Experience and outcomes for relatives of patients dying in the ICU: the CAESAR tool
‘Make me acquainted with your grief’——W. Shakespeare (Julius Caesar, Act 2, Scene 1)
The death of a loved one is recognized as one of life’s most challenging and stressful experiences (1). This is especially the case where the death is not anticipated, involves a catastrophic event or is perceived as involving significant suffering (2). These factors are often present when death occurs within the intensive care unit (ICU), when admission can be sudden and unexpected. Overall hospital mortality for patients admitted to the ICU is reported as just over 11% (3), but may be many times higher when admission is unplanned (4). Critical care specialists are increasingly aware that in circumstances where a patient’s life cannot be saved, there is an ethical and professional responsibility to ensure that the patient and their loved ones experience the ‘best death’ that is possible (5). The focus of patient care shifts from the provision of artificial life supporting therapies to a prioritization of the patient’s comfort, dignity and adherence to any previously expressed preferences or choices.
During the dying process, support for a patient’s relatives is crucial. However, despite the known risk of prolonged psychological problems for the bereaved, it is difficult to predict who will be most affected and unclear how to reduce these problems. Psychological distress experienced by relatives of a dying patient includes depression, anxiety, post-traumatic stress disorder (PTSD), sleep disruption and complicated grief (6,7). Up to 70% of family members may experience some or all of these issues (8-10). While many of these manifestations may be attributable to bereavement, the characteristics of ICU-related deaths may have an additional impact. Intensive Care may be perceived as dehumanizing and violate the personhood of the individual (11). Further understanding the magnitude of this problem is necessary for the development and study of potential interventions for family care. Several studies have examined factors that may impact on the experience of families (12,13). However, tools that may be easily and reproducibly incorporated into routine practice are lacking.
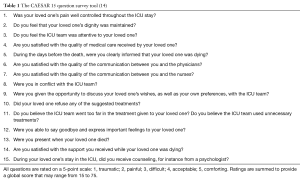
Findings from the recently published CAESAR study (14) may assist clinicians and researchers in developing better strategies to assist the relatives of dying ICU patients. This large, prospective study evaluated the perspectives of relatives of dying patients in the ICU. Extensive work was done to establish a simple tool with which to assess the experience of relatives of the dying, which was then correlated with subsequent psychological distress. Drawing on existing evidence, local experience and extensive qualitative interviews, the investigators identified fifty items relating to the experience of relatives across eight domains. After testing in a single ICU, the number of items was reduced to thirty-three, spread across three domains: (I) communication issues (especially in the setting of conflict); (II) family needs and (III) satisfaction. This survey was subsequently prospectively evaluated over 2 years in forty-one French ICUs. Consecutive deaths of patients who spent at least 48 hours in the ICU were included, with the key surrogate decision maker identified (in order) as legal proxy, spouse, adult offspring, sibling or other relative. Relatives completed the survey by telephone 3 weeks after their relative’s death and then 9 weeks later went on to complete both the Hospital Anxiety Depression Score (HADS) and the Impact of Event Scale-Revised (IES-R) for PTSD. Six and twelve months after the death of their loved one, relatives were sent a further questionnaire that included the Inventory of Complicated Grief (ICG) and IES-R by mail. Further refinement of the survey was achieved after statistical analysis led to the elimination of eighteen redundant questions. The resultant fifteen-question tool (Table 1) allows individual item scores of 1 to 5 that are summed to obtain a global score of 15 to 75.
Amongst the 4,607 patients admitted to the forty-one ICUs during the study period, 19% (875 individuals) died in the ICU. However, only half of these episodes (475 deaths) were included in the study due to exclusion criteria [228], missed enrolment [104] and refusal of consent by relatives [68]. Remarkably, at 3 weeks, the 33-item questionnaire was completed by over 90% of relatives, with almost all including a response to every question. As a result, non-responder bias amongst participants was minimal. Factors associated with a lower CAESER score included longer ICU length of stay and use of vasopressor therapies, which may be surrogates for a difficult experience of critical illness in a more unwell patient.
Eighty-six percent of relatives completed the HADS and IES-R at 12 weeks, with over half exhibiting symptoms of depression and over a third of them exhibiting symptoms of anxiety. Complicated grief was evident in just over half of all relatives at 26 months. In the lowest quartile of CAESER score relatives, complicated grief was evident in nearly three quarters of respondents at 6 months and nearly two thirds of respondents at 12 months. PTSD symptoms were evident in approximately 40% of relatives with the number decreasing slightly over the period from 3 to 12 months.Once again, relatives with CAESAR scores in the lowest quartile exhibited the greatest burden of PTSD symptoms, with 60% of respondents impacted, falling to 55% and 47% at 6 and 12 months respectively. A separate group of 125 patient relatives were drawn from 232 deaths in 15 ICUs for the purpose of providing a validation cohort. Similar numbers of patients were excluded based on not meeting inclusion criteria, being missed for inclusion or having relatives that refused to consent being in the study. More than 90% of eligible relatives in the validation cohort completed the telephone questionnaire at three weeks. This validation sample was utilized to evaluate factorial validity of both the 33-item questionnaire and the final 15-item CAESAR questionnaire.
The CAESAR questionnaire seems to be feasible to administer, with a reported time taken to complete of around twenty minutes. By minimizing the number of questions, using precise language (i.e., avoiding leading questions and confusing modifiers), and measuring agreement in a quantifiable format, the investigators have created a tool that maximizes reliability and validity (15). The high response rate suggests that grieving relatives find the format acceptable and are prepared to participate. Low scores at three weeks correlated strongly with self-reported symptoms of anxiety, depression, PTSD and complicated grief. It therefore shows potential as a means of readily quantifying risk for psychological problems in relatives of patients who die in the ICU. However, whether these findings can be replicated in non-French clinical settings needs to be evaluated in order to establish the generalizability of this approach.
As well as developing a relatively simple tool to predict the burden of psychological symptoms in relatives of non-surviving ICU patients, the CAESAR investigators identified several features of end-of-life care that correlate with subsequent PTSD and complicated grief. These included the relative’s perceptions of adequacy of pain control, maintenance of patient’s dignity, family presence during dying and the exploration of patient’s preferences. Additionally, the perceived quality of communication was amongst the most highly rated elements of ICU end of life care. These domains could be further studied and might form the basis of benchmarking between ICUs. They may also be the focus of further interventional studies to improve the experience of dying and reduce the burden of psychological distress among relatives.
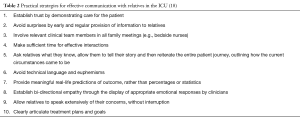
Importantly, communication was identified as an essential and potentially modifiable factor associated with the experience of dying (16,17). For relatives to accept medical recommendations such as to withdraw or withhold non-beneficial treatment is extremely difficult and can only occur when a strong bond of trust in the treating clinicians can be established. This requires intensive care specialists to demonstrate kindness, empathy and clinical competence, combined with high-level communication skills. Key strategies for effective communication with relatives in the ICU are summarized in Table 2 (18). These approaches are even more important in settings of conflict or distress, which are more likely to occur when an ICU patient is dying.
Several other strategies for improving the experience of relatives of dying patients in the ICU include the optimization of pain control and effective management of distressing symptoms. Ensuring that care and attention is directed to respecting the dignity of the dying patient with specific efforts to incorporate their known wishes, beliefs, preferences and goals is likely to diminish the potential for long-term psychological injury to their relatives (19). While goals change and treatments may be withdrawn or withheld, care continues throughout the dying process and relatives should be supported to maintain involvement in a manner that that suits their individual circumstances. The transition from active, cure-directed treatment to palliative measures based on optimal control of symptoms needs to be carefully forecast, explained, justified and implemented with sensitivity and compassion by intensive care clinicians in order to minimize distress. The CAESAR tool may provide a relatively simple and effective measure of how such aspects of practice impact on relatives and as such could prove extremely useful in the design and evaluation of interventions to reduce the long-term negative impact of losing a loved one in the ICU.
Acknowledgements
None.
Footnote
Provenance: This is an invited Commentary commissioned by the Section Editor Zhongheng Zhang (Department of Critical Care Medicine, Jinhua Municipal Central Hospital, Jinhua Hospital of Zhejiang University, Jinhua, China).
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Holmes TH, Rahe RH. The Social Readjustment Rating Scale. J Psychosom Res 1967;11:213-8. [Crossref] [PubMed]
- Shear MK. Clinical practice. Complicated grief. N Engl J Med 2015;372:153-60. [Crossref] [PubMed]
- Zimmerman JE, Kramer AA, Knaus WA. Changes in hospital mortality for United States intensive care unit admissions from 1988 to 2012. Crit Care 2013;17:R81. [Crossref] [PubMed]
- Exploring unplanned ICU admissions: a systematic review. 2011. Available online: .http://joannabriggslibrary.org/index.php/jbisrir/article/view/147
- Nelson JE. Saving lives and saving deaths. Ann Intern Med 1999;130:776-7. [Crossref] [PubMed]
- Davidson JE, Jones C, Bienvenu OJ. Family response to critical illness: postintensive care syndrome-family. Crit Care Med 2012;40:618-24. [Crossref] [PubMed]
- Siegel MD, Hayes E, Vanderwerker LC, et al. Psychiatric illness in the next of kin of patients who die in the intensive care unit. Crit Care Med 2008;36:1722-8. [Crossref] [PubMed]
- Verceles AC, Corwin DS, Afshar M, et al. Half of the family members of critically ill patients experience excessive daytime sleepiness. Intensive Care Med 2014;40:1124-31. [Crossref] [PubMed]
- Pochard F, Azoulay E, Chevret S, et al. Symptoms of anxiety and depression in family members of intensive care unit patients: ethical hypothesis regarding decision-making capacity. Crit Care Med 2001;29:1893-7. [Crossref] [PubMed]
- Pochard F, Darmon M, Fassier T, et al. Symptoms of anxiety and depression in family members of intensive care unit patients before discharge or death. A prospective multicenter study. J Crit Care 2005;20:90-6. [Crossref] [PubMed]
- Kelleher S. Providing patient-centred care in an intensive care unit. Nurs Stand 2006;21:35-40. [Crossref] [PubMed]
- Azoulay E, Pochard F, Kentish-Barnes N, et al. Risk of post-traumatic stress symptoms in family members of intensive care unit patients. Am J Respir Crit Care Med 2005;171:987-94. [Crossref] [PubMed]
- Haines KJ, Denehy L, Skinner EH, et al. Psychosocial outcomes in informal caregivers of the critically ill: a systematic review. Crit Care Med 2015;43:1112-20. [Crossref] [PubMed]
- Kentish-Barnes N, Seegers V, Legriel S, et al. CAESAR: a new tool to assess relatives' experience of dying and death in the ICU. Intensive Care Med 2016;42:995-1002. [Crossref] [PubMed]
- Jones D, Story D, Clavisi O, et al. An introductory guide to survey research in anaesthesia. Anaesth Intensive Care 2006;34:245-53. [PubMed]
- Warrillow S, Farley KJ, Jones D. How to improve communication quality with patients and relatives in the ICU. Minerva Anestesiol 2016. [Epub ahead of print]. [PubMed]
- Lautrette A, Darmon M, Megarbane B, et al. A communication strategy and brochure for relatives of patients dying in the ICU. N Engl J Med 2007;356:469-78. [Crossref] [PubMed]
- Warrillow S, Farley KJ, Jones D, et al. Ten practical strategies for effective communication with relatives of ICU patients. Intensive Care Med 2015;41:2173-6. [Crossref] [PubMed]
- Detering KM, Hancock AD, Reade MC, et al. The impact of advance care planning on end of life care in elderly patients: randomised controlled trial. BMJ 2010;340:c1345. [Crossref] [PubMed]