Preoperative evaluation of stage T3, central-type non-small cell lung cancer with double sleeve lobectomy under complete video-assisted thoracoscopic surgery using spiral computed tomography post-processing techniques
Introduction
In central-type lung cancers, the large blood vessels, trachea, or bronchi adjacent to the hilum of the lung are typically prone to tumour invasion. Hence, accurate evaluation of the range of tumour invasion and extent of involvement of blood vessels and bronchi are important criteria that help a surgeon decide the need and method for surgery and subsequent postoperative evaluation. Routine cross-sectional, chest computed tomography (CT) is the most commonly used imaging technique to diagnose chest diseases. In recent years, with spiral CT post-processing software development and application, post-processing techniques had been widely used in clinical diagnosis, such as multiplanar reformation (MPR), maximum intensity projection (MIP), minimum intensity projection (MinIP), and volume rendering (VR). These techniques are comprehensive and allow multidirectional and stereo imaging; they are also more accurate than the routine CT used to evaluate the relationship between lesions and surrounding tissues or organs. However, their application in non-small cell lung cancer (NSCLC) has only been rarely reported (1).
Double sleeve (vascular and bronchial) lobectomy with complete video-assisted thoracoscopic surgery (c-VATS) is a new surgical method in recent years for treatment of central-type lung cancer (2-4). However, it is a challenging and complex procedure even when performed through thoracotomy (2). There are few cross-sectional CT reports regarding double sleeve lobectomy with c-VATS of central-type lung cancer (2-4). Since June 2012, 10 patients with stage T3, central-type NSCLC were treated with double sleeve lobectomy via c-VATS and showed good outcomes in our hospital. In this study, we explored the comparison between surgical pathological results and the preoperative estimated value of spiral CT post-processing techniques in these 10 patients.
Methods
Patient population
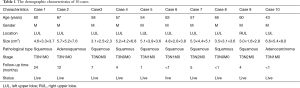
From June 2012 to June 2014, 10 patients with stage T3, central-type NSCLC underwent c-VATS with double sleeve lobectomy at our institution; their medical records were retrospectively analysed. All patients were men aged between 43 and 67 years (mean age, 59.1±7.0 years). In nine cases, the tumour was located on the left upper lobe of the lung, and in one case, it was located in the right upper lobe. Further, eight cases were squamous cell carcinomas, one case was an adenocarcinoma, and another one was a foetal adenocarcinoma. Three cases were staged as IIB and seven, as IIIA. Follow-up period ranged from 1 to 24 months; all 10 patients are presently alive (Table 1). This retrospective study was approved by our institutional review board, which waived informed consent.
Full table
Spiral CT examination
The Siemens SOMATOM Definition AS sensation 128 spiral CT scanner (Germany) was used for measurements. The scanning range was from superior aperture of the thorax to both sides of the diaphragm, where the costophrenic angle disappeared. During scanning, patients maintained a supine position while holding their breath at full inspiration. The scan parameters were as follows: tube voltage, 120 kV; automatic modulation of tube current; matrix size, 512×512; pitch, 1.0; collected thickness, 1-mm. The enhanced contrast agent was non-ion type at a concentration of 300 mgI/mL. The antecubital vein was injected using a pressure syringe at the rate of 4 mL/s, and the intravenous injection dose was 1.2 mL/kg. The pulmonary arterial phase scan began 12 s after contrast-agent injection; the area from the superior aortic arch to the distal tip of the heart was scanned. The aortic phase scan began 25 s after contrast-agent injection; the area from the 5th cervical vertebra to the 2nd lumbar vertebra was scanned. The total scanning radiation dose of plain and enhanced scan was about 5.1–6.2 mSv. Radiation dose of CT post-processing techniques does not increase, but the examination cost increases about $75 compared with traditional CT scan.
Imaging post-processing techniques
Images were processed with the syngo MMWP VE36A independent workstation. In pulmonary arterial phase images, multiplanar reconstruction (MPR), MIP and VR techniques were used to reconstruct images of the pulmonary artery trunk and upper lobe pulmonary artery. MPR, MinIP, and VR techniques were used to reconstruct 2-dimensional or 3-dimensional images of the bronchi in the aortic phase images. The standard plane of the bronchi was the coronal plane passing through the central axis of the bronchi.
CT images evaluation
Evaluation criteria of pulmonary artery with tumour invasion (5)
Vessel integrity on cross-sectional helical studies and combined CT angiography and three dimensional reconstruction technology studies were assessed on a 5-grade scale: grade 0, normal, with a fat plane between the tumour and the vessel; grade 1, loss of fat plane between the tumour and the vessel, encased vessel with tumour extending less than one half of the perimeter; grade 2, encased vessel with tumour extending equal to or more than one half of the perimeter, but less than two thirds of the perimeter, with or without smooth displacement of the vessel, flattening or slight irregularity of one side of the vessel; grade 3, encased vessel with tumour extending equal to or more than two thirds of the perimeter, altering its contour and producing concentric or eccentric narrowing of the lumen; grade 4, occluded vessel or vascular lumen with filling defect. Involvement of the pulmonary artery and vein were graded on this scale.
Evaluation criterion of the bronchi with tumour invasion (6)
Grade 0 (non-invasion), smooth and non-thickening luminal wall, no luminal stenosis; grade 1 (suspicious invasion), luminal wall was pressed with or without smooth displacement of the bronchus and thickened but smooth luminal wall without stenosis; grade 2 (mild invasion), mild luminal stenosis (degree of stenosis, ≤25%); grade 3 (moderate invasion), moderate luminal stenosis (degree of stenosis, 25–75%); and grade 4 (severe invasion), severe luminal stenosis (degree of stenosis, ≥75% or bronchial occlusion.
Confirmation of the evaluated object
In pulmonary artery evaluation, we included both sides of the arterial trunk and the segmental artery of both upper lungs. In the evaluation of bronchi, we included bronchi and segmental bronchi of both upper lobes, right and left main bronchi.
Results evaluation
Two experienced imaging radiologists were responsible for analysis of transaxial CT and post-processing images. Results regarding the morphology, sizes, density, margins, and pulmonary vascular or tracheal bronchial tree involvement from lung cancer were analysed. In case of any disagreement, detailed discussions were held to reach consensus.
Results
In total, we assessed both the left and right main pulmonary arteries, 40 branches of segmental arteries of both upper lobes, as well as 40 branches of bronchi. In all 10 cases, the trachea and the left and right main bronchus showed no tumour involvement, and the bronchi stump did not show presence of tumour tissue, as per surgical pathological reports.
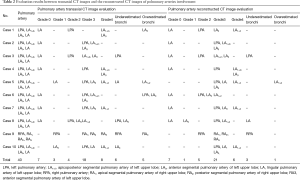
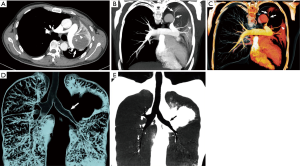
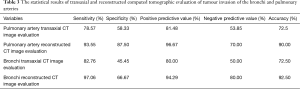
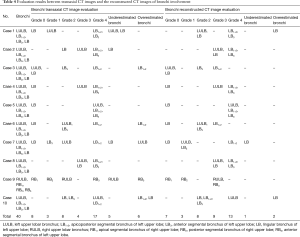
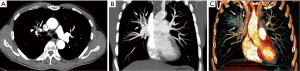
For tumour invasion of pulmonary artery (Table 2), cross-sectional CT images (Figure 1A) were evaluated, which included 7, 3, 4, 18, and 8 branches of pulmonary arteries from grade 0 to grade 4, respectively. Similarly for CT reconstructed images (Figure 1B-E), we evaluated 7, 1, 5, 21, and 6 branches of pulmonary arteries from grade 0 to grade 4, respectively. According to surgical pathological results, cross-sectional CT images were consistent with the results in 29 branches, underestimated in 6, and overestimated in 5. The sensitivity, specificity, positive predictive value, and negative predictive value were 78.57%, 58.33%, 81.48%, and 53.85%, respectively; the accurate rate of diagnosis was 72.50%. Further, CT reconstructed images were consistent with surgical results in 36 branches, underestimated in three, and overestimated in one. The sensitivity, specificity, positive predictive value, and negative predictive value were 93.55%, 87.50%, 96.67%, and 70.00%, respectively; the accurate rate of diagnosis was 90.00% (Table 3). Evaluated results between cross-sectional CT images and the reconstructed CT images were statistically analysed using the chi-square test, which showed a significant difference (χ2=4.021, P=0.045).
Full table
Full table
For the bronchial tumour invasion (Table 4), cross-sectional CT images (Figure 2A) that included 8, 3, 8, 4, and 17 branchial branches from grade 0 to grade 4, respectively. Similarly for CT reconstructed images (Figure 2B,C), we evaluated 7, 3, 8, 9, and 13 bronchial branches from grade 0 to grade 4, respectively. According to surgical pathological results, cross-sectional CT images were consistent with the results in 29 branches, underestimated in 5, and overestimated in 6. The sensitivity, specificity, positive predictive value, and negative predictive value were 82.76%, 45.45%, 80.00%, and 50.00%, respectively; the accurate rate of diagnosis was 72.50%. Further, CT reconstructed images were consistent with surgical results in 37 branches, underestimated in 1, and overestimated in 2. The sensitivity, specificity, positive predictive value, and negative predictive value were 97.06%, 66.67%, 94.29%, and 80.00%, respectively; the accurate rate of diagnosis was 92.50% (Table 4). Evaluated results between cross-sectional CT images and the reconstructed CT images were statistically analysed using the Chi-square test, which showed a significant difference (χ2=5.541, P=0.019).
Full table
Discussion
The location, range, and extent of tumour invasion of the pulmonary artery, trachea, and bronchus in central-type lung cancer have a huge influence on the removal rate, surgical method, and degree of difficulty in lung cancer surgery. In recent years, the technology of pulmonary resection has been improved, and double sleeve lobectomy has been increasingly used (2-4). Pulmonary artery and bronchial sleeve lobectomy are mainly used in central-type NSCLC. In this procedure, the lung tissue without tumour invasion can be retained, thereby preserving more than 25–35% of pulmonary function for postoperative patients and significantly improving their quality of life (7). The c-VATS double sleeve lobectomy is more difficult than double sleeve lobectomy via conventional thoracotomy, because it requires additional surgical skill for performing c-VATS. In fact, to date there are very few reported cases of double sleeve lobectomy by c-VATS (2-4,8). In addition, the surgeon needs to obtain accurate information of the relationship between the tumour and central pulmonary vessels, trachea, and bronchi before surgery, in order to choose the optimal treatment plan and preoperative preparation.
Spiral CT post-processing techniques have developed rapidly in recent years. MPR is simple and fast and can reconstruct images in any plane and direction (9). Reconstruction of images in the coronal, sagittal, and cross-sectional planes can clearly show the length and range of tumour invasion into the blood vessels, trachea, and bronchi (10,11), providing the basis for doctors to develop suitable surgical plans. However, as blood vessels are very tortuous, MPR cannot very effectively display the vascular major axial. In this regard, MIP is a very important blood-vessel imaging technique, which can show the full view of pulmonary vessels and the diameter and behaviour of the central pulmonary vessels. It can also be used to measure the diameter and cross-sectional area of the pulmonary artery. Similarly, MinIP has obvious advantages in the display of airway lesions (12). VR can be applied to three dimensional volume cutting imaging of the spatial structure in any thickness, and to some extent, it can avoid the overlap. VR is a very valuable tool to visualize the running course and anatomic distribution of large vessels, trachea, and bronchi at the lung hilum (10). In addition, VR can also function in arbitrary angle and direction rotation, and the reconstructed three dimensional images can be played continuously with VR. It is conducive to accurately determine the source and destination of the pulmonary artery, trachea, and bronchi.
In this study, we evaluated the relationship between stage T3, central-type NSCLC and blood vessels and bronchi based on five grades. We observed that for tumour invasion in the pulmonary artery, six branches in the cross-sectional CT images were underestimated, while three in the reconstructed images were underestimated; further, five were overestimated, and one was overestimated. This was mainly because the cross-sectional CT images can only reflect the anterior-posterior positional relationship between tumour tissue and blood vessels. It was difficult to display the relationship of superior and inferior positions. It cannot accurately analyse the relationship between the blood vessels of oblique line and curved line with the tumour and the extent of tumour invasion.
For evaluation extent of the invaded bronchi, five branches in cross-sectional CT images were underestimated, while two branches in reconstructed images were underestimated. Because on cross-sectional CT images, it was difficult to accurately judge the lesion’s invasive range, thereby causing misdiagnosis or missed diagnosis. Six branches were overvalued and one was overvalued. This was mainly because the view from cross-sectional CT images was limited. The cross-sectional CT images may provide limited information in displaying the spatial relationship between the tumour and bronchus (13-16), while CT reconstructed images can be clearer in comparison.
With respect to evaluation of extent of the invaded pulmonary artery, we observed that the specificity and accuracy of diagnosis increased by 29.17% and 17.50%, respectively, in the CT reconstruction post-processing technique. Similarly, in the evaluation of extent of the invaded bronchi, we observed that the specificity and accuracy of diagnosis increased by 21.22% and 20%, respectively, in the post-processing technique. Therefore, the preoperative evaluation of extent of central-type lung cancer invasion on the adjacent pulmonary vessels and bronchi by spiral CT post-processing technique showed that the diagnostic accuracy of CT post-processing images was significantly higher than that of conventional cross-sectional CT images through comparing with surgical pathological results.
In this study, cross-sectional CT images and multiple imaging post-processing techniques were used to analyse and evaluate the extent of tumour invasion to the pulmonary artery and bronchus. The MPR, MIP, and VR techniques were used in blood-vessel images reconstructions of the pulmonary trunk, apical, posterior, and anterior segmental artery of the upper lobe, while the MinIP and VR techniques were used in image reconstructions of the lobar and segmental bronchi. The results indicate that CT post-processing techniques and surgical pathological findings showed consistent and high diagnostic rates, which can likely compensate for the limitations of routine cross-sectional CT.
The small sample size is a limitation because of the complex surgery in this study. However, although there were only 10 patients with complete preoperative clinical and imaging data, we have been able to successfully apply the c-VATS-assisted double sleeve lobectomy in our institution during the past 2 years. We intend to study more cases in the future and summarize the findings in a larger sample size.
In conclusion, spiral CT post-processing techniques can accurately evaluate the situation of central-type lung cancer invasion of adjacent pulmonary blood vessels and bronchi, which is conducive to clinical staging, treatment decisions, and prognostic assessment.
Acknowledgements
Funding: The research was supported by Open Project of State Key Laboratory of Respiratory Disease (SKLRD2016OP011) and Science and Technology Planning Project of Guangdong Province (Grant No. 2014A020212340).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This retrospective study was approved by our institutional review board, which waived informed consent.
References
- Bai H, Miao J, He Z, et al. The application of spiral CT angiography in cancerous invasion of central pulmonary artery in lung cancer. Zhongguo Fei Ai Za Zhi 2000;3:445-8. [PubMed]
- Gonzalez-Rivas D, Delgado M, Fieira E, et al. Double sleeve uniportal video-assisted thoracoscopic lobectomy for non-small cell lung cancer. Ann Cardiothorac Surg 2014;3:E2. [PubMed]
- Liu L, Mei J, Pu Q, et al. Thoracoscopic bronchovascular double sleeve lobectomy for non-small-cell lung cancer. Eur J Cardiothorac Surg 2014;46:493-5. [Crossref] [PubMed]
- Huang J, Li J, Qiu Y, et al. Thoracoscopic double sleeve lobectomy in 13 patients: a series report from multi-centers. J Thorac Dis 2015;7:834-42. [PubMed]
- Raptopoulos V, Steer ML, Sheiman RG, et al. The use of helical CT and CT angiography to predict vascular involvement from pancreatic cancer: correlation with findings at surgery. AJR Am J Roentgenol 1997;168:971-7. [Crossref] [PubMed]
- Iwasaki Y. Large cell carcinoma. Nihon Rinsho 2000;58:1127-31. [PubMed]
- Ferguson MK, Landreneau RJ, Hazelrigg SR, et al. Long-term outcome after resection for bronchial carcinoid tumors. Eur J Cardiothorac Surg 2000;18:156-61. [Crossref] [PubMed]
- Gonzalez-Rivas D, Fieira E, de la Torre M, et al. Bronchovascular right upper lobe reconstruction by uniportal video-assisted thoracoscopic surgery. J Thorac Dis 2014;6:861-3. [PubMed]
- Quint LE, Whyte RI, Kazerooni EA, et al. Stenosis of the central airways: evaluation by using helical CT with multiplanar reconstructions. Radiology 1995;194:871-7. [Crossref] [PubMed]
- Newmark GM, Conces DJ Jr, Kopecky KK. Spiral CT evaluation of the trachea and bronchi. J Comput Assist Tomogr 1994;18:552-4. [Crossref] [PubMed]
- Lacrosse M, Trigaux JP, Van Beers BE, et al. 3D spiral CT of the tracheobronchial tree. J Comput Assist Tomogr 1995;19:341-7. [Crossref] [PubMed]
- Boiselle PM, Reynolds KF, Ernst A. Multiplanar and three-dimensional imaging of the central airways with multidetector CT. AJR Am J Roentgenol 2002;179:301-8. [Crossref] [PubMed]
- Makita O, Yamashita Y, Arakawa A, et al. Diffuse perfusion abnormality of the liver parenchyma on angiography-assisted helical CT in relation to cirrhosis and previous treatments: a potential diagnostic pitfall for detecting hepatocellular carcinoma. Clin Imaging 2000;24:292-7. [Crossref] [PubMed]
- Yamasaki T, Kurokawa F, Shirahashi H, et al. Percutaneous radiofrequency ablation therapy with combined angiography and computed tomography assistance for patients with hepatocellular carcinoma. Cancer 2001;91:1342-8. [Crossref] [PubMed]
- Ofer A, Nitecki SS, Braun J, et al. CT angiography of the carotid arteries in trauma to the neck. Eur J Vasc Endovasc Surg 2001;21:401-7. [Crossref] [PubMed]
- Tins B, Oxtoby J, Patel S. Comparison of CT angiography with conventional arterial angiography in aortoiliac occlusive disease. Br J Radiol 2001;74:219-25. [Crossref] [PubMed]


