Free jejunum interposition as salvage surgery after cervical esophagus injury
Introduction
Stomach is the most commonly used organ for reconstruction of esophagus after esophagectomy. It got the merit of easy to manipulate, less surgical relative trauma and less influence on the rest of digest system. In some rare cases when stomach was not suitable for such construction, other optional organs, such as colon and jejunum should probably be the alternates. Compared with jejunum, the usage of colon have been considered as having several disadvantages, such as regurgitation and unpleasant sensation of fullness (1,2). So in such circumstances, many more surgeons preferred to use jejunum as the ideal reconstruction organ. Being considered as the problematic and sophisticated surgical procedure, the widespread prevalence of jejunum interposition was precluded. Here we present a case of replacement of esophagus by free jejunum with long term survival.
In this case, a small part of cervical esophagus was injured after thyroid resection. To replace this short part of injured esophagus, stomach, jejunum, and colon could be the potential choice. The stomach was not selected because all distal part of esophagus under injured part should be resected if replaced by stomach which could do much more trauma to the patient. Neither did the colon be selected as it got the features of regurgitation, an unpleasant sensation of fullness, and the need for remedial operation. So free jejunum interposition became our preferred choice.
Case presentation
Thyroidectomy was performed for a 74-year-old female. On post-operative day 1, undigested liquid foods drained out of cervical wound after having meal. Fistula of cervical esophagus was suspected and exploratory surgery was performed on the same day. Two centimeters defect was noticed on esophagus just under cricoid cartilage. Planning to make a fixation, the injured portion of esophageal was freed firstly. Obvious inflammation could be observed around defect region of esophageal. After failed in trying to fix the defect, open drainage of cervical wound was performed. Distal end of the injured esophageal was sealed. Jejunostomy were also performed subsequently.
Enteral nutrition was used for the next 9 months before esophageal reconstruction. One month before savage surgery, this patient was hospitalized and accepted daily cleaning of the wound. Preoperative esophagoscopy showed stricture of esophagus 2-cm from the orifice. After infection of cervical wound was controlled, the savage surgery was put on schedule. Liquid diet was administered the day before operation.
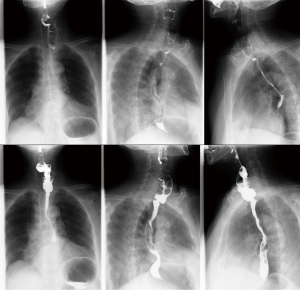
As Figure 1 showed, a hemimanubriectomy with resection of the head of left clavicle is performed to allow space at the thoracic inlet. Esophageal bed was used to place the free jejunum. Median incision of abdominal was used in harvesting jejunum.
During reconstruction, after resection of 3-cm constrictive esophagus, the resected part was then replaced with 5-cm free vascular pedicled jejunum. The proximal part of jejunum which was 20 cm away from the Treiz lig was harvested for anastomosis. End-to-end and end-to-side anastomosis were used for esophagus jejunum anastomosis. Interrupted suture technique was used in digest tract anastomosis. Running suture technique and end-to-side anastomotic way was used in vascular anastomosis. An experienced microvascular surgeon performed all of the vascular anastomosis. The transverse cervical artery was used for the arterial inflow. For outflow, the external jugular vein was used for drainage of the mesenteric vein. Before the proximal intestine-to-esophagus anastomosis is created, a portion of the superior part of the bowel that was disconnected from the gastrointestinal tract but left attached to blood supply was externalized through the neck incision to monitor the viability of the augmented conduit. The total operation time was 380 minutes and the intraoperative blood loss was 300 mL.
Four days after reconstruction, the externalized bowel was resected and its proximal end was ligated. Liquid food was administered 10 days after reconstruction. The patient was discharged 15 days after reconstruction. Annual follow-up was carried out. Only minor late operation complication (anastomotic stricture) occurred during 13 years of annual follow-up (Figure 2).
Discussion
Esophageal reconstruction in patient without a suitable stomach is one of the most challenging work that a thoracic surgeon could ever meet. Either the jejunum or the colon could be employed as a substitute for the gastric tube in replacement of esophagus (3). Studies have proposed several disadvantages of colon interposition when compared with jejunum. The development of conduit redundancy impairs food transit, leading to regurgitation, an unpleasant sensation of fullness, and the need for remedial operation (1,2). Colonic necrosis, thought to result from arterial or venous insufficiency at the distal part of the graft, carries a significant mortality risk (4).
The jejunum is uniquely suitable for esophageal reconstruction because it is relatively abundant and typically free of disorder. Also it has intrinsic peristalsis and its lumen size is much similar to that of esophagus (5). As reported, the jejunum could be interpositioned either pedicled, super charged, or free segment. The pedicled jejunum is limited with respect to its extension length due to poor connection of marginal vessels, and it was therefore used for lower anastomosis (3). Many years have been taken in development of full-length esophageal reconstruction. The super charged pedicled jejunum and free segment interposition could be suitable for replacement of any segment of esophagus. In literature, Longmire and colleagues were the first to present a long-segment jejunal interposition with microvascular anastomosis (6). After that, Androsov used the reported Longmire’s vascular augmentation technique in 11 patients in 1956 (7). In 2005, Ascioti et al. reported the first large series of pedicled jejunal interposition to replace the entire esophagus in cancer patients by using the “super-charging” technique (5). However, the prevalence of these surgical procedures was precluded because of the complexity of vascular microanastomosis in spite of these early reports.
Indications for cervical esophageal reconstruction mainly include traumatic injury or dysfunction caused by congenital disorders, corrosive injury, or radiation damage (8). Furthermore, reconstruction may be indicated as salvage surgery of accidental injury during thyroidectomy just as showed in our report. In this case, we experienced a savage surgery for esophageal injury patients. Nine months after first drainage operation, replacement was successfully performed. The scar caused by long term infection and inflammation make the replacement procedure much more sophisticated than regular free jejunum interposition. To minimize the influence of physiological function of digestive system, we used free jejunum during this salvage reconstruction procedure.
Several major complications would commonly see post-operatively such as aspiration, pneumonia, and recurrent laryngeal nerve injury. However, compared with aspiration and pneumonia, non-occlusive mesenteric ischemia was the most dreadful and devastating complication as it could probably lead to the failure of graft. To avoid this devastating procedure, we resected part of the bony structures of the thoracic orifice to release the space for mesenteric vessel. And a portion of disconnected bowel with blood supply was externalized to monitor the viability of the augmented conduit. Four days after operation the externalized part bowel was resected. No early postoperative complication occurred and this patient was discharged 15 days postoperatively. The proficient microvascular skill and nerve preservation skill played a key role in this case. Minor late operation complication (anastomotic stricture) occurred in this patient and it was resolved under gastroscopy during follow-up.
Free jejunum interposition was the toughest job among esophageal operations. While with delicate multiple-disciplinary cooperation, skilled surgeon’s experience and critical postoperative care, it could be handled in experienced thoracic surgeons and get satisfied early and late postoperative outcomes. We recommend that such major surgeries be used in critical selected patients.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
References
- Urschel JD. Late dysphagia after presternal colon interposition. Dysphagia 1996;11:75-7. [Crossref] [PubMed]
- Cense HA, Visser MR, van Sandick JW, et al. Quality of life after colon interposition by necessity for esophageal cancer replacement. J Surg Oncol 2004;88:32-8. [Crossref] [PubMed]
- Doki Y, Okada K, Miyata H, et al. Long-term and short-term evaluation of esophageal reconstruction using the colon or the jejunum in esophageal cancer patients after gastrectomy. Dis Esophagus 2008;21:132-8. [Crossref] [PubMed]
- Briel JW, Tamhankar AP, Hagen JA, et al. Prevalence and risk factors for ischemia, leak, and stricture of esophageal anastomosis: gastric pull-up versus colon interposition. J Am Coll Surg 2004;198:536-41. [Crossref] [PubMed]
- Ascioti AJ, Hofstetter WL, Miller MJ, et al. Long-segment, supercharged, pedicled jejunal flap for total esophageal reconstruction. J Thorac Cardiovasc Surg 2005;130:1391-8. [Crossref] [PubMed]
- Longmire WP Jr, Ravitch MM. A new method for constructing an artificial esophagus. Ann Surg 1946;123:819-35. [Crossref]
- Binford RT Jr, Cheraskin E. Clinical problems related to the tongue. Pediatr Clin North Am 1956.919-32. [PubMed]
- Kim Evans KF, Mardini S, Salgado CJ, et al. Esophagus and hypopharyngeal reconstruction. Semin Plast Surg 2010;24:219-26. [Crossref] [PubMed]



