Should we resuscitate or not—that is the question!
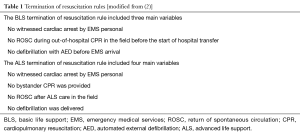
Sudden cardiac arrest is a major public health problem; every year about 350,000 people die in Europe after such an event (1). The 2015 American Heart Association (AHA) as well as the European Resuscitation Council (ERC) guidelines for cardiopulmonary resuscitation (CPR) describe basic life support (BLS) and advanced life support (ALS) rules for termination of resuscitation (TOR) (2). Several studies have evaluated the generalizability of the TOR rules in BLS and ALS emergency medical services (EMS) systems (Table 1) (3-12). The BLS TOR rule suggests that resuscitative efforts may be aborted in patients whose arrest was not witnessed by EMS, in whom return of spontaneous circulation (ROSC) is not achieved in the field and when no shocks are delivered (Table 1). The ALS TOR rule can be applied when the arrest was not witnessed, when bystander CPR was not provided, when no ROSC is achieved despite ALS care in the field, and when no shocks are delivered. Recent studies demonstrated that ALS EMS providers can also use the BLS TOR rule (Table 1). This has been included as the “universal termination of resuscitation (TOR) rule” in the ERC guidelines (2). However, an ongoing debate exists whether TOR rules can be applied to victims of out-of-hospital cardiac arrests (OHCA) of both cardiac and non-cardiac etiologies.
Why is the TOR rule important? Transport of OHCA patients under CPR to an emergency department exposes paramedics and EMS physicians, as well as the public, to the risks of high-speed transportation. In addition, concerns exist about using of valuable hospital resources for non-salvageable patients.
Therefore, the question remains whether patients suffering from ongoing OHCA should be transported with CPR in progress. In a retrospective observational study of 10,704 patients with OHCA by Drennan et al. (11), 5,871 patients (55%) were transported with CPR in progress. Of these OHCA patients, 2,495 patients (43%) arrested before EMS arrival, and had not received defibrillation [automated external defibrillation (AED)] prior to EMS arrival; only 15 patients (0.6%) survived. Of the remaining 3,374 OHCA patients (57%), who had an EMS-witnessed cardiac arrest or who were resuscitated by laypersons and defibrillated using AEDs, 122 patients (3.6%) survived.
The main criticism—and a major limitation—of the study by Drennan et al. (11) as well as of another investigation by Morrison et al. (7) is that survival rates without neurological disability at 1 month, 6 months or 1 year were not reported.
In a prospective multi-center observational study (SOS Kanto 2012) of OHCA patients transported to 67 emergency hospitals between January 2012 and March 2013 in the Kanto region of Japan, the BLS and ALS TOR rules for OHCA resulting from both cardiac and non-cardiac etiologies were again validated (13). Ambulance crews included three EMS providers, with at least one emergency lifesaving technician (ELST) as the highest qualification capable of performing standard ALS interventions. EMS personnel in Japan is not allowed to terminate resuscitation in the field. Therefore, all patients were transported to a hospital. Inclusion criteria were adults (≥18 years) and nontraumatic OHCA. The primary outcome was cerebral performance category (CPC) of 1 (good performance) and 2 (moderate disability) as favorable outcome and CPC category 3–5 as unfavorable outcome when assessed at 1 month after cardiac arrest. The secondary outcome was mortality at 1 month. Out of 16,452 OHCA patients, 11,505 patients (69.9%) were included after adjusting for inclusion criteria and missing data. The main results are shown in Figure 1. Of included patients, 3.0% showed a neurologically favorable outcome with a CPC 1 or 2.
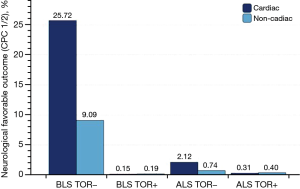
Out of 11,505 eligible cases, 6,138 patients (53.4%) suffered from cardiac and 5,367 patients (46.6%) suffered from non-cardiac etiology. BLS was performed on 2,818 (45.9%) and 2,606 patients (48.6%) with OHCA from cardiac and non-cardiac etiology, respectively. ALS was performed on 3,320 (54.1%) and 2,761 patients (51.4%) with OHCA from cardiac and non-cardiac etiology, respectively. The diagnostic accuracy of the BLS TOR rule for predicting unfavorable outcomes in patients with OHCA of cardiac etiology who received BLS included a specificity of 0.985 [95% confidence interval (CI): 0.956–0.997] and a positive predictive value (PPV) of 0.999 (95% CI: 0.996–1.000). In patients with OHCA from cardiac etiologies who received ALS, the ALS TOR rule had a specificity of 0.963 (95% CI: 0.896–0.992) and a PPV of 0.997 (95% CI: 0.991–0.999). In patients with OHCA from non-cardiac etiologies who received BLS, the specificity was 0.915 (95% CI: 0.796–0.976) and PPV was 0.998 (95% CI: 0.995–0.999). For patients with OHCA from non-cardiac etiologies who received ALS, the specificity was 0.833 (95% CI: 0.586–0.964) and PPV was 0.996 (95% CI: 0.988–0.999).
The authors concluded that both TOR rules have high specificity and PPV in patients with OHCA from cardiac etiologies. For patients with OHCA from non-cardiac etiologies, the TOR rules had a high PPV, but relatively low specificity. Therefore, based on this study, the TOR rules are useful in patients with OHCA from cardiac etiologies, but should be applied with caution to patients with OHCA from non-cardiac etiologies.
Whilst these results are of major relevance to the scientific community, several limitations exist. Most importantly, the study cohort is a selective one, excluding pediatric patients (age <18 years) and traumatic cardiac arrest (TCA). In addition, it is questionable whether the results are generalizable, as the study reports data from one particular region within Japan (Kanto area) and details of treatment provided by EMS are not reported. For example, concerns about airway management in Japanese EMS exist (14), and outcome associated with out-of-hospital OHCA resuscitation by non-physicians appears to be inferior to physician-directed CPR (15). It is also important to note that Kashiura et al. (13) did not assess the use of the BLS TOR as “universal” TOR rule in patients who received ALS measures. It is thus impossible to draw conclusions on the validity of this universal TOR rule based on this study.
Of note, 13 patients had unexpected survival despite meeting criteria based on both the BLS and the ALS TOR rule. These patients had suffered a cardiac arrest from causes such as accidental hypothermia, pulmonary embolism, drug overdose and suffocation. In five of these 13 patients, extracorporeal cardiopulmonary resuscitation (eCPR) (16) was used.
The authors suggest that end-tidal carbon dioxide (etCO2) should be included in the decision making process, as a low etCO2 may indicate a poor prognosis. However, we would caution that etCO2 levels should be interpreted in light of automated mechanical chest compression devices (ACCD) and the choice of airway device. We recently criticized that there is considerable potential for ineffective ventilation with continuous and uninterrupted mechanical chest compressions in patients ventilated via supraglottic airway devices (17). This may be particularly important for patients transported to a hospital with prolonged and ongoing CPR during transport (17). No such data are reported in the study by Kashiura et al. (13).
In conclusion, the results reported by Kashiura et al. (13) suggest that the transport of patients under CPR may be beneficial in OHCA of non-cardiac etiologies. In the study patient population, the TOR rules have relatively poor specificity for predicting a poor neurological outcome, considering the potential consequences of premature TOR in the field. However, the study’s limitations need to be considered prior to implementing this concept in any EMS system. Factors such as BLS or ALS level of care, specific ALS measures provided, paramedic or physician-directed care, regional infrastructure and risks associated with EMS transport will have a significant impact on any such decision. The availability of emerging, novel resuscitation techniques, such as eCPR, may be an important factor to consider when weighing the risks and benefits of early transport with CPR in progress (18).
Acknowledgements
None.
Footnote
Provenance: This is an invited Editorial commissioned by the Section Editor Zhongheng Zhang (Department of Critical Care Medicine, Jinhua Municipal Central Hospital, Jinhua Hospital of Zhejiang University, Jinhua, China).
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Böttiger BW. "A Time to Act"--Anaesthesiologists in resuscitation help save 200,000 lives per year worldwide: School children, lay resuscitation, telephone-CPR, IOM and more. Eur J Anaesthesiol 2015;32:825-7. [Crossref] [PubMed]
- Soar J, Nolan JP, Böttiger BW, et al. European Resuscitation Council Guidelines for Resuscitation 2015: Section 3. Adult advanced life support. Resuscitation 2015;95:100-47. [Crossref] [PubMed]
- Morrison LJ, Visentin LM, Kiss A, et al. Validation of a rule for termination of resuscitation in out-of-hospital cardiac arrest. N Engl J Med 2006;355:478-87. [Crossref] [PubMed]
- Richman PB, Vadeboncoeur TF, Chikani V, et al. Independent evaluation of an out-of-hospital termination of resuscitation (TOR) clinical decision rule. Acad Emerg Med 2008;15:517-21. [Crossref] [PubMed]
- Morrison LJ, Verbeek PR, Zhan C, et al. Validation of a universal prehospital termination of resuscitation clinical prediction rule for advanced and basic life support providers. Resuscitation 2009;80:324-8. [Crossref] [PubMed]
- Sasson C, Hegg AJ, Macy M, et al. Prehospital termination of resuscitation in cases of refractory out-of-hospital cardiac arrest. JAMA 2008;300:1432-8. [Crossref] [PubMed]
- Morrison LJ, Eby D, Veigas PV, et al. Implementation trial of the basic life support termination of resuscitation rule: reducing the transport of futile out-of-hospital cardiac arrests. Resuscitation 2014;85:486-91. [Crossref] [PubMed]
- Skrifvars MB, Vayrynen T, Kuisma M, et al. Comparison of Helsinki and European Resuscitation Council "do not attempt to resuscitate" guidelines, and a termination of resuscitation clinical prediction rule for out-of-hospital cardiac arrest patients found in asystole or pulseless electrical activity. Resuscitation 2010;81:679-84. [Crossref] [PubMed]
- Fukuda T, Ohashi N, Matsubara T, et al. Applicability of the prehospital termination of resuscitation rule in an area dense with hospitals in Tokyo: a single-center, retrospective, observational study: is the pre hospital TOR rule applicable in Tokyo? Am J Emerg Med 2014;32:144-9. [Crossref] [PubMed]
- Diskin FJ, Camp-Rogers T, Peberdy MA, et al. External validation of termination of resuscitation guidelines in the setting of intra-arrest coldsaline, mechanical CPR, and comprehensive post resuscitation care. Resuscitation 2014;85:910-4. [Crossref] [PubMed]
- Drennan IR, Lin S, Sidalak DE, et al. Survival rates in out-of-hospital cardiac arrest patients transported without prehospital return of spontaneous circulation: an observational cohort study. Resuscitation 2014;85:1488-93. [Crossref] [PubMed]
- Ong ME, Jaffey J, Stiell I, et al. Comparison of termination-of-resuscitation guidelines for basic life support: defibrillator providers in out-of-hospital cardiac arrest. Ann Emerg Med 2006;47:337-43. [Crossref] [PubMed]
- Kashiura M, Hamabe Y, Akashi A, et al. Applying the termination of resuscitation rules to out-of-hospital cardiac arrests of both cardiac and non-cardiac etiologies: a prospective cohort study. Crit Care 2016;20:49. [Crossref] [PubMed]
- Bernhard M, Becker TK, Böttiger BW. Prehospital airway management for out-of-hospital cardiac arrest. JAMA 2013;309:1888. [Crossref] [PubMed]
- Böttiger BW, Bernhard M, Knapp J, et al. Influence of EMS-physician presence on survival after out-of-hospital cardiopulmonary resuscitation: systematic review and meta-analysis. Crit Care 2016;20:4. [Crossref] [PubMed]
- Teschendorf P, Bernhard M. A bridge to life: ECPR who, when, where and why? Resuscitation 2014;85:709-10. [Crossref] [PubMed]
- Bernhard M, Hossfeld B, Kumle B, et al. Don't forget to ventilate during cardiopulmonary resuscitation with mechanical chest compression devices. Eur J Anaesthesiol 2016. [Epub ahead of print]. [Crossref] [PubMed]
- Grunau B, Reynolds J, Scheuermeyer F, et al. Relationship between Time-to-ROSC and Survival in Out-of-hospital Cardiac Arrest ECPR Candidates: When is the Best Time to Consider Transport to Hospital? Prehosp Emerg Care 2016.1-8. [Epub ahead of print]. [Crossref] [PubMed]