Veno-arterial extracorporeal membrane oxygenation for cardiogenic shock due to myocarditis in adult patients
Introduction
Myocarditis is defined as an inflammatory disease of the heart muscle whose diagnosis should fulfill established histological, immunological and immunohistochemical criteria (1). Different triggers could be advocated as possible etiologies of myocarditis: viral and non-viral infections, medications, systemic autoimmune diseases and toxic reactions (2). The spectrum of clinical presentations of myocarditis is broad and varies from subclinical asymptomatic courses to refractory cardiogenic shock (3). The prognosis of patients with myocarditis depends mainly on the severity of clinical presentation. In particular, myocarditis patients developing cardiogenic shock refractory to optimal maximal medical treatment may benefit from the use of veno-arterial extracorporeal membrane oxygenation (VA-ECMO) as a temporary mechanical circulatory support (MCS). The aim of the present report is to offer a descriptive review of the most important articles of the literature showing the results of VA-ECMO in the specific setting of cardiogenic shock due to myocarditis in adult patients.
A paradigm shift
Cardiogenic shock is a life-threatening condition characterized by tissue hypoperfusion and multiorgan failure requiring prompt interventions. Initially refractory cardiogenic shock is supported with temporary MCS as a “bridge to decision” before considering the patient eligible for a long-term device implantation in case of no recovery. This general trend has been regularly highlighted by the Annual Reports of the Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS) (4,5). The implantation of long-term MCS in cardiogenic shock patients, i.e., INTERMACS Level 1 patients, fell since 2006 from 41% to 14%. As a consequence, there has been a considerable increase from 8% to 30% in the implantation of long-term MCS in INTERMACS Level 3 patients, i.e., stable but inotrope-dependent heart failure patients. In this subgroup of critically ill and unstable patients in cardiogenic shock, VA-ECMO allows, on the one hand, temporary hemodynamic stabilization with improvement of end-organ function and, on the other hand, gives the time to perform complementary diagnostic exams and to decide the therapeutic strategy in these high-risk candidates for immediate long-term MCS implantation (6). VA-ECMO could be implanted and removed directly at the bedside in the intensive care unit and offers a reasonable solution in term of cost-effectiveness.
Patients who do not show myocardial recovery during VA-ECMO support could be directed to long-term ventricular assist device implantation or heart transplantation depending on age, general clinical and functional status, life expectancy and organs function (brain, lung, liver and kidneys). Finally, as stated by the European Society of Cardiology guidelines for the diagnosis and treatment of acute and chronic heart failure, short-term MCS should be considered (as a “bridge to recovery”) in patients remaining severely hypoperfused despite inotropic therapy and with a potentially reversible cause (e.g., viral myocarditis) or a potentially surgically correctable cause (7).
In a landmark report published in 2005 Chen and coworkers described their results with VA-ECMO for fulminant myocarditis-induced cardiogenic shock (8). The use of VA-ECMO offered an overall survival to hospital discharge of 73% in a cohort of 15 patients. These results were quite better as compared to a previous experience with an external pulsatile ventricular assist device. In this international registry encompassing 11 patients, 7 (63%) of them survived to the explantation of the device without heart transplantation (9). Although previous investigators already emphasized on the clinical usefulness of VA-ECMO (10-12), the study of Chen et al. was the first report clearly outlining the advantage of ECMO over ventricular assist devices in the specific setting of cardiogenic shock, i.e., the possibility to provide a biventricular support of easy and rapid setup even in emergent cardiopulmonary resuscitation situations. Long-term left ventricular or biventricular assist device implantation is a more complicated, time-consuming and much more expensive and invasive operation. Moreover, the evaluation of myocardial recovery in patients supported with long-term MCS is somewhat complicated and the final decision to wean off is in some cases a dangerous challenge. These authors showed to the scientific community the theoretical principles and the practical applications to consider VA-ECMO as the first-line MCS for myocarditis patients in cardiogenic shock refractory to standard maximal medical treatment.
Single-centre experiences
The initial experience of Chen and colleagues opened the way to several other reports confirming the role of VA-ECMO as a valuable and effective treatment option in myocarditis-induced refractory cardiogenic shock. Table 1 resumes the results of the most representative published studies of the literature reporting the use of VA-ECMO for cardiogenic shock due to myocarditis in single-centre adult experiences.
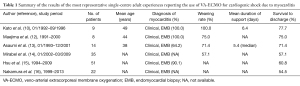
Full table
Asaumi and coworkers focused on the survival and clinical outcome of fulminant myocarditis patients (defined as those who require VA-ECMO for cardiogenic shock and do not respond to intensive medical treatments, like high doses of intravenous catecholamines or for refractory ventricular tachyarrhythmia; n=14) and compared them with those of patients with acute non-fulminant myocarditis (defined as those who had an acute onset of symptoms but did not have compromised haemodynamic following conventional medical treatment; n=13) (13). The authors demonstrated that approximately 70% of patients with fulminant myocarditis supported by percutaneous VA-ECMO could be rescued. Any patient died in the non-fulminant myocarditis group neither in the acute phase nor in the chronic phase.
The “Pitié-Salpêtrière” Hospital group published in 2009 the first comparative study between VA-ECMO (n=6) and biventricular assist device (n=5) in fulminant myocarditis patients (17). They found the same survival rate in both groups (83.3% vs. 80%, respectively) but ECMO implantation was associated with a significantly lower rate of red blood cells transfusions. Moreover the duration of support, infectious complications rate and renal and hepatic dysfunctions tended to be less important in the ECMO group. Other appealing advantages of ECMO support are the possibility of local anesthesia for implantation and removal and implantation outside of a cardiac surgery centre with safe secondary transfer. Two years later the same group described the short- and long-term outcomes of 41 patients with fulminant myocarditis rescued with MCS (14). Among their patients’ population, the first 6 patients of the series were supported with a biventricular assist device while the following 35 patients received a VA-ECMO. In the VA-ECMO group, 24 (68.5%) patients survived to hospital discharge but heart transplantation free-survival was 57.1% (n=20).
Finally, Chen and colleagues updated in 2011 the results of their single-centre experience of VA-ECMO support for acute fulminant myocarditis (15). To the best of our knowledge it is the largest adult single-centre experience encompassing 75 patients (51 adult and 24 pediatric patients). The survival rate was 60.8% for adult patients and 70.8% for pediatric patients but the difference between adult and pediatric group was not statistically significant.
Multi-centre experiences
Table 2 summarizes the results of the most representative published studies of the literature reporting the use of VA-ECMO for cardiogenic shock due to myocarditis in multi-centre adult experiences.
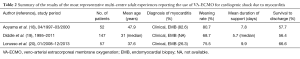
Full table
The scientific committee of the Japanese Circulation Society published in 2002 a national survey gathering information on patients with fulminant myocarditis who were treated with VA-ECMO during a 3-year period (18). Fifty-two patients were enrolled in the survey and, among them, 30 (57.7%) patients survived and returned to normal life. Moreover, the investigators performed several comparisons between different subgroups of patients in order to identify possible prognostic factors. Patients who could not be weaned off VA-ECMO and subsequently died displayed more severe myocardial damage and experienced more frequently complications associated with ECMO, especially lower limb ischemia and multiple organ failure.
Diddle et al. published in 2015 data reported to the Extracorporeal Life Support Organization (ELSO) registry (19). The authors included in the analysis data from all patients 16 years old or older who were assigned a primary or secondary diagnosis of myocarditis in the over 230 U.S. and international ELSO member centres. So, the study population was formed by 147 patients and, among them, 134 (91.1%) were supported with VA-ECMO while the remainder with veno-venous ECMO. Of the 147 patients, 101 (68.7%) were weaned from ECMO and 83 (56.4%) survived to hospital discharge without heart transplantation. Transplant-free survival to discharge was 62% in those patients on ECMO support less than or equal to 1 week but it was 45% in patients requiring ECMO for more than 1 week. A multivariate logistic regression model was created to evaluate the association of pre-ECMO and ECMO support-related predictors and it demonstrated that the occurrence of pre-ECMO arrest and the need for higher ECMO support at 4 h were independently associated with in-hospital mortality. A second regression model was created to evaluate adverse events on ECMO and it demonstrated that neurologic events, renal failure, arrhythmia and hyperbilirubinemia were independently associated with in-hospital mortality.
More recently, Lorusso and coworkers analysed through an Italian multi-institutional investigation the results of VA-ECMO in the setting of acute fulminant myocarditis patients (20). The investigators purposely chose a more recent time frame (from January 2008 to December 2013) to assess modern ECMO systems and management, which included advanced VA-ECMO technology and components and more advanced expertise achieved in adult VA-ECMO for emergent cardiovascular diseases. Fifty-seven patients were included in this analysis and 43 (75.5%) patients achieved complete myocardial recovery with ECMO ablation. Overall survival to hospital discharge (excluding three patients who eventually received heart transplantation) was 66.6%. Multivariate analysis showed that low pH before VA-ECMO implantation, absence or long lactate normalization time and absence of functional cardiac recovery on ECMO were predictive of in-hospital death.
Discussion
Myocarditis is a rare inflammatory disease that deserves a particular consideration in the cardiac surgical community as it represents a real public health concern. Myocarditis accounts for approximately 10% of cases of sudden death in young adults (21). Moreover longitudinal studies of acute myocarditis have documented the development of dilated cardiomyopathy in 20% of patients (22).
The complexity of myocarditis is well depicted by its difficult pathophysiology, challenging diagnosis and extremely variable presentation (23). Indeed, the analysis of the histologic findings and clinical course allowed for a clinicopathologic classification of myocarditis in four different subgroups (24). Patients with fulminant myocarditis become acutely ill after a distinct viral prodrome and have severe cardiovascular compromise and ventricular dysfunction that either resolves spontaneously or results in death. Patients with acute, chronic active and chronic persistent myocarditis have a less distinct onset of illness. Therefore fulminant myocarditis should be considered as a distinct clinical entity with an excellent long-term prognosis (25). Previous studies showed that the long-term outcome of patients with acute myocarditis was poor as compared to that of patients with fulminant myocarditis (26,27). This difference could be explicated by the differences in patients’ clinical backgrounds, the time of cardiac symptoms presentation, and myocardial healing characteristics which both may witness the pathophysiology of myocarditis. Patients with myocarditis without a distinct onset may have already undergone the remodelling process following a viral infection, leading to dilated cardiomyopathy (13,22).
Owing to the available data collected in this review, VA-ECMO displays an overall survival to hospital discharge comprised between 55% and 78% in patients with fulminant and acute myocarditis developing cardiogenic shock. In a recent meta-analysis of the literature that analysed the clinical outcomes in fulminant myocarditis requiring VA-ECMO, the minimum and maximum reported rates of survival to hospital discharge were 58% and 88%, respectively, after removing pediatric patients and excluding one study that did not delineate clinical outcomes of their pediatric population (28). This percentage is similar to that of patients in cardiogenic shock state due to drug poisoning and is probably explained by the high potential of myocardial recovery shared by these pathologic conditions.
Predictors of myocardial recovery
The relatively low incidence of myocarditis among the general population and the even more infrequent development of cardiogenic shock requiring temporary MCS make any statistical attempt to identify possible predictors of myocardial recovery during VA-ECMO support both challenging and precious.
Chen and colleagues identified for the first time troponin T as a possible indicator to predict the recovery of the damaged myocardium (29); they found elevated troponin T levels before VA-ECMO implantation reflecting the cardiogenic shock state of the patients but the levels rapidly declined after VA-ECMO setup corresponding to the amelioration of the clinical course. Moreover they insisted on the observation that troponin T levels rapidly declined within 3 days of VA-ECMO support in the successfully rescued patients. In their following landmark report the authors also showed that the higher initial troponin levels did not preclude the possibility of myocardial recovery, thus highlighting the more significant role of slope trend of troponin decline (8). It means that the trend of the troponin decline provides a more specific guide to evaluate the myocardial recovery and to estimate the timing of weaning of the VA-ECMO rather than the absolute peak. Finally, in their 2011 updated single-centre experience, they confirmed the role of timing of peak troponin level as an important predictor for myocardial recovery (15). They found that there was a statistically significant increase in mortality when the troponin level did not decrease within 72 h after VA-ECMO implantation. The present finding could be explained by the fact that the injured myocardial mass is more related to the troponin area under the curve than the pic. Unfortunately the different laboratory parameters used over time (initially troponin T and then troponin I) limited the attempts to produce a standardized diagnostic tool (8).
In the comparative study published by Asaumi et al., patients who were not weaned from VA-ECMO and died exhibited a higher peak CK-MB level and a more depressed left ventricular systolic function than those who were weaned from VA-ECMO. Interestingly, despite similar peak CK-MB levels, there was a significant difference in fractional shortening between patients with fulminant myocarditis who were weaned from VA-ECMO and those with non-fulminant myocarditis. These findings indicate that the extent of myocardial dysfunction and necrosis caused by inflammatory responses may determine the acute outcome in myocarditis patients (13).
In the “Pitié-Salpêtrière” Hospital experience more severe disease at hospital admission (expressed by a Simplified Acute Physiology Score II ≥56) and higher troponin I levels (≥12 μg/L) at MCS initiation were associated with unsuccessful weaning and intensive care unit mortality (14).
However, in a recent prospective, observational, single-centre study, early measurements of cardiac biomarkers (blood N-terminal fragment of the B-type natriuretic peptide, troponin Ic, midregional fragment of the proatrial natriuretic peptide, proadrenomedullin and copeptin) were not useful for identifying those patients who would recover from refractory cardiogenic shock requiring VA-ECMO support (30). In particular, neither the absolute values of these biomarkers at days 1, 3 or 7 nor their kinetics during the first week of VA-ECMO support differed between patients weaned or not.
Left ventricular unloading
From a hemodynamic standpoint peripheral VA-ECMO can cause a significant increase of left ventricular afterload and, in some cases, pulmonary edema (31). This hemodynamic state is further exacerbated in case of stunned myocardium with severely depressed left ventricular ejection and absence of aortic valve opening. Finally, the presence of left ventricular distension is a major limitation to myocardial recovery. In papers providing detailed information left ventricular distension requiring left ventricular unloading is reported between 15% and 30% of peripheral VA-ECMO support for cardiogenic shock due to myocarditis (8,14,17,20,29).
When the increase of the inotropic support is not enough to prevent pulmonary edema, left ventricular unloading could be achieved using different techniques:
- Conversion from peripheral to central VA-ECMO: it is the most invasive but the most effective way to obtain a good left ventricular unloading. A cannula in the right superior pulmonary vein (32) or left ventricular apex can be used to decompress the left ventricle. Usually the cannulation of the ascending aorta provides an antegrade arterial flow, thus reducing left ventricular afterload. This technique requires of course a standard median sternotomy with a potential increased risk of bleeding and infectious complications;
- Cannulation of the left ventricular apex: in this technique the cannula is inserted in the left ventricular apex through an anterolateral minithoracotomy at the fourth-fifth left intercostal space. The cannula is then connected to the femoral venous drainage of the peripheral VA-ECMO using a Y-connector. This less invasive technique offers a good left ventricular decompression but displays an elevated risk of bleeding with recurrent left hemothorax. Some authors have also proposed a left ventricular apex cannulation through a subxiphoid minimally invasive approach (33);
- Impella axial pump: the Impella 5.0 is a micro-axial, catheter-based, short-term left ventricle assist device, which is inserted retrograde into the left ventricle across the aortic valve through a surgical peripheral access. While ensuring a good hemodynamic support, it allows effective left ventricular unloading (34). The right subclavian artery is nowadays the preferred approach to Impella 5.0 implementation. Other investigators described the possibility to use the Impella 2.5 in combination to VA-ECMO in order to unload the left ventricle (35). This percutaneous MCS offers only a partial unloading that is often not sufficient in patients with severely depressed left ventricular function; the new Impella CP could be an effective alternative to the surgical Impella 5.0 owing to pump flow up to 4 L/min and its totally percutaneous insertion;
- Percutaneous atrial septostomy: the principle is to create an atrial septal defect that allows left heart decompression through a left-to-right shunt. The efficacy of balloon or blade atrial septostomy depends mainly on the technical expertise of interventional cardiologists and seems best suited for the pediatric population (36,37);
- Other percutaneous techniques: in the literature there are several reports describing alternative percutaneous techniques of left ventricular unloading; these techniques include a trans-septal left atrial (38) or ventricular (39) cannula through an antegrade venous approach, transaortic left ventricular cannula through a retrograde arterial approach (40), transaortic pigtail catheter (41) and pulmonary artery cannula (42). These alternative techniques are to date limited to case reports or small case series and further studies are necessary to best define their role.
Our institutional policy to unload the left ventricle in peripheral VA-ECMO patients is the conversion to a central configuration. Our technique couples the cannulation of the ascending aorta and left ventricular apex. In our opinion, the cannulation of the right atrium is no more necessary owing to the large diameter (25 or 29 French) of available femoral venous cannulas (Figure 1).
Conclusions
Acute fulminant myocarditis developing refractory cardiogenic shock carries a high mortality despite improvements over time in the diagnosis and clinical management of this disease. VA-ECMO is the treatment of choice for such a critical ill population owing to its ease of setup, implantation, management and removal. VA-ECMO offers an overall survival to hospital discharge in patients suffering from myocarditis-induced cardiogenic shock comprised between 55% and 78%. Left ventricular unloading might be necessary in up to 30% of patients supported with peripheral VA-ECMO and is an effective technique owing to the high potential of recovery of myocarditis. Further investigations are warranted in order to identify potential predictors of myocardial recovery in patients under VA-ECMO support for myocarditis and so to define the subsequent decision-making algorithm in those who will not recover.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Caforio AL, Pankuweit S, Arbustini E, et al. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J 2013;34:2636-48. [Crossref] [PubMed]
- Kindermann I, Barth C, Mahfoud F, et al. Update on myocarditis. J Am Coll Cardiol 2012;59:779-92. [Crossref] [PubMed]
- Sagar S, Liu PP, Cooper LT. Myocarditis. Lancet 2012;379:738-47. [Crossref] [PubMed]
- Kirklin JK, Naftel DC, Kormos RL, et al. The fourth intermacs annual report: 4,000 implants and counting. J Heart Lung Transplant 2012;31:117-26. [Crossref] [PubMed]
- Kirklin JK, Naftel DC, Pagani FD, et al. Seventh intermacs annual report: 15,000 patients and counting. J Heart Lung Transplant 2015;34:1495-504. [Crossref] [PubMed]
- Lebreton G, Pozzi M, Mastroianni C, et al. Extracorporeal life support as a bridge to bridge: a strategy to optimize ventricular assist device results. Eur J Cardiothorac Surg 2015;48:785-91. [Crossref] [PubMed]
- McMurray JJ, Adamopoulos S, Anker SD, et al. ESC Committee for Practice Guidelines. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J 2012;33:1787-847. [Crossref] [PubMed]
- Chen YS, Yu HY, Huang SC, et al. Experience and result of extracorporeal membrane oxygenation in treating fulminant myocarditis with shock: what mechanical support should be considered first? J Heart Lung Transplant 2005;24:81-7. [Crossref] [PubMed]
- Chen JM, Spanier TB, Gonzalez JJ, et al. Improved survival in patients with acute myocarditis using external pulsatile mechanical ventricular assistance. J Heart Lung Transplant 1999;18:351-7. [Crossref] [PubMed]
- Kato S, Morimoto S, Hiramitsu S, et al. Use of percutaneous cardiopulmonary support of patients with fulminant myocarditis and cardiogenic shock for improving prognosis. Am J Cardiol 1999;83:623-5. [Crossref] [PubMed]
- Acker MA. Mechanical circulatory support for patients with acute-fulminant myocarditis. Ann Thorac Surg 2001;71:S73-6; discussion S82-5.
- Maejima Y, Yasu T, Kubo N, et al. Long-term prognosis of fulminant myocarditis rescued by percutaneous cardiopulmonary support device. Circ J 2004;68:829-33. [Crossref] [PubMed]
- Asaumi Y, Yasuda S, Morii I, et al. Favourable clinical outcome in patients with cardiogenic shock due to fulminant myocarditis supported by percutaneous extracorporeal membrane oxygenation. Eur Heart J 2005;26:2185-92. [Crossref] [PubMed]
- Mirabel M, Luyt CE, Leprince P, et al. Outcomes, long-term quality of life, and psychologic assessment of fulminant myocarditis patients rescued by mechanical circulatory support*. Crit Care Med 2011;39:1029-35. [Crossref] [PubMed]
- Hsu KH, Chi NH, Yu HY, et al. Extracorporeal membranous oxygenation support for acute fulminant myocarditis: analysis of a single center’s experience. Eur J Cardiothorac Surg 2011;40:682-8. [PubMed]
- Nakamura T, Ishida K, Taniguchi Y, et al. Prognosis of patients with fulminant myocarditis managed by peripheral venoarterial extracorporeal membranous oxygenation support: a retrospective single-center study. J Intensive Care 2015;3:5. [Crossref] [PubMed]
- Pages ON, Aubert S, Combes A, et al. Paracorporeal pulsatile biventricular assist device versus extracorporal membrane oxygenation–extracorporal life support in adult fulminant myocarditis. J Thorac Cardiovasc Surg 2009;137:194-7. [Crossref] [PubMed]
- Aoyama N, Izumi T, Hiramori K, et al. National survey of fulminant myocarditis in Japan. Circ J 2002;66:133-44. [Crossref] [PubMed]
- Diddle JW, Almodovar MC, Rajagopal SK, et al. Extracorporeal membrane oxygenation for the support of adults with acute myocarditis. Crit Care Med 2015;43:1016-25. [Crossref] [PubMed]
- Lorusso R, Centofanti P, Gelsomino S, et al. Venoarterial Extracorporeal membrane oxygenation for acute fulminant myocarditis in adult patients: a 5-year multi-institutional experience. Ann Thorac Surg 2016;101:919-26. [Crossref] [PubMed]
- Fabre A, Sheppard MN. Sudden adult death syndrome and other non-ischaemic causes of sudden cardiac death. Heart 2006;92:316-20. [Crossref] [PubMed]
- D'Ambrosio A, Patti G, Manzoli A, et al. The fate of acute myocarditis between spontaneous improvement and evolution to dilated cardiomyopathy: a review. Heart 2001;85:499-504. [Crossref] [PubMed]
- Banfi C, Guerbaai RA, Giraud R, et al. Role of endomyocardial biopsy in the diagnostic procedure of pheochromocytoma induced cardiogenic shock. Int J Cardiol 2016;206:138. [Crossref] [PubMed]
- Lieberman EB, Hutchins GM, Herskowitz A, et al. Clinicopathoiogic description of myocarditis. J Am Coll Cardiol 1991;18:1617-26. [Crossref] [PubMed]
- McCarthy RE, Boehmer JP, Hruban RH, et al. Long-term outcome of fulminant myocarditis as compared with acute (nonfulminant) myocarditis. N Eng J Med 2000;342:690-5. [Crossref] [PubMed]
- Mason JW, O'Connell JB, Herskowitz A, et al. A clinical trial of immunosuppressive therapy for myocarditis. N Eng J Med 1995;333:269-75. [Crossref] [PubMed]
- Grogan M, Redfield MM, Bailey KR, et al. Long-term outcome of patients with biopsy-proved myocarditis: comparison with idiopathic dilated cardiomyopathy. J Am Coll Cardiol 1995;26:80-4. [Crossref] [PubMed]
- Cheng R, Hachamovitch R, Kittleson M, et al. Clinical outcomes in fulminant myocarditis requiring extracorporeal membrane oxygenation: a weighted meta-analysis of 170 patients. J Card Fail 2014;20:400-6. [Crossref] [PubMed]
- Chen YS, Wang M, Chou NK, et al. Rescue for acute myocarditis with shock by extracorporeal membrane oxygenation. Ann Thorac Surg 1999;68:2220-4. [Crossref] [PubMed]
- Luyt CE, Landivier A, Leprince P, et al. Usefulness of cardiac biomarkers to predict cardiac recovery in patients on extracorporeal membrane oxygenation support for refractory cardiogenic shock. J Crit Care 2012;27:524.e7-14. [Crossref] [PubMed]
- Burkhoff D, Sayer G, Doshi D, et al. Hemodynamics of Mechanical Circulatory Support. J Am Coll Cardiol 2015;66:2663-74. [Crossref] [PubMed]
- Weymann A, Schmack B, Sabashnikov A, et al. Central extracorporeal life support with left ventricular decompression for the treatment of refractory cardiogenic shock and lung failure. J Cardiothorac Surg 2014;9:60. [Crossref] [PubMed]
- Guirgis M, Kumar K, Menkis AH, et al. Minimally invasive left-heart decompression during venoarterial extracorporeal membrane oxygenation: an alternative to a percutaneous approach. Interact Cardiovasc Thorac Surg 2010;10:672-4. [Crossref] [PubMed]
- Beurtheret S, Mordant P, Pavie A, et al. Impella and extracorporeal membrane oxygenation: a demanding combination. ASAIO J 2012;58:291-3. [Crossref] [PubMed]
- Cheng A, Swartz MF, Massey HT. Impella to unload the left ventricle during peripheral extracorporeal membrane oxygenation. ASAIO J 2013;59:533-6. [Crossref] [PubMed]
- Bignon M, Roule V, Dahdouh Z, et al. Percutaneous balloon atrioseptostomy for left heart discharge in extracorporeal life support patients with persistent pulmonary edema. J Interv Cardiol 2012;25:62-7. [Crossref] [PubMed]
- Seib PM, Faulkner SC, Erickson CC, et al. Blade and balloon atrial septostomy for left heart decompression in patients with severe ventricular dysfunction on extracorporeal membrane oxygenation. Catheter Cardiovasc Interv 1999;46:179-86. [Crossref] [PubMed]
- Aiyagari RM, Rocchini AP, Remenapp R, et al. Decompression of the left atrium during extracorporeal membrane oxygenation using a transseptal cannula incorporated into the circuit*. Crit Care Med 2006;34:2603-6. [Crossref] [PubMed]
- Alkhouli M, Narins CR, Lehoux J, et al. Percutaneous Decompression of the Left Ventricle in Cardiogenic Shock Patients on Venoarterial Extracorporeal Membrane Oxygenation. J Card Surg 2016;31:177-82. [Crossref] [PubMed]
- Chocron S, Perrotti A, Durst C, et al. Left ventricular venting through the right subclavian artery access during peripheral extracorporeal life support. Interact Cardiovasc Thorac Surg 2013;17:187-9. [Crossref] [PubMed]
- Hong TH, Byun JH, Lee HM, et al. Initial experience of transaortic catheter venting in patients with venoarterial extracorporeal membrane oxygenation for cardiogenic shock. ASAIO J 2016;62:117-22. [PubMed]
- Avalli L, Maggioni E, Sangalli F, et al. Percutaneous left-heart decompression during extracorporeal membrane oxygenation: an alternative to surgical and transeptal venting in adult patients. ASAIO J 2011;57:38-40. [Crossref] [PubMed]



