treatment of acute exacerbations of chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis 2014;9:421-30. [Crossref] [PubMed]
- Confalonieri M, Urbino R, Potena A, et al. Hydrocortisone infusion for severe community-acquired pneumonia: a preliminary randomized study. Am J Respir Crit Care Med 2005;171:242-8. [Crossref] [PubMed]
- Siemieniuk RA, Meade MO, Alonso-Coello P, et al. Corticosteroid Therapy for Patients Hospitalized With Community-Acquired Pneumonia: A Systematic Review and Meta-analysis. Ann Intern Med 2015;163:519-28. [Crossref] [PubMed]
- Torres A, Sibila O, Ferrer M, et al. Effect of corticosteroids on treatment failure among hospitalized patients with severe community-acquired pneumonia and high inflammatory response: a randomized clinical trial. JAMA 2015;313:677-86. [Crossref] [PubMed]
- John M, Hoernig S, Doehner W, et al. Anemia and inflammation in COPD. Chest 2005;127:825-9. [Crossref] [PubMed]
- Martinez-Rivera C, Portillo K, Muñoz-Ferrer A, et al. Anemia is a mortality predictor in hospitalized patients for COPD exacerbation. COPD 2012;9:243-50. [Crossref] [PubMed]
- Schönhofer B, Böhrer H, Köhler D. Blood transfusion facilitating difficult weaning from the ventilator. Anaesthesia 1998;53:181-4. [Crossref] [PubMed]
- Schönhofer B, Wenzel M, Geibel M, et al. Blood transfusion and lung function in chronically anemic patients with severe chronic obstructive pulmonary disease. Crit Care Med 1998;26:1824-8. [Crossref] [PubMed]
- Silverberg DS, Mor R, Weu MT, et al. Anemia and iron deficiency in COPD patients: prevalence and the effects of correction of the anemia with erythropoiesis stimulating agents and intravenous iron. BMC Pulm Med 2014;14:24. [Crossref] [PubMed]
- Plant PK, Owen JL, Elliott MW. Early use of non-invasive ventilation for acute exacerbations of chronic obstructive pulmonary disease on general respiratory wards: a multicentre randomised controlled trial. Lancet 2000;355:1931-5. [Crossref] [PubMed]
- Corrado A, Roussos C, Ambrosino N, et al. Respiratory intermediate care units: a European survey. Eur Respir J 2002;20:1343-50. [Crossref] [PubMed]
- Confalonieri M, Trevisan R, Demsar M, et al. Opening of a respiratory intermediate care unit in a general hospital: impact on mortality and other outcomes. Respiration 2015;90:235-42. [Crossref] [PubMed]
- Calverley PM, Anderson JA, Celli B, et al. Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. N Engl J Med 2007;356:775-89. [Crossref] [PubMed]
- Ernst P, Gonzalez AV, Brassard P, et al. Inhaled corticosteroid use in chronic obstructive pulmonary disease and the risk of hospitalization for pneumonia. Am J Respir Crit Care Med 2007;176:162-6. [Crossref] [PubMed]
- Suissa S, Coulombe J, Ernst P. Discontinuation of Inhaled Corticosteroids in COPD and the Risk Reduction of Pneumonia. Chest 2015;148:1177-83. [Crossref] [PubMed]
- Price LC, Lowe D, Hosker HS, et al. UK National COPD Audit 2003: Impact of hospital resources and organisation of care on patient outcome following admission for acute COPD exacerbation. Thorax 2006;61:837-42. [Crossref] [PubMed]
- Hosker H, Anstey K, Lowe D, et al. Variability in the organisation and management of hospital care for COPD exacerbations in the UK. Respir Med 2007;101:754-61. [Crossref] [PubMed]


