Clinical innovations in minimally invasive surgery in Korea
Changing trends of VATS in Republic of Korea
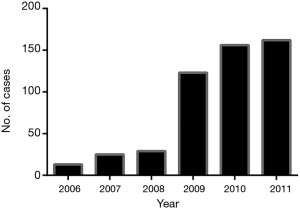
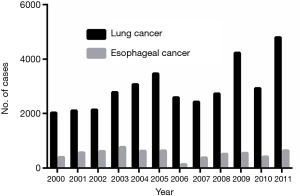
In Korea, innovative devices have driven the rapid shift to minimally invasive surgery for thoracic procedures. The number of minimally invasive operations has been increasing (Figure 1); the minimally invasive approach to thoracic disease has been popularized by various organizations and is now the standard procedure in Korea. Earlier, a pioneer in video-assisted thoracoscopic surgery (VATS) was not able to attain sufficient interest within the country and could not establish the technique as strongly here as in other countries (1,2). Many Korean thoracic surgeons have been encouraged to use VATS by the Korean Association of Thoracic Surgical Oncology (KATSO) and the Asia Thoracoscopic Surgery Education Program (ATEP), an Asian collaborative VATS education program (3). Currently, most thoracic surgeons in Korea perform VATS (4). It is not clear who performed the first VATS lung surgery in Korea, but literature reviews in the Korean Journal of Thoracic Cardiovascular Surgery revealed that VATS was first used in 1991 (5) and was first used for major lung resection in 1993 (6). VATS has been used increasingly frequently to treat thoracic disease, and the volume of robotic thoracic surgeries being performed has gradually increased in Korea: there were 2 centers in 2006, but 16 centers in 2015 (7). In addition, single-incision VATS has recently been popularized and is considered a feasible thoracoscopic alternative to conventional multiport VATS (8-10). Obviously great changes and progress has been made in thoracic surgery. Figure 2 shows the rapid evolution in thoracic surgery in our center between 2000 and 2015. Currently, the single-port approach is often used for thoracic surgery at our center (11,12), but it is not popular at the major centers in Korea (>2,000 cases per year). Compared to conventional VATS, the single-port approach requires longer operation times and a longer learning curve at early period. In addition, the instruments for single-port VATS may not be as easily available as those for conventional VATS. These reasons have prevented widespread adoption of this innovative technique. In addition, the socioeconomic environment and debates over the increasing national medical costs and insurance limit the introduction of new instruments and devices without great benefit for patients even though they showed clear clinical evidence of success. Alternative techniques such as uniportal surgery (13,14) and robotic surgery for lung (15) and esophageal cancer (16) are being promoted by a few pioneers in Korea.
Robotic surgery in Korea
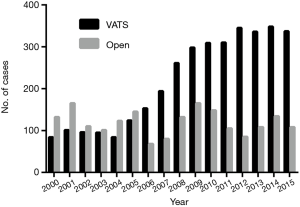
Robotic surgical systems provide high-definition 3-dimensional video systems, articulated wrists, tremor filtering, and other functions that are limited in conventional VATS systems. In Korea, robotic surgery for thoracic disease began in 2006 (7). Between 2006 and 2011, the use of robotic surgery for thoracic disease increased sharply in major hospitals; by 2011, this technique was being used for 150 patients per year (Figure 3). The most common indications were lung cancer, esophageal cancer, and mediastinal tumors. Some thoracic surgeons had reported the early outcomes of robotic surgery for lung cancer and esophageal cancer. However, the recent trend in robotic surgery has changed in Korea; currently, only a small number of thoracic surgeons perform robotic surgery, and these operations have been centralized to a few high-volume centers. In addition, higher costs, lack of clear benefits, and low volumes in most centers may be major causes in this phenomenon. In addition, because of specific provisions in the Korean National Health Insurance Service (NHIS), the patients are responsible for all medical costs of robotic surgery for thoracic disease. In contrast, more than 90% of the medical costs for other surgical procedures (VATS, open surgery) can be reimbursed by NHIS. Despite having many advantages for surgeon, robotic surgery is not used as often for thoracic disease as it is for other indications. This intuitive, remote surgical system has become the standard approach for pelvic, urological, gynecological, and colorectal surgery. However, the absolute indication for use in thoracic disease remains unclear, unlike for the use of VATS surgery in thoracic disease. Unfortunately, our center recently started using a robotic system [2016] and has not many experiences. The previously mentioned problems regarding medical cost reimbursement and centralization to high-volume center for proper education should be addressed.
Single-port VATS in Korea
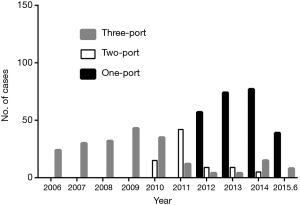
Over the past decades, the minimally invasive approach has been used increasingly for thoracic surgical procedures; today, most of thoracic surgeries performed are minimally invasive. Recently, single-port VATS (uniportal or single-incisional approach) has been introduced as an alternative to conventional multiport VATS procedures (12,17); our center launched this procedure in 2005 (8). We have changed our procedure from conventional VATS to the single-port version for most thoracic diseases, including benign lung cancer and other lung diseases (Figure 4). The concept behind this procedure is that VATS can be performed through one small (2–4 cm) hole with the same benefits as multiport VATS, but with fewer incisions and less intercostal pain. Because of the technical limitations of the instruments, only a few thoracic surgeons are performing this procedure in Korea. However, uniportal VATS might become more popular in the future, with improvement in endoscopic instruments.
Innovative surgical option for thoracic surgery in Korea
As the elderly population in Korea has rapidly grown over recent decades, the number of older patients who need thoracic surgery has increased. In clinical situations, we usually encounter elderly patients (more than 75 years) who have early lung cancer with poor pulmonary reserve or with other comorbidities. Minimally invasive surgery could be the best option for these patients, for whom it may not be possible to perform open surgical procedures safely. Our center is now focusing on using various innovative, image-guided surgical techniques to minimize resections and incisions, and we are performing clinical trials regarding this issue. Preservation of normal lung parenchyma might be an important prognostic factor for surgery, especially in older patients. Recent advances in image-guided VATS in hybrid settings (18,19) and in electromagnetic navigational bronchoscopic localization tools (20) might enable us to correctly localize tumors to perform sublobar resections, such as segmentectomies in patients with poor pulmonary reserve. In the near future, the use of image-guided surgery with various innovative techniques will increase and could become popular (21). Our center is the one of leading groups in Korea for clinical research on image-guided surgery with near-infrared imaging systems, although this technique is not popular at large volume centers (22).
Summary
Advancements in techniques have allowed thoracic surgery to evolve from radical resection by open surgery to minimal resection with minimally invasive techniques, and from requiring large incisions to requiring small incisions. Such changes in thoracic surgery are being seen in Korea. These innovations were made possible in Korea by pioneer surgeons who were dedicated to minimally invasive thoracic surgery and who overcame many obstacles to understand and adopt the latest surgical techniques. Currently, many Korean hospitals, including our center, are experiencing great changes in thoracic surgery, and the future will be challenging for young thoracic surgeons who are training in this country. The clinical experiences of Asian thoracic surgeons and the cooperation among them in research will promote the advancement of thoracic surgery in the future.
Acknowledgements
Funding: This work was supported by a grant from the National Research Foundation of Korea (NRF) grant funded by the Ministry of Education, Science and Technology (NRF-2015R1A2A2A04005760) and “the Technology Innovation Program” (N0001689) funded By the Ministry of Trade, industry & Energy (MI, Korea).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Kim K, Kim HK, Park JS, et al. Video-assisted thoracic surgery lobectomy: single institutional experience with 704 cases. Ann Thorac Surg 2010;89:S2118-22. [Crossref] [PubMed]
- Park JS, Kim K, Choi MS, et al. Video-Assisted Thoracic Surgery (VATS) lobectomy for pathologic stage I non-small cell lung cancer: a comparative study with thoracotomy lobectomy. Korean J Thorac Cardiovasc Surg 2011;44:32-8. [Crossref] [PubMed]
- Jheon S, Yang HC, Cho S. Video-assisted thoracic surgery for lung cancer. Gen Thorac Cardiovasc Surg 2012;60:255-60. [Crossref] [PubMed]
- Kim HK. Video-assisted thoracoscopic lobectomy for lung cancer. J Korean Med Assoc 2012;55:1193-8. [Crossref]
- Kim KH. Thoracoscopic treatment of spontaneous pneumothorax. Korean J Thorac Cardiovasc Surg 1991;24:261-264.
- Kim HK, Lee DY, Yoon YH, et al. Videothoracoscopic operation. Korean J Thorac Cardiovasc Surg 1993;26:86-8.
- Kang CH, Bok JS, Lee NR, et al. Current trend of robotic thoracic and cardiovascular surgeries in Korea: analysis of seven-year national data. Korean J Thorac Cardiovasc Surg 2015;48:311-7. [Crossref] [PubMed]
- Kim HK, Choi YH. The feasibility of single-incision video-assisted thoracoscopic major pulmonary resection performed by surgeons experienced with a two-incision technique. Interact Cardiovasc Thorac Surg 2015;20:310-5. [Crossref] [PubMed]
- Song IH, Yum S, Choi W, et al. Clinical application of single incision thoracoscopic surgery: early experience of 264 cases. J Cardiothorac Surg 2014;9:44. [Crossref] [PubMed]
- Yang HC, Cho S, Jheon S. Single-incision thoracoscopic surgery for primary spontaneous pneumothorax using the SILS port compared with conventional three-port surgery. Surg Endosc 2013;27:139-45. [Crossref] [PubMed]
- Han KN, Kim HK, Lee HJ, et al. Single-port video-assisted thoracoscopic pulmonary segmentectomy: a report on cases†. Eur J Cardiothorac Surg 2016;49 Suppl 1:i42-7. [PubMed]
- Ng CS, Kim HK, Wong RH, et al. Single-port video-assisted thoracoscopic major lung resections: experience with 150 consecutive cases. Thorac Cardiovasc Surg 2016;64:348-53. [Crossref] [PubMed]
- You SX. Professor Hyun Koo Kim: a great master of single port video-assisted thoracoscopic surgery. J Thorac Dis 2015;7:E382-3. [PubMed]
- Chung JH, Choi YS, Cho JH, et al. Uniportal video-assisted thoracoscopic lobectomy: an alternative to conventional thoracoscopic lobectomy in lung cancer surgery? Interact Cardiovasc Thorac Surg 2015;20:813-9. [Crossref] [PubMed]
- Jang HJ, Lee HS, Park SY, et al. Comparison of the early robot-assisted lobectomy experience to video-assisted thoracic surgery lobectomy for lung cancer: a single-institution case series matching study. Innovations (Phila) 2011;6:305-10. [Crossref] [PubMed]
- Kim DJ, Hyung WJ, Lee CY, et al. Thoracoscopic esophagectomy for esophageal cancer: feasibility and safety of robotic assistance in the prone position. J Thorac Cardiovasc Surg 2010;139:53-59.e1. [Crossref] [PubMed]
- Sihoe AD. The evolution of minimally invasive thoracic surgery: implications for the practice of uniportal thoracoscopic surgery. J Thorac Dis 2014;6:S604-17. [PubMed]
- Oh Y, Lee YS, Quan YH, et al. Thoracoscopic color and fluorescence imaging system for sentinel lymph node mapping in porcine lung using indocyanine green-neomannosyl human serum albumin: intraoperative image-guided sentinel nodes navigation. Ann Surg Oncol 2014;21:1182-8. [Crossref] [PubMed]
- Doo KW, Yong HS, Kim HK, et al. Needlescopic resection of small and superficial pulmonary nodule after computed tomographic fluoroscopy-guided dual localization with radiotracer and hookwire. Ann Surg Oncol 2015;22:331-7. [Crossref] [PubMed]
- Pearlstein DP, Quinn CC, Burtis CC, et al. Electromagnetic navigation bronchoscopy performed by thoracic surgeons: one center's early success. Ann Thorac Surg 2012;93:944-9; discussion 949-50. [Crossref] [PubMed]
- Oh Y, Quan YH, Kim M, et al. Intraoperative fluorescence image-guided pulmonary segmentectomy. J Surg Res 2015;199:287-93. [Crossref] [PubMed]
- Kim HK, Quan YH, Choi BH, et al. Intraoperative pulmonary neoplasm identification using near-infrared fluorescence imaging. Eur J Cardiothorac Surg 2016;49:1497-502. [Crossref] [PubMed]