Complex uniportal video-assisted thoracoscopic sleeve lobectomy during live surgery broadcasting
Introduction
The impact and evolution of minimally invasive thoracic surgery has been substantial during the last decade. The uniportal VATS technique has emerged as a revolutionary approach for early stage and advanced tumors (1). A lot of experience has been acquired in order to progress from the first thoracoscopic lung resections performed in the early 90s (2) to the complex vascular and bronchial reconstruction lobectomies performed by experience surgeons nowadays (3-5). Improvements in thoracoscopic instrumentation and technology such as high definition cameras and energy devices contributed considerably in this evolution (6).
Sleeve and double sleeve lobectomies are complex procedures even when they are performed in open surgery. These procedures are preferred instead of pneumonectomies for advance stage lung cancer because they preserve lung parenchyma and avoid the morbidity associated with pneumonectomies (7,8). Since the oncologic principles are not compromised the postoperative results in term of oncologic safety should be similar, but the patient obtains the advantage of a minimally invasive procedure such as less pain, faster recovery and less hospitalization time.
In the hands of expert VATS surgeons, bronchial and vascular reconstructions can also be done safely and many groups have published their results with multiport VATS and more recently with the uniportal approach (4-6,9,10).
The case reported in this article (Figure 1) shows that even extremely complex cases that require an sleeve resection can be safely performed through uniportal VATS by an expert surgeon (Dr. Gonzalez-Rivas) during a live surgery event.
Clinical summary
A 42-year-old morbidly obese female patient (BMI 40) was diagnosed with a left upper lobe tumor (Figure 2). The patient suffered from recurrent pneumonias during the last year. The surgical case was selected for uniportal VATS live surgery during a workshop. The bronchoscopy showed an endobronchial mass in the left upper lobe bronchus involving the the main bronchus close to the carina (Figure 3A). The patient was placed in a right lateral decubitus position. A 4cm incision was made in the fifth intercostal space and dissection was performed until access to the thoracic cavity was obtained. No rib spreader was used during the surgery. The camera was placed in the posterior part of the incision and the instruments were introduced from below. Since the patient was obese, the diaphragm was highly located because of the pressure from abdominal cavity. Severe adhesions to the parietal pleura and mediastinum were found and detached. The left lower lobe was fused to the diaphragm and it was carefully detached with bimanual instrumentation and using an energy devices. After liberating the lower lobe, the fissure was handling. Identification of the interlobar plane was difficult because it was and incomplete fissure with a lot of adhesions between the lobes, so it was approach from anterior to posterior, with blunt dissection and remaining lung parenchyma in the fissure was stapled. The dissection continued with the pulmonary artery, which was technically challenging due to inflammatory changes of the tissues and also because of lymph nodes that obstruct the planes of dissection. Carefully identifying the adventitial plane of the pulmonary artery allows to safely dissecting it and dividing the first branches with a vascular endostapler. The left upper lobe vein was dissected and divided afterwards with the help of a tie to retract to avoid injury to the pulmonary artery when introducing the endostapler. Small branches of the pulmonary artery were ligated with a silk for the proximal end and divided with the energy device for the distal end. The interlobar artery was found dissecting above the junction of the inferior and superior pulmonary vein, completing the fissure stapling the lung tissue and identifying and dividing the lingular artery. Afterwards the interlobar artery was mobilized to facilitate exposure to the bronchus, which was carefully dissected. An incision was made in the base of the left upper bronchus and a circumferential cut was made with scissors to the main stem bronchus and the lower lobe bronchus. The left upper lobe was removed using an endobag. Further dissection was necessary to correctly expose the divided left main bronchus, since huge lymphadenopathies were obstructing it and will complicate the anastomosis procedure. Complete lymph node dissection was performed prior to initiating the anastomosis.
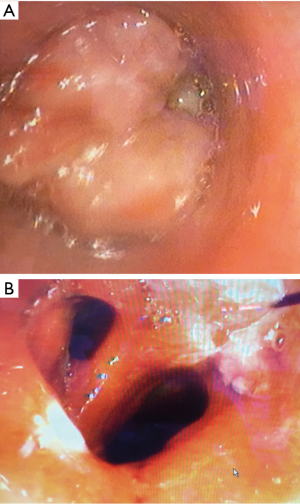
An end-to-end anastomosis was performed starting with a posterior stitch in the cartilaginous-membranous junction to help approximate the left lower and main stem bronchus. A continuous suture was initiated in the membranous portion from posterior to anterior, using a not pusher to tie the knot. Afterwards another continuous suture from posterior to anterior was done for the cartilaginous part and tie after completion with the running suture of the membranous wall. Air leak was ruled out with a water test upon insufflation. No tissue flap was used to protect the anastomosis and a single chest tube was placed through the incision. The postoperative bronchoscopy showed good caliber of the anastomosis (Figure 3B).
The postoperative course of the patient was uneventful and the patient was discharged home on the 7th postoperative day with excellent recovery. The pathological analysis showed a moderately-differentiated mucoepidermoid carcinoma with no lymph node involvement (11 adenopathies studied free of tumor).
Discussion
Indications and contraindications for VATS lobectomy have changed over time, due to increased experience in the technique. Initially VATS lobectomy was only consider for early stage lung cancer but thanks to the advances in thoracoscopic technology VATS has now a role in advance stage cases, even if they required bronchial or vascular reconstruction and it had been gaining acceptance in the thoracic community (3,9,12). The uniportal VATS technique, which is the latest step in VATS evolution, has also been used to safely perform this kind of complex cases (1,4-6).
As in any other surgical procedure, the uniportal sleeve technique has a learning curve, and it only should be attempted by expert surgeons with the uniportal VATS approach for lobectomy and the open sleeve procedures. Some authors suggest at least 200 VATS lobectomies and 20 open sleeve procedures before attempting a thoracoscopic sleeve resection (13).
Among the different sleeve lobectomies, the left side procedures are usually the more complicated ones, due to the presence of the aortic arch, the bigger size of the pulmonary artery and the absence of the intermediate bronchus (14).
Principles of single port VATS bronchoplasty are the same as in open surgery, the anastomosis has to be well vascularized, free of tension and in the left upper sleeve care must be taken to avoid injury to left recurrent laryngeal nerve during dissection and anastomosis. The preferred technique for anastomosis of the authors is a continuous suture with and absorbable 3−0 suture in two steps for the posterior and anterior wall of the bronchus, it is quicker and avoids tangling (6,14) .Usually there is no need of buttressing the anastomosis and anastomosis without coverage with tissue flap are safe (15). We only buttress the anastomosis after radiation or when there are signs of infection (14).
Currently, not many teams around the world are able to complete a uniportal VATS sleeve lobectomy, this slow adoption is because it requires advance training and experience and lacking of it rises concerns about technical issues like maintaining oncologic principles and the possibility of facing a major intraoperative bleeding (6,14).
There are very few published articles of bronchial or combined bronchovascular sleeve performed by VATS, and the vast majority are done through multiport VATS (16,17). Most of the articles published on uniportal VATS complex reconstruction belong to the team from La Coruña (4-6,14) and is that experience gained that has allowed to perform not only conventional sleeve procedures, which by themselves are challenging but to be able to successfully perform sleeve lobectomies even in extremely difficult scenarios like the case presented above. There were a number of conditions that made the surgery extremely difficult; the obesity, contributing also to a highly located diaphragm, the severely attached diaphragm to the lower lobe and the enlarged lymph nodes that were blocking the vascular structures and the bronchus (18).
Recently, tracheal and carinal uniportal VATS resections had been reported, emerging as an option to the conventional approach of a right thoracotomy or median sternotomy (14), although time will be need it before other groups obtain the necessary experience to be able to attempt such cases.
The case presented in this article shows that the limits are there to be surpassed and that the indications and capabilities of uniportal VATS continue to growth as it goes on erasing previous boundaries.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Is uniportal thoracoscopic surgery a feasible approach for advanced stages of non-small cell lung cancer? J Thorac Dis 2014;6:641-8. [PubMed]
- Roviaro G, Rebuffat C, Varoli F, et al. Videoendoscopic pulmonary lobectomy for cancer. Surg Laparosc Endosc 1992;2:244-7. [PubMed]
- Bertolaccini L, Viti A, Terzi A. Moving beyond the boundary: the emerging role of video-assisted thoracic surgery for bronchoplastic resections. J Thorac Dis 2014;6:1170-2. [PubMed]
- Gonzalez-Rivas D, Fernandez R, Fieira E, et al. Uniportal video-assisted thoracoscopic bronchial sleeve lobectomy: first report. J Thorac Cardiovasc Surg 2013;145:1676-7. [Crossref] [PubMed]
- Gonzalez-Rivas D, Delgado M, Fieira E, et al. Double sleeve uniportal video-assisted thoracoscopic lobectomy for non-small cell lung cancer. Ann Cardiothorac Surg 2014;3:E2. [PubMed]
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Uniportal video-assisted thoracoscopic sleeve lobectomy and other complex resections. J Thorac Dis 2014;6:S674-81. [PubMed]
- Maurizi G, D'Andrilli A, Anile M, et al. Sleeve lobectomy compared with pneumonectomy after induction therapy for non-small-cell lung cancer. J Thorac Oncol 2013;8:637-43. [Crossref] [PubMed]
- Howington JA, Blum MG, Chang AC, et al. Treatment of stage I and II non-small cell lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013;143:e278S-313S.
- Mahtabifard A, Fuller CB, McKenna RJ Jr. Video-assisted thoracic surgery sleeve lobectomy: a case series. Ann Thorac Surg 2008;85:S729-32. [Crossref] [PubMed]
- Li Y, Wang J. Video-assisted thoracoscopic surgery sleeve lobectomy with bronchoplasty: an improved operative technique. Eur J Cardiothorac Surg 2013;44:1108-12. [Crossref] [PubMed]
- Yang Y, Guido Guerrero W, Algitmi I, et al. Left lower lobe sleeve resection and anastomosis. Asvide 2016;3:224. Available online: http://www.asvide.com/articles/983
- Hennon M, Sahai RK, Yendamuri S, et al. Safety of thoracoscopic lobectomy in locally advanced lung cancer. Ann Surg Oncol 2011;18:3732-6. [Crossref] [PubMed]
- Gonzalez D, de la Torre M, Paradela M, et al. Video-assisted thoracic surgery lobectomy: 3-year initial experience with 200 cases. Eur J Cardiothorac Surg 2011;40:e21-8. [Crossref] [PubMed]
- Gonzalez-Rivas D, Yang Y, Sekhniaidze D, et al. Uniportal video-assisted thoracoscopic bronchoplastic and carinal sleeve procedures. J Thorac Dis 2016;8:S210-22. [PubMed]
- Storelli E, Tutic M, Kestenholz P, et al. Sleeve resections with unprotected bronchial anastomoses are safe even after neoadjuvant therapy. Eur J Cardiothorac Surg 2012;42:77-81. [Crossref] [PubMed]
- Han Y, Zhou S, Yu D, et al. Video-assisted thoracic surgery (VATS) left upper sleeve lobectomy with partial pulmonary artery resection. J Thorac Dis 2013;5 Suppl 3:S301-3. [PubMed]
- Liu L, Mei J, Pu Q, et al. Thoracoscopic bronchovascular double sleeve lobectomy for non-small-cell lung cancer. Eur J Cardiothorac Surg 2014;46:493-5. [Crossref] [PubMed]
- Guido Guerrero W, Gonzalez-Rivas D, Hernandez Arenas LA, et al. Techniques and difficulties dealing with hilar and interlobar benign lymphadenopathy in uniportal VATS. J Vis Surg 2016;2:23.



