Sufficient myocardial protection of del Nido cardioplegia regardless of ventricular mass and myocardial ischemic time in adult cardiac surgical patients
Introduction
Del Nido (DN) cardioplegia has been developed to protect vulnerable immature cardiomyocytes; DN solution contains various additives including magnesium and lidocaine, which inhibit calcium accumulation in myocytes and prevent ischemia-reperfusion injury after cardiac surgery (1). With this advantage and single dose property, the DN formula has been widely used during pediatric cardiac surgery with favorable results (2-5). However, its use in the field of adult cardiac surgery are not popular yet (6-8).
The aims of this study were (I) to evaluate efficiency of DN cardioplegic solution (CPS) according to the ventricular mass and ischemic time and (II) to compare early results after surgery using DN CPS with those using a blood type CPS in adult cardiac surgical patients.
Methods
Patient characteristics
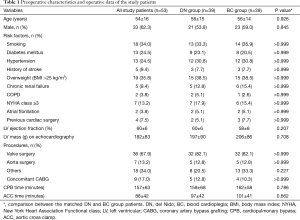
The study protocol was reviewed by the Institutional Review Board and was approved as a minimal risk retrospective study (Approval Number: 1511-022-715), which did not require individual consent based on the institutional guidelines for waiving consent. From July 2014 to December 2015, a total of 238 patients underwent surgery under cardioplegic arrest using DN (n=70) or blood type (n=168) cardioplegia. Among 70 patients with DN cardioplegia, 17 patients who underwent arrhythmia surgery using cryoablation, which affects the release of the myocardial enzyme, were excluded and 53 patients (male:female =33:20) were enrolled in the present study. Mean age at the operation was 54±16 years (Table 1). To prove non-inferior results of the DN cardioplegia, study patients were matched with patients who underwent surgery using blood type cardioplegia during the study period and results were compared. Propensity score matching yielded 39 pairs of patients with DN and blood-type cardioplegia (DN and BC groups, respectively). There were no statistically significant differences in the patient characteristics between the two matched groups (Table 1).
Full table
Surgical procedures and operative data
The surgeries included isolated or combination of valvular heart surgery (n=36), aorta replacement surgery (n=7), and other operations such as congenital heart disease or a tumor (n=18). Concomitant coronary artery bypass graft surgery was performed in nine patients. The cardiopulmonary bypass (CPB) and aortic cross clamp (ACC) times were 157±63 and 88±42 minutes, respectively. In the matched two groups, there were no significant differences in surgical procedures and operative data (Table 1).
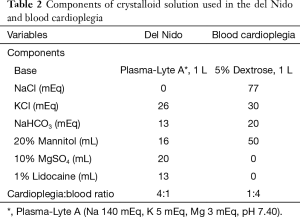
Use of cardioplegia
DN cardioplegia was used as a 4:1 mixture of the DN solution and the patient’s blood (1). Blood type cardioplegia was used as a 4:1 mixture of the patient’s blood and crystalloid (Table 2). Cardioplegia was administered through antegrade route, retrograde route or both as appropriate. DN cardioplegia was infused with an initial dose of 1,000–1,500 mL, and an additional dose of 500 mL was re-infused when the ACC time exceeded 90 minutes. In the BC group, an initial dose of 20 mL/kg was used followed by additional doses of 10 mL/kg every 20 minutes or when the myocardial temperature was over 15 °C.
Full table
Evaluation of the outcomes
The primary end-point was the peak level and changes of troponin I (TnI). The patients underwent routine laboratory tests including TnI serum levels in the preoperative period, and at immediately, 6 hours, 1 day, 2 days and 3 days after surgery. The impact of ACC time, left ventricular mass (LVM) and other factors on peak level of TnI was analyzed.
The secondary end-points were clinical outcomes including operative mortality and postoperative complications. Operative mortality was defined as any death within 30 days after surgery or during the same hospitalization. The occurrence of any short runs of atrial fibrillation before discharge was considered as new onset postoperative atrial fibrillation. The respiratory complications included postoperative pneumonia, prolonged ventilator support and a need for tracheostomy for any reason. Postoperative acute kidney injury was defined as an increase of >50% in serum creatinine level from the preoperative value or a need for renal replacement therapy irrespective of the serum creatinine level. Low cardiac output syndrome was defined as a cardiac index <2.0 L/min/m2 or a systolic arterial pressure <90 mmHg requiring inotropic support (dopamine or dobutamine) of >5 μg/kg/min.
The primary and secondary end-points were compared between the two matched groups.
Statistical analysis
The statistical analysis was performed using the SPSS software package version 22 (IBM Corp., Armonk, NY, USA). The data are expressed as the mean ± standard deviations, median with ranges, or proportions. The factors including the LVM and ACC time were analyzed using linear regression models to evaluate the association of those with the peak TnI level in the 53 study patients.
To match patients who underwent surgery with different cardioplegia, a propensity score of receiving DN cardioplegia was calculated using 17 preoperative and intraoperative variables. The variables used in the estimation of the propensity score included the following: (I) age; (II) sex; (III) smoking; (IV) diabetes mellitus; (V) hypertension; (VI) history of stroke; (VII) overweight; (VIII) chronic renal failure; (IX) New York Heart Association functional class (NYHA) ≥3; (X) chronic obstructive pulmonary disease; (XI) atrial fibrillation; (XII) previous cardiac surgery; (XIII) left ventricular ejection fraction; (XIV) LVM; (XV) type of surgery; (XVI) CPB time; (XVII) ACC time. The P value of the Hosmer-Lemeshow test was statistically insignificant (P=0.803) and the c statistic of the propensity score model was 0.866. The 1:1 propensity score matching extracted 39 patients from each group. For the comparison of the categorical and continuous variables between the matched groups, McNemar’s test and paired t-test were performed. Repeated measure analysis of variance was used to compare the longitudinal data between the two groups.
A P value <0.05 was considered statistically significant.
Results
Use of cardioplegia
DN CPS was infused with an initial dose of 1,126±221 mL as antegrade (n=38), retrograde (n=12) or both (n=3). Thirty-eight patients received a single dose infusion with an ACC time of 68±24 minutes; 2 of 38 patients had an ACC time over 90 minutes with a single dose infusion (97 and 144 minutes). An additional 500 mL of cardioplegia was re-infused in 15 patients at 91±9 minutes after the ACC. The average volume infused was 1,340±449 mL. After the release of the ACC, spontaneous defibrillation was achieved in 50 of 53 patients (94.3%).
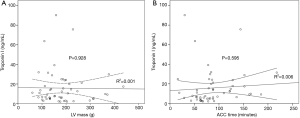
Evaluation of the TnI level
Median TnI level at preoperative period, and immediate, 6 hours, 1 day, 2 days and 3 days after surgery were 0.01 ng/mL (range, 0.01–0.47 ng/mL), 4.3 ng/mL (range, 0.1–43.7 ng/mL), 9.0 ng/mL (range, 1.0–75.7 ng/mL), 6.4 ng/mL (range, 1.2–90.2 ng/mL), 3.3 ng/mL (range, 0.5–57.6 ng/mL) and 1.5 ng/mL (range, 0.1–33.5 ng/mL), respectively. In most patients, the TnI level was highest at 6 (n=27) or 24 hours (n=18) after surgery. The median peak level of TnI after surgery was 9.8 ng/mL (range, 2.0–90.2 ng/mL). The linear regression models demonstrated that neither the LVM (β ± standard error for 1 g increment =−0.003±0.030; P=0.928) nor ACC time (β ± standard error for 1 min increment =0.032±0.059; P=0.595) were associated with peak level of TnI after surgery (Figure 1). In addition, no significant factor related with the peak level of TnI after surgery was found. Additionally, in 38 patients who received single dose infusion, the LVM and ACC time were not associated with the peak level of TnI (β ± standard error for 1 g increment =0.004±0.048; P=0.936, and β ± standard error for 1 min increment =0.121±0.142; P=0.399, respectively).
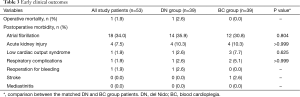
Early clinical outcomes
Early mortality occurred in 1 patient (1.9%). The patient died of unresolved bacteremia after valvular heart surgery for infective endocarditis. Postoperative complications included atrial fibrillation (n=18, 34.0%), acute kidney injury (n=4, 7.5%), low cardiac output syndrome (n=1, 1.9%), and respiratory complications (n=1, 1.9%) (Table 3). No one suffered from perioperative myocardial infarction.
Full table
Results of the propensity score matching analysis
The number of cardioplegic infusion, and infusion volumes were smaller in the DN than BC groups. After release of ACC, spontaneous defibrillation was achieved more frequently in the DN group than in the BC group (37/39, 94.9% vs. 12/39, 30.8%; P<0.001) (Table 4).
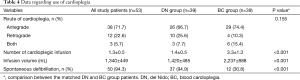
Full table
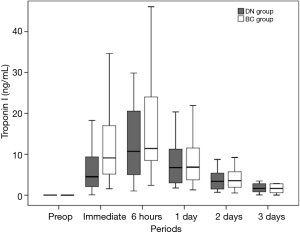
The peak level of TnI in the DN group was lower than that of BC group, although not statistically significant (the median peak level of TnI in the DN group and the BC group =9.8 ng/mL (range, 2.0–75.7 ng/mL) and 16.0 ng/mL (range, 3.5–153.9 ng/mL), respectively; P=0.085). The serial changes in TnI up to 3 days after surgery were similar between the two groups (P=0.959) (Figure 2). There were also no differences in the early outcomes including mortality and postoperative complication rates of the two propensity score-matched groups (Table 3).
Discussion
This study demonstrated two main findings. First, in adult cardiac patients, stable cardiac arrest could be maintained using the DN cardioplegia, irrespective of the LVM and ACC time, with the advantages of fewer dose and small volume properties. Second, DN cardioplegia is as effective as intermittent blood cardioplegia (BC) for adult cardiac patients in terms of myocardial protection and early clinical outcomes.
DN cardioplegia was initially developed to protect the immature heart, which is vulnerable to reperfusion injury because of its intolerance of a high level of intracellular calcium after an ischemic period (1). It contains polarizing agents, such as magnesium and lidocaine, which slow the rate of energy consumption and intracellular accumulation of the detrimental calcium ion, and thus lead stable arrest of cardiac myocytes with a reduced number and volume of infusions. Other components include mannitol to scavenge free radicals and reduce myocardial edema, and sodium bicarbonate to maintain the intracellular pH (1). Previous studies demonstrated that aged hearts are also susceptible to ischemia-reperfusion injury because of altered Ca2+ homeostasis. Using animal models, these studies confirmed the efficacy of DN cardioplegia in elderly (9-11). However, DN cardioplegia has not been widely used in adult cardiac surgery and only few studies have evaluated its efficacy for adult cardiac patients by comparing the results of surgery in DN and BC groups. Previous studies have demonstrated that DN cardioplegia could be a good alternative to BC for adult cardiac surgeries, such as redo-aortic valve surgery, coronary artery bypass grafting (CABG) and isolate valve surgery, in terms of the operative mortality and postoperative event rates (6-8).
Because of single dose and small volume properties of the DN cardioplegia, there might be two concerns when using it in complex adult cardiac surgical patients: Is it efficient for adult hearts with increased myocardial mass? Does it effectively protect the myocardium when the ACC time is prolonged? To answer these questions, we evaluated the association between the peak level of TnI, and the LVM and ACC time using linear regression analyses. Although the number of patients was relatively small, we found no trend of a correlation between the peak TnI level, and the LVM and ACC time. The myocardial TnI level was also not associated with the LVM and ACC time in the 38 patients who received a single dose of DN cardioplegia. These findings are different from results the of the previous study (8), which demonstrated the association between longer ischemic times and higher troponin T levels in both DN and BC group patients. This discrepancy might be partly because of the following reasons: (I) in the previous study, the troponin level was basically measured at a single time point (6 to 12 hours) compared with the repeated measures used in the present study; and (II) the operations were performed under normothermic CPB compared with hypothermic CPB in our study.
In the present study, we compared the peak level and serial changes of TnI in the DN group with the BC group as a marker of myocardial injury as well as the early clinical results. To adjust the baseline differences of the two groups, the propensity score matching was performed by including 17 preoperative and intraoperative variables. There were no differences in peak level and serial changes of myocardial TnI up to 3 days after surgery and the early clinical outcomes were also similar between the two groups.
As in previous studies, spontaneous defibrillation was more frequently achieved in the DN group than BC group, and only less than 10% of the DN group patients needed electrical defibrillation, which could be detrimental to cardiomyocytes (12). Reduced calcium ion accumulation in cardiomyocytes during arrest might prevent myocardial injury and ventricular fibrillation after reperfusion (1,12).
This study has several limitations that must be recognized. First, this study was performed with a retrospective design. Second, different patient characteristics might affect the study results, although the propensity score analyses were performed to minimize this effect. Finally, the number of patients enrolled in the study was relatively small to draw definite conclusions.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study protocol was reviewed by the Institutional Review Board and was approved as a minimal risk retrospective study (Approval Number: 1511-022-715), which did not require individual consent based on the institutional guidelines for waiving consent.
References
- Matte GS, del Nido PJ. History and use of del Nido cardioplegia solution at Boston Children's Hospital. J Extra Corpor Technol 2012;44:98-103. [PubMed]
- Charette K, Gerrah R, Quaegebeur J, et al. Single dose myocardial protection technique utilizing del Nido cardioplegia solution during congenital heart surgery procedures. Perfusion 2012;27:98-103. [Crossref] [PubMed]
- Kotani Y, Tweddell J, Gruber P, et al. Current cardioplegia practice in pediatric cardiac surgery: a North American multiinstitutional survey. Ann Thorac Surg 2013;96:923-9. [Crossref] [PubMed]
- O'Brien JD, Howlett SE, Burton HJ, et al. Pediatric cardioplegia strategy results in enhanced calcium metabolism and lower serum troponin T. Ann Thorac Surg 2009;87:1517-23. [Crossref] [PubMed]
- Sinha P, Zurakowski D, Jonas RA. Comparison of two cardioplegia solutions using thermodilution cardiac output in neonates and infants. Ann Thorac Surg 2008;86:1613-9. [Crossref] [PubMed]
- Sorabella RA, Akashi H, Yerebakan H, et al. Myocardial protection using del nido cardioplegia solution in adult reoperative aortic valve surgery. J Card Surg 2014;29:445-9. [Crossref] [PubMed]
- Yerebakan H, Sorabella RA, Najjar M, et al. Del Nido Cardioplegia can be safely administered in high-risk coronary artery bypass grafting surgery after acute myocardial infarction: a propensity matched comparison. J Cardiothorac Surg 2014;9:141. [Crossref] [PubMed]
- Mick SL, Robich MP, Houghtaling PL, et al. del Nido versus Buckberg cardioplegia in adult isolated valve surgery. J Thorac Cardiovasc Surg 2015;149:626-634; discussion 634-6. [Crossref] [PubMed]
- O'Blenes SB, Friesen CH, Ali A, et al. Protecting the aged heart during cardiac surgery: the potential benefits of del Nido cardioplegia. J Thorac Cardiovasc Surg 2011;141:762-70. [Crossref] [PubMed]
- Govindapillai A, Hua R, Rose R, et al. Protecting the aged heart during cardiac surgery: use of del Nido cardioplegia provides superior functional recovery in isolated hearts. J Thorac Cardiovasc Surg 2013;146:940-8. [Crossref] [PubMed]
- Govindapillai A, Hancock Friesen C, O'Blenes SB. Protecting the aged heart during cardiac surgery: single-dose del Nido cardioplegia is superior to multi-dose del Nido cardioplegia in isolated rat hearts. Perfusion 2016;31:135-42. [Crossref] [PubMed]
- Ristagno G, Wang T, Tang W, et al. High-energy defibrillation impairs myocyte contractility and intracellular calcium dynamics. Crit Care Med 2008;36:S422-7. [Crossref] [PubMed]


