Benefits of using omental pedicle flap over muscle flap for closure of open window thoracotomy
Introduction
Thoracic empyema, which usually occurs after lung resection and pneumonia, remains a life-threatening infection, with a persistently high mortality rate ranging from 6% to 24% (1-4). Adequate drainage is the first step to improve this infectious condition. In the acute phase, closed drainage of thoracic empyema may be attempted; however, in cases with uncontrolled infection and bronchopleural fistula (BPF), open drainage such as an open window thoracotomy (OWT) has been used. OWT is considerably effective in cleaning the thoracic cavity; however, it is one of the most invasive therapies that deteriorates patients’ quality of life. Immediate OWT closure is important, and we should evaluate the risk of recurrence, decide proper timing to perform the closure operation and select what we use to eliminate the thoracic space. Intrathoracic transposition of muscle or omental pedicle flap is one of the most radical surgeries to seal the thoracic cavity (5), but the better technique among the two is unknown. In this study, we aimed to evaluate the outcomes of using omental pedicle and muscle flaps for OWT closure. To the best of our knowledge, this is the first evaluation of the outcomes such as mortality, morbidity, recurrence and hospital stay after OWT closure.
Methods
This was an observational retrospective cohort study performed at a single institution. This article was approved to ethics committee of the University of Occupational and Environmental Health Japan, and the number of ethics approval was H27-080. Informed consent under this study was obtained to patients before taking part.
Study population
We included 27 consecutive patients who underwent OWT closure using either omental pedicle or muscle flap at the hospital of the University of Occupational and Environmental Health, Japan, between January 2005 and December 2014. Data were collected retrospectively from medical and operative records.
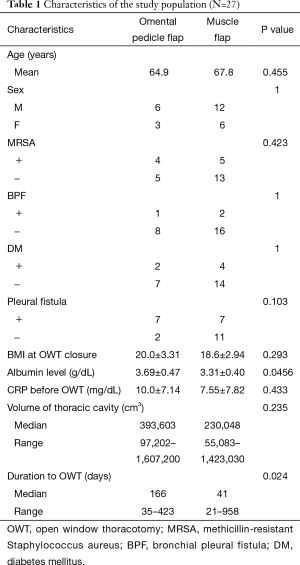
Sex, age, diabetes mellitus (DM), body mass index (BMI) at OWT closure, BPF, pleural fistula, C-reactive protein (CRP) before OWT and serum albumin levels before OWT closure, volume of empyema space, methicillin-resistant Staphylococcus aureus (MRSA) infection and duration of OWT are stated in Table 1.
Full table
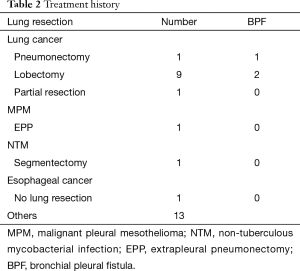
Table 2 states the characteristics of 13 consecutive patients (10 with lung cancer, 1 with malignant mesothelioma, 1 with mycobacterial infection and 1 with oesophageal cancer) who developed thoracic empyema after lung resection by extrapleural pneumonectomy (EPP) (n=1), pneumonectomy (n=1), lobectomy (n=9), segmentectomy (n=1) and partial resection (n=1). Three patients developed BPF. The cause of thoracic empyema was pneumonia in 11 patients and unknown in 2 patients.
Full table
Bacterial culture was performed in all patients. The causative of thoracic empyema was bacteria in 25 patients, MRSA in 9 patients and fungi in 2 patients; tuberculosis was not detected.
The thoracic cavity was evaluated by computed tomography (CT).
Management of empyema and surgical procedure
At our institution, the usual first step for thoracic empyema treatment was chest tube drainage or video-assisted thoracoscopic surgery (VATS) debridement. Chest drainage was performed in all patients and VATS debridement was performed in six patients. However, all patients had uncontrollable thoracic infection; therefore, OWT was performed.
The skin-incision approach for OWT was determined based on the location of thoracic dead space on preoperative CT imaging. This approach was selected to preserve as much muscle as possible; the number rib bones resected was 2–6. During OWT, we performed gauze dressing once or twice a day, depending on the condition of the thoracic cavity. Some cases were administered antibiotics. The time for OWT closure was determined either when the thoracic cavity was visually clean, the bacteria had been eradicated or BPF was closed.
The wound closure operation included combined limited thoracoplasty and intrathoracic transposition of either muscle or omental pedicle flap, depending on the volume of the thoracic cavity, bacterial aetiology of the infection, influence of previous thoracic surgery, nutrition status and history of abdominal operation.
Omental pedicle flap was used in 9 patients, whereas muscle flap was used in 18 patients.
All omental pedicle flap intrathoracic transposition procedures were performed via median laparotomy; the greater omentum was mobilized from the greater curvature of the stomach with the preservation of the gastroepiploic artery. Thoracotomy with rib bone resection was performed to reduce the cavity, followed by debridement and 5–10 L of saline solution lavage of the previously infected site. The thoracic cavity was filled with the greater omental pedicle flap through a 1–2-cm incision on the diaphragm or through the substernum. The omental pedicle flap was fixed onto the thoracic space using biological glue and absorbable suture.
Intrathoracic transposition of extrathoracic muscle was performed through the latissimus dorsi, serratus anterior, intercostal muscle and/or pectoralis major. Latissimus dorsi alone was used in seven patients, latissimus dorsi with serratus anterior was used in five patients, serratus anterior alone was used in one patient, pectoralis major alone was used in three patients and intercostal muscle alone was used in two patients. Muscle flap procedure was performed through an incision tracing with the previous OWT incision. After separating from the chest wall and fat tissue, the muscle flap was transposed onto the thoracic cavity while preserving the arterial supply.
Three patients did not need the insertion of a chest tube for drainage but 24 patients needed its insertion to monitor infection after surgery. In 17 cases, the procedures were performed by a general thoracic surgeon and a digestive organ surgeon, whereas in 1 case, the procedure was performed by a plastic surgeon with a thoracic surgical team.
Outcome
We evaluate mortality, morbidity, local recurrence, success, duration of drain placement after closure operation and postoperative hospital stay between omental pedicle flap and muscle flap.
Mortality is observed for a year. Morbidity was defined as the need for surgical procedure after initial operation or drug intervention of more than 14 days. Local recurrence meant infection and fistula after operation. Local infection recurrence was defined as positive bacterial culture of the infected site with accompanying signs and symptoms such as fever, fatigue and chills. Success was defined as resolution of infection with antibiotic administration without the need for surgical treatment.
Statistical analyses
All statistical analyses were performed with Stata version 14.0 (StataCorp, College Station, TX) and R commander (R 2.13.0; R Foundation for Statistical Computing, Vienna, Austria). Data were expressed as range, median or mean, as appropriate. Comparative evaluation was performed using the Student’s t-test, Mann-Whitney U test, Spearman’s rank correlation coefficient test and Fischer’s exact test, as appropriate. Statistical significance was determined at a P value of less than 0.05.
Results
Patient characteristics
Table 1 demonstrates patient characteristics. The two groups were identical in terms of age, sex, BMI at OWT closure, BPF, pleural fistula, CRP before OWT and volume of the thoracic cavity. However, in comparison with the muscle flap group, the omental pedicle flap group had significantly higher preoperative serum albumin levels (3.689 vs. 3.310 g/dL, P=0.0456, according to the Student’s t-test) and longer duration of OWT (166 vs. 41 days, P=0.024, according to the Mann-Whitney U test).
Mortality, morbidity, local recurrence and success
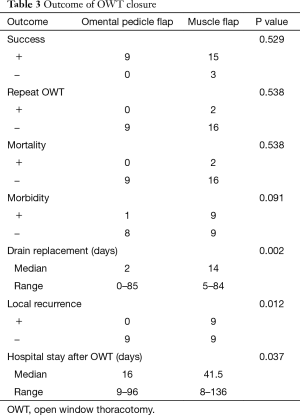
Mortality was observed in two patients belonging to the muscle flap group and no patient belonging to the omental pedicle flap group (0% vs. 11.2%, P=0.538, according to the Fisher’s exact test; Table 3). In the muscle flap group, an 84-year-old woman died because of sepsis due to recurrent thoracic infection on postoperative day 30. The second mortality case was a 77-year-old man who underwent repeat OWT due to recurrent BPF after right pneumonectomy; the patient died on postoperative day 53 because of septic shock.
Full table
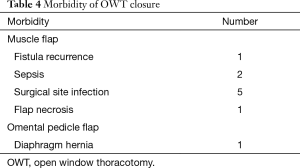
In this series, perioperative morbidity occurred in one patient belonging to the omental pedicle flap group and nine patients belonging to the muscle flap group [11.1% (1/9) vs. 50.0% (9/18), P=0.091, according to the Fisher’s exact test; Table 3]. One patient in the omental pedicle flap group developed diaphragmatic hernia, which was successfully treated by emergency hernia repair. In the muscle flap group, sepsis due to aspiration pneumonia occurred in two cases, fistula recurrence occurred in one case, surgical site infection occurred in five cases and muscle flap necrosis occurred in one case (Table 4).
Full table
The rate of local recurrence of thoracic space infection was significantly higher with muscle flap than with omental pedicle flap [0% (0/9) vs. 50.0% (9/18), P=0.012, according to the Fisher’s exact test; Table 3]. These patients were administered antibiotics and underwent drain replacement; two patients underwent repeat OWT owing to non-resolved infection and persistent pleural fistula.
Success rate was similar between the two groups [100% (9/9) with omental pedicle flap vs. 83.3% (15/18) with muscle flap, P=0.529, according to the Fisher’s exact test; Table 3].
Duration of drain placement after closure operation and postoperative hospital stay
The median duration of indwelling chest drainage after closure operation was significantly shorter with omental pedicle flap than with muscle flap (2 vs. 18.5 days, P=0.002, according to the Mann-Whitney U test; Table 3). The median duration of the postoperative hospital stay was significantly shorter with the omental pedicle flap than with the muscle flap (16.0 vs. 41.5 days, P=0.037, according to the Mann-Whitney U test).
Discussion
This retrospective study demonstrated that omental pedicle flap was superior to muscle flap in reducing local recurrence and shortening postoperative hospital stay after OWT closure. To my best knowledge, this is the first report that compared the mortality, morbidity, recurrence and postoperative hospital stay between the use of omental pedicle and muscle flaps for OWT closure.
Control of thoracic empyema relies on a strategy to reduce bacteria and eliminate infection. VATS debridement is effective as an initial operation (6), but OWT for open drainage should be considered when infection is uncontrolled after VATS. However, being one of the most invasive therapies, OWT closure at the soonest possible time is desirable to improve both the quality of life and prognosis. In a multivariate analysis of 35 consecutive patients, Hato demonstrated that the success of OWT closure was related to mortality (7). However, OWT closure itself is a challenging procedure with high mortality risks. Some studies have reported that the success rate of OWT closure is 26–94% and the mortality rate is 2.6–13.3% (8-11).
The best technique for OWT closure and thoracic cavity sealing is unclear. We often performed thoracotomy using either muscle or omental pedicle flap as the closure technique. Muscle flap is one of the most common and acceptable procedures for OWT closure. Some studies have reported that mortality rate with muscle flap is approximately 5%, success rate, which was defined as chest closure and cure of empyema, is over 90% and postoperative hospital stay is approximately 40 days (range, 4–150 days) (12-15). These results were similar to our data, indicating the feasibility of our procedure.
Comparison of outcomes between omental pedicle and muscle flaps has been difficult because of the heterogeneity of patients who undergo OWT closure. Omental pedicle flap is more frequently used for severe cases, involving complicated infection, OWT after BPF and a previous pneumonectomy (5,16). On the other hand, muscle pedicle flap is usually applied for non-severe cases. This heterogeneity interrupted the proper analysis of which is better to use for OWT closure. In this study, the baseline characteristics of the two groups were similar and enabled proper analysis.
Omental pedicle flap for OWT closure is the most radical surgical treatment for thoracic empyema (5,16-18) and is used for very severe cases, involving MRSA empyema, a previous pneumonectomy empyema caused by BPF and chronic empyema caused by aspergillus and tuberculosis. This is because the omentum has anti-inflammatory properties and promotes tissue healing because of the presence of abundant blood vessels and lymphatics (19). Okumura reported that using omental pedicle flap for chronic empyema provided clinical success in 82.6% (19/23) without compromising pulmonary function. Moreover, mortality rate was 4.3% (1/23) and recurrence rate was 8.7% (2/23). The results of our data were not inferior to those of this previous study.
In this study, the shorter hospital stay and duration of drainage after OWT with omental pedicle flap was probably because of the efficient cleansing of the thoracic cavity, absorption of discharge, preservation of good healing conditions, longer duration of OWT and better nutritional status, as demonstrated by the significantly higher preoperative serum albumin levels in the omental pedicle flap group than the muscle flap group.
Despite the good outcomes of omental pedicle flap, laparotomy may have severe complications, such as ileus, diaphragmatic hernia, haemorrhage after surgery and some minor abdominal complaints. Okumura (5) showed that the incidence of abdominal complication was 39.1% (9/23). Kurahashi (20) reported that the incidence of severe abdominal complication was 8.7% (2/23). In this study, we showed that the overall morbidity was 12.9% (1/9). Our data was not inferior to the past reports.
In this study, local recurrence with muscle flap was extremely higher than that with omental pedicle flap, probably because of the inappropriate selection of material for transposition. Two BPF cases that underwent muscle flap transposition had a history of abdominal surgery. BPF is a prognostic factor for OWT and a predictor of OWT closure (8,21). Therefore, we should aggressively choose to use omental pedicle flap in complicated cases.
The best method for OWT closure is unclear, but it is important to consider the volume of the thoracic cavity, location, incision, muscle damage, BPF, history of abdominal surgery and aetiology of the infection (MRSA, aspergillus and tuberculosis) and to not hesitate to perform thoracotomy to obliterate dead space. Omental pedicle flap leads to good healing and prevention of local recurrence; therefore, we should make a firm decision to use this flap for severe thoracic empyema. On the other hand, we should be reminded that omental pedicle flap is an invasive procedure. In the future, studies are needed to clarify the population in which omental pedicle flap is appropriate and the prognostic factors for OWT closure.
Study limitation
First, this cohort study had a retrospective design, was conducted in a single institution and comprised a small number of subjects; therefore, bias was inevitable. Second, the study period was ten years, during which antibiotic therapy for empyema has improved to include coverage for MRSA. In this study, MRSA infection was observed in 25.9% cases and another therapeutic strategy is currently being developed. Third, we were not able to perform multivariate analysis because this series was too small. A large-number and multi-centre study is needed to verify the outcomes of different OWT closure techniques.
Conclusions
Omental pedicle flap was superior to muscle flap in reducing local recurrence and shortening postoperative hospital stay after OWT closure. However, mortality, morbidity and success rates were not influenced by the type of flap used for OWT closure. Omental pedicle flap may be more appropriate than muscle flap in high risk cases in consideration of the volume of the thoracic cavity, location, previous operation, history of abdominal surgery, bacterial aetiology of empyema and status of thoracic infection.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This article was approved to ethics committee of the University of Occupational and Environmental Health Japan, and the number of ethics approval was H27-080. Informed consent under this study was obtained to patients before taking part.
References
- Davies CW, Kearney SE, Gleeson FV, et al. Predictors of outcome and long-term survival in patients with pleural infection. Am J Respir Crit Care Med 1999;160:1682-7. [Crossref] [PubMed]
- Ferguson AD, Prescott RJ, Selkon JB, et al. The clinical course and management of thoracic empyema. QJM 1996;89:285-9. [Crossref] [PubMed]
- Mandal AK, Thadepalli H, Mandal AK, et al. Outcome of primary empyema thoracis: therapeutic and microbiologic aspects. Ann Thorac Surg 1998;66:1782-6. [Crossref] [PubMed]
- Ashbaugh DG. Empyema thoracis. Factors influencing morbidity and mortality. Chest 1991;99:1162-5. [Crossref] [PubMed]
- Okumura Y, Takeda S, Asada H, et al. Surgical results for chronic empyema using omental pedicled flap: long-term follow-up study. Ann Thorac Surg 2005;79:1857-61. [Crossref] [PubMed]
- Angelillo Mackinlay TA, Lyons GA, Chimondeguy DJ, et al. VATS debridement versus thoracotomy in the treatment of loculated postpneumonia empyema. Ann Thorac Surg 1996;61:1626-30. [Crossref] [PubMed]
- Hato T, Suzuki S, Harada M, et al. Comprehensive treatment approach is necessary for the closure of open window thoracostomy: an institutional review of 35 cases. Surg Today 2014;44:443-8. [Crossref] [PubMed]
- Shamji FM, Ginsberg RJ, Cooper JD, et al. Open window thoracostomy in the management of postpneumonectomy empyema with or without bronchopleural fistula. J Thorac Cardiovasc Surg 1983;86:818-22. [PubMed]
- Goldstraw P. Treatment of postpneumonectomy empyema: the case for fenestration. Thorax 1979;34:740-5. [Crossref] [PubMed]
- Pairolero PC, Arnold PG, Trastek VF, et al. Postpneumonectomy empyema. The role of intrathoracic muscle transposition. J Thorac Cardiovasc Surg 1990;99:958-66; discussion 966-8. [PubMed]
- García-Yuste M, Ramos G, Duque JL, et al. Open-window thoracostomy and thoracomyoplasty to manage chronic pleural empyema. Ann Thorac Surg 1998;65:818-22. [Crossref] [PubMed]
- Jadczuk E. Posptneumonectomy empyema. Eur J Cardiothorac Surg 1998;14:123-6. [Crossref] [PubMed]
- Regnard JF, Alifano M, Puyo P, et al. Open window thoracostomy followed by intrathoracic flap transposition in the treatment of empyema complicating pulmonary resection. J Thorac Cardiovasc Surg 2000;120:270-5. [Crossref] [PubMed]
- Krassas A, Grima R, Bagan P, et al. Current indications and results for thoracoplasty and intrathoracic muscle transposition. Eur J Cardiothorac Surg 2010;37:1215-20. [Crossref] [PubMed]
- Stefani A, Jouni R, Alifano M, et al. Thoracoplasty in the current practice of thoracic surgery: a single-institution 10-year experience. Ann Thorac Surg 2011;91:263-8. [Crossref] [PubMed]
- Levashev YN, Akopov AL, Mosin IV. The possibilities of greater omentum usage in thoracic surgery. Eur J Cardiothorac Surg 1999;15:465-8. [Crossref] [PubMed]
- Ayabe T, Yoshioka M, Fukushima Y, et al. Study of surgical treatment with omental flap transposition for chronic empyema. Kyobu Geka 2003;56:989-94; discussion 994-6. [PubMed]
- Yokomise H, Takahashi Y, Inui K, et al. Omentoplasty for postpneumonectomy bronchopleural fistulas. Eur J Cardiothorac Surg 1994;8:122-4. [Crossref] [PubMed]
- Kitano M. Omentoplasty in thoracic surgery. Gen Thorac Cardiovasc Surg 2008;56:483-9. [Crossref] [PubMed]
- Kurahashi Y, Okubo K, Cho H, et al. Omentoplasty for thoracic problems - Usefulness of pedicled omentum and review of unsuccessful cases. Jpn J Chest Surg 2004;18:532-7. [Crossref]
- Massera F, Robustellini M, Pona CD, et al. Predictors of successful closure of open window thoracostomy for postpneumonectomy empyema. Ann Thorac Surg 2006;82:288-92. [Crossref] [PubMed]


