Esophageal cancer incidence and mortality in China, 2009
Introduction
Esophageal cancer is the fourth most common cause of cancer death, while the mortality rate was 15.21 per 10,000 (11.19% of the total cancer death) according to the data from The Third National Causes of Death Sampling Survey [2004-2005] (1). Esophageal cancer mortality rates have decreased somewhat over the past three decades with the improvement of its socio-economic status and lifestyle (1). However, esophageal cancer remains prevalent in rural areas and in males (2). Accurate population-based statistics of esophageal cancer are the basis for policy makers and researchers for effective cancer prevention and control.
Material and methods
Data source
National Central Cancer Registry (NCCR) of China was the governmental authority affiliated to Bureau of Disease Control, Ministry of Health, in charge of cancer data collection, evaluation and publication from population-based cancer registries nationwide. All new cancer cases diagnosed in 2009 were reported to cancer registries from all hospitals, community health centers and the other departments, including centers of township medical insurance and the New-type Rural Cooperative Medical System. The death record database was linked and matched with cancer registration database for identifying cancer deaths and supplementing missed cases.
Until June 1st, 2012, there were 104 cancer registries (46 cities and 58 counties) from 27 provinces reporting cancer registration data to NCCR. The overall population coverage was 109,476,347, accounting for 8.20% of the whole population. The cancer registries coded cancer site and histology by the International Classification of Diseases (ICD) for Oncology, third edition and ICD-10. Invasive cases of esophageal cancer (C15) were retrieved from the overall cancer database and analyzed. Demographic information was provided by national statistics bureau.
Quality control
Based on “Guideline of Chinese Cancer Registration” and the standard of data inclusion in “Cancer Incidence in Five Continents Volume IX”, cancer registration data were evaluated by the quality indicators of proportion of morphological verification (MV%), percentage of cancer cases identified with death certification only (DCO%) and mortality to incidence ratio (M/I) (3-5). Generally, data with DCO% less than 20%, an overall MV% of more than 55%, and M/I between 0.55-0.95 were considered acceptable.
Statistical analysis
Crude incidence and mortality rates of esophageal cancer were calculated stratified by sex, area and for 19 age groups (0-, 1-4, 5-9, … 80-84, 85+ years). China sensus in 1982 and Segi’s world population were applied for age standardized rates. The cumulative risk of developing or dying from cancer before 75 years (in the absence of competing causes of death) was calculated and presented as a percentage. Software including MS-FoxPro, MS-Excel, IARCcrgTools issued by IARC and IACR were used for data checkup. SAS software was used to calculate the incidence and mortality rates.
Results
A total of 72 population-based cancer registries with qualified cancer statistics were included in the study. The population covered by these cancer registries was 85,470,522, including 43,231,554 males and 42,238,968 females, accounting for 6.40% of the whole population. Among them, 31 registries were from urban areas, covering a total of 57,489,009 population. And 41 registries were from rural areas, covering a total of 27,981,513 population. The MV%, DCO%, and M/I ratio for the national pooled data were 50.76%, 4.88% and 0.85 respectively. In urban areas, the MV%, DCO%, and M/I ratio were 55.03%, 4.71% and 0.86 respectively. In rural areas, they were 38.68%, 5.35% and 0.84. There were 18,924 new cases diagnosed with esophageal cancer in 2009. Of them, 13,161 were males and 5,763 were females. The number of overall cancer deaths was 14,337, including 10,067 males and 4,270 females. The detailed information for the covering population, incident cases and the cancer deaths of esophageal cancer in each cancer registry was shown in Table 1.
Table 1
| Registry | Urban =1 Rural =2 | Population
|
New cancer cases
|
Cancer death
|
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Both | Male | Female | Both | Male | Female | Both | Male | Female | ||
| Beijing | 1 | 7,645,186 | 3,859,586 | 3,785,600 | 676 | 532 | 144 | 586 | 449 | 137 |
| Qianxi | 2 | 361,312 | 182,138 | 179,174 | 90 | 78 | 12 | 48 | 40 | 8 |
| Shexian | 2 | 394,944 | 205,168 | 189,776 | 328 | 221 | 107 | 273 | 181 | 92 |
| Cixian | 2 | 634,333 | 322,621 | 311,712 | 688 | 407 | 281 | 506 | 311 | 195 |
| Baoding | 1 | 948,612 | 478,051 | 470,561 | 103 | 73 | 30 | 100 | 59 | 41 |
| Yangquan | 1 | 683,165 | 346,023 | 337,142 | 153 | 103 | 50 | 126 | 85 | 41 |
| Yangcheng | 2 | 383,165 | 192,119 | 191,046 | 357 | 226 | 131 | 239 | 159 | 80 |
| Chifeng | 1 | 1,203,006 | 613,725 | 589,281 | 72 | 62 | 10 | 57 | 47 | 10 |
| Shenyang | 1 | 3,497,815 | 1,722,976 | 1,774,839 | 331 | 284 | 47 | 247 | 208 | 39 |
| Dalian | 1 | 2,266,224 | 1,136,772 | 1,129,452 | 214 | 193 | 21 | 145 | 130 | 15 |
| Zhuanghe | 2 | 915,660 | 461,826 | 453,834 | 61 | 56 | 5 | 41 | 35 | 6 |
| An’shan | 1 | 1,471,775 | 731,916 | 739,859 | 120 | 91 | 29 | 92 | 84 | 8 |
| Benxi | 1 | 955,409 | 475,113 | 480,296 | 99 | 89 | 10 | 70 | 61 | 9 |
| Dandong | 1 | 767,011 | 378,794 | 388,217 | 48 | 39 | 9 | 39 | 34 | 5 |
| Donggang | 2 | 640,853 | 323,798 | 317,055 | 34 | 23 | 11 | 34 | 29 | 5 |
| Dehui | 2 | 943,395 | 479,486 | 463,909 | 28 | 21 | 7 | 19 | 13 | 6 |
| Yanji | 2 | 440,957 | 215,260 | 225,697 | 23 | 21 | 2 | 17 | 17 | 0 |
| Daoli District,Harbin | 1 | 713,264 | 351,071 | 362,193 | 69 | 62 | 7 | 39 | 35 | 4 |
| Nangang District,Harbin | 1 | 1,020,233 | 508,921 | 511,312 | 56 | 44 | 12 | 53 | 47 | 6 |
| Shangzhi | 2 | 616,046 | 314,864 | 301,182 | 51 | 43 | 8 | 27 | 24 | 3 |
| Shanghai | 1 | 6,181,334 | 3,084,496 | 3,096,838 | 504 | 351 | 153 | 521 | 355 | 166 |
| Jintan | 2 | 545,000 | 262,407 | 282,593 | 283 | 199 | 84 | 223 | 161 | 62 |
| Suzhou | 1 | 2,392,087 | 1,183,716 | 1,208,371 | 549 | 382 | 167 | 318 | 231 | 87 |
| Haian | 2 | 936,785 | 463,612 | 473,173 | 708 | 445 | 263 | 560 | 370 | 190 |
| Qidong | 2 | 1,114,951 | 548,805 | 566,146 | 133 | 89 | 44 | 136 | 90 | 46 |
| Haimen | 2 | 1,016,228 | 501,407 | 514,821 | 191 | 134 | 57 | 166 | 114 | 52 |
| Lianyungang | 1 | 886,862 | 452,358 | 434,504 | 141 | 106 | 35 | 109 | 76 | 33 |
| Donghai | 2 | 1,117,858 | 579,751 | 538,107 | 285 | 219 | 66 | 240 | 182 | 58 |
| Guanyun | 2 | 1,015,229 | 534,502 | 480,727 | 301 | 200 | 101 | 280 | 198 | 82 |
| Chuzhou District, Huai’an | 1 | 1,174,877 | 609,088 | 565,789 | 1,120 | 662 | 458 | 758 | 435 | 323 |
| Huaiyin District, Huai’an | 1 | 900,027 | 465,502 | 434,525 | 624 | 419 | 205 | 368 | 245 | 123 |
| Xuyi | 2 | 759,450 | 388,180 | 371,270 | 398 | 275 | 123 | 235 | 154 | 81 |
| Jinhu | 2 | 352,292 | 176,689 | 175,603 | 216 | 125 | 91 | 165 | 102 | 63 |
| Sheyang | 2 | 965,817 | 494,682 | 471,135 | 444 | 280 | 164 | 364 | 228 | 136 |
| Jianhu | 2 | 805,465 | 410,369 | 395,096 | 527 | 305 | 222 | 412 | 276 | 136 |
| Dafeng | 2 | 724,147 | 363,326 | 360,821 | 348 | 224 | 124 | 303 | 204 | 99 |
| Yangzhong | 2 | 272,046 | 134,758 | 137,288 | 269 | 156 | 113 | 249 | 139 | 110 |
| Taixing | 2 | 1,128,840 | 613,199 | 515,641 | 615 | 386 | 229 | 518 | 336 | 182 |
| Hangzhou | 1 | 6,753,509 | 3,403,893 | 3,349,616 | 890 | 759 | 131 | 660 | 547 | 113 |
| Jiaxing | 1 | 509,367 | 253,819 | 255,548 | 64 | 55 | 9 | 54 | 45 | 9 |
| Jiashan | 2 | 382,475 | 189,692 | 192,783 | 67 | 49 | 18 | 64 | 52 | 12 |
| Haining | 2 | 653,957 | 322,969 | 330,988 | 74 | 57 | 17 | 63 | 52 | 11 |
| Shangyu | 2 | 771,321 | 383,462 | 387,859 | 139 | 128 | 11 | 135 | 119 | 16 |
| Xianju | 2 | 490,070 | 255,438 | 234,632 | 155 | 96 | 59 | 148 | 94 | 54 |
| Feixi | 2 | 858,895 | 449,882 | 409,013 | 397 | 299 | 98 | 220 | 162 | 58 |
| Maanshan | 1 | 633,477 | 323,834 | 309,643 | 131 | 98 | 33 | 115 | 89 | 26 |
| Tongling | 1 | 433,545 | 221,375 | 212,170 | 104 | 86 | 18 | 92 | 75 | 17 |
| Changle | 2 | 673,717 | 355,091 | 318,626 | 69 | 51 | 18 | 52 | 42 | 10 |
| Xiamen | 1 | 1,160,135 | 583,873 | 576,262 | 322 | 260 | 62 | 240 | 176 | 64 |
| Zhanggong District, Ganzhou | 1 | 420,759 | 212,159 | 208,600 | 36 | 32 | 4 | 31 | 25 | 6 |
| Linqu | 2 | 817,857 | 417,434 | 400,423 | 132 | 107 | 25 | 105 | 75 | 30 |
| Wenshang | 2 | 762,828 | 388,454 | 374,374 | 464 | 314 | 150 | 316 | 194 | 122 |
| Feicheng | 2 | 733,501 | 358,739 | 374,762 | 731 | 501 | 230 | 504 | 345 | 159 |
| Yanshi | 2 | 602,266 | 306,192 | 296,074 | 237 | 128 | 109 | 167 | 97 | 70 |
| Linzhou | 2 | 1,080,241 | 557,392 | 522,849 | 860 | 459 | 401 | 605 | 361 | 244 |
| Xiping | 2 | 858,002 | 434,899 | 423,103 | 260 | 145 | 115 | 190 | 108 | 82 |
| Wuhan | 1 | 4,832,174 | 2,484,622 | 2,347,552 | 435 | 337 | 98 | 350 | 288 | 62 |
| Yunmeng | 2 | 524,801 | 261,237 | 263,564 | 41 | 37 | 4 | 29 | 26 | 3 |
| Hengdong | 2 | 713,458 | 373,923 | 339,535 | 35 | 25 | 10 | 21 | 15 | 6 |
| Guangzhou | 1 | 3,968,216 | 2,014,580 | 1,953,636 | 302 | 246 | 56 | 249 | 208 | 41 |
| Sihui | 2 | 413,363 | 211,351 | 202,012 | 31 | 25 | 6 | 21 | 17 | 4 |
| Zhongshan | 1 | 1,468,391 | 732,333 | 736,058 | 140 | 127 | 13 | 120 | 110 | 10 |
| Liuzhou | 1 | 1,038,208 | 533,050 | 505,158 | 53 | 41 | 12 | 37 | 32 | 5 |
| Fusui | 2 | 444,332 | 236,000 | 208,332 | 17 | 15 | 2 | 12 | 11 | 1 |
| Jiulongpo District, Chongqing | 1 | 798,618 | 402,961 | 395,657 | 73 | 58 | 15 | 71 | 54 | 17 |
| Qingyang District,Chengdu | 1 | 534,701 | 277,154 | 257,547 | 70 | 55 | 15 | 52 | 44 | 8 |
| Ziliujing District,Zigong | 1 | 357,600 | 179,873 | 177,727 | 62 | 54 | 8 | 41 | 33 | 8 |
| Yanting | 2 | 610,103 | 316,499 | 293,604 | 573 | 366 | 207 | 478 | 306 | 172 |
| Jingtai | 2 | 233,609 | 119,953 | 113,656 | 21 | 19 | 2 | 17 | 15 | 2 |
| Liangzhou District,Wuwei | 1 | 990,583 | 524,276 | 466,307 | 493 | 367 | 126 | 286 | 223 | 63 |
| Xining | 1 | 882,839 | 439,175 | 443,664 | 113 | 88 | 25 | 64 | 50 | 14 |
| Xinyuan | 2 | 271,944 | 138,895 | 133,049 | 76 | 52 | 24 | 45 | 33 | 12 |
| Total | 85,470,522 | 43,231,554 | 42,238,968 | 18924 | 13161 | 5763 | 14337 | 10067 | 4270 | |
Incidence
The crude incidence rate for esophageal cancer was 22.14/100,000 in 2009, accounting for 7.74% of overall new cancer cases. It ranked fifth most common cancers in all cancer sites following cancers of lung, stomach, colon-rectum and liver. The age-standardized rates by China (CASR) population and by World population (WASR) were 10.88/100,000 and 14.81/100,000, respectively. Among the patients aged 0-74, the cumulative incidence rate was 1.88%.
Esophageal cancer occurred more often among men than women. For males, esophageal cancer was the fifth most common cancer and the crude incidence rate was 30.44/100,000, whereas the CASR and WASR were 15.62/100,000 and 21.27/100,000 respectively. For females, esophageal cancer was the sixth most common cancer and the crude incidence rate was 13.64/100,000, where as the CASR and WASR were 6.27/100,000 and 8.59/100,000. The crude incidence rate in urban areas (ranked sixth most common cancer) was 14.21/100,000 and it was lower than that in rural areas (ranked the third most common cancer with incidence rate of 38.44/100,000). After age standardization, incidence rate in urban (6.65/100,000 for WASR) was still much lower than that in rural (20.57/100,000 for WASR) (Table 2).
Table 2
| Area | Sex | New cases | Incidence (1/105)
|
CASRa (1/105) | WASRb (1/105) | Cumulative rate 0-74 (%) | Rank | |
|---|---|---|---|---|---|---|---|---|
| Rate | % | |||||||
| All areas | Both | 18,924 | 22.14 | 7.74 | 10.88 | 14.81 | 1.88 | 5 |
| Male | 13,161 | 30.44 | 9.57 | 15.62 | 21.27 | 2.69 | 5 | |
| Female | 5,763 | 13.64 | 5.39 | 6.27 | 8.59 | 1.09 | 6 | |
| Urban | Both | 8,167 | 14.21 | 4.68 | 6.65 | 9.07 | 1.13 | 6 |
| Male | 6,155 | 21.24 | 6.43 | 10.46 | 14.25 | 1.77 | 5 | |
| Female | 2,012 | 7.06 | 2.56 | 2.99 | 4.13 | 0.51 | 11 | |
| Rural | Both | 10,757 | 38.44 | 15.38 | 20.57 | 27.95 | 3.57 | 3 |
| Male | 7,006 | 49.18 | 16.78 | 27.22 | 37.05 | 4.69 | 3 | |
| Female | 3,751 | 27.31 | 13.31 | 13.97 | 19.03 | 2.44 | 3 | |
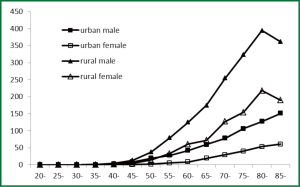
Age-specific incidence rates of esophageal cancer for both genders and areas were compared. Overall, the age-specific incidence rate was relatively low in subjects before 45 years old. However, the rate was dramatically increasing for patients after 45 years old, reaching peak for subjects of 80-84 years old (129.26/100,000). For males, subjects in the age group of 85 years or more had highest age-specific rates, whereas for females, subjects in the age group of 80-84 years old had highest rates. Generally, esophageal cancer among males had a higher age-specific incidence rate than those among females except for those in small age groups (<30 years old). Similarly, the age-standardized esophageal cancer rates in rural were generally higher than that in urban areas except for subjects in small age groups (Table 3, Figure 1).
Table 3
| Age group | All areas
|
Urban
|
Rural
|
||||||
|---|---|---|---|---|---|---|---|---|---|
| Both | Male | Female | Both | Male | Female | Both | Male | Female | |
| all | 22.14 | 30.44 | 13.64 | 14.21 | 21.24 | 7.06 | 38.44 | 49.18 | 27.31 |
| 0- | 0.32 | 0.31 | 0.34 | 0.52 | 0.50 | 0.55 | 0.00 | 0.00 | 0.00 |
| 1- | 0.04 | 0.07 | 0.00 | 0.00 | 0.00 | 0.00 | 0.10 | 0.18 | 0.00 |
| 5- | 0.03 | 0.00 | 0.06 | 0.00 | 0.00 | 0.00 | 0.07 | 0.00 | 0.14 |
| 10- | 0.02 | 0.04 | 0.00 | 0.00 | 0.00 | 0.00 | 0.05 | 0.10 | 0.00 |
| 15- | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| 20- | 0.04 | 0.08 | 0.00 | 0.04 | 0.07 | 0.00 | 0.05 | 0.09 | 0.00 |
| 25- | 0.10 | 0.11 | 0.08 | 0.06 | 0.08 | 0.04 | 0.18 | 0.18 | 0.18 |
| 30- | 0.29 | 0.30 | 0.27 | 0.23 | 0.23 | 0.24 | 0.38 | 0.42 | 0.34 |
| 35- | 1.16 | 1.90 | 0.41 | 0.76 | 1.27 | 0.25 | 1.96 | 3.15 | 0.74 |
| 40- | 3.75 | 5.97 | 1.49 | 2.46 | 4.29 | 0.59 | 6.36 | 9.33 | 3.31 |
| 45- | 10.81 | 17.60 | 3.77 | 7.79 | 13.89 | 1.44 | 17.62 | 26.04 | 8.98 |
| 50- | 26.87 | 42.16 | 11.11 | 17.67 | 31.03 | 3.95 | 50.30 | 70.23 | 29.48 |
| 55- | 47.05 | 69.05 | 24.91 | 28.44 | 46.92 | 10.18 | 91.51 | 120.35 | 61.21 |
| 60- | 76.78 | 108.85 | 44.60 | 42.92 | 68.08 | 18.27 | 149.91 | 193.69 | 103.68 |
| 65- | 95.43 | 132.43 | 59.28 | 58.17 | 87.47 | 30.36 | 169.64 | 218.28 | 119.39 |
| 70- | 114.04 | 159.64 | 72.12 | 67.14 | 101.43 | 36.16 | 226.79 | 295.38 | 161.08 |
| 75- | 120.96 | 161.26 | 85.15 | 74.1 | 103.44 | 47.79 | 242.67 | 314.20 | 180.66 |
| 80- | 129.26 | 175.08 | 92.90 | 86.2 | 119.83 | 58.86 | 238.22 | 321.77 | 175.85 |
| 85- | 105.19 | 163.46 | 68.32 | 74.91 | 122.02 | 44.34 | 184.20 | 277.87 | 128.74 |
Mortality
The crude mortality rate for esophageal cancer was 16.77/100,000 in 2009, accounting for 9.29% of cancer deaths in 2009. The CASR and WASR for mortality were 7.75/100,000 and 10.76/100,000, respectively. Among the patients with age of 0-74, the cumulative rate was 1.30%.
The mortality rate of esophageal cancer was much higher in males than in females. For males, the crude rate, CASR and WASR were 23.29/100,000, 11.42/100,000, and 15.86/100,000. For females, the crude rate, CASR and WASR were 10.11/100,000, 4.22/100,000 and 5.96/100,000. In urban areas, the crude rate, CASR and WASR were 10.59/100,000, 4.65/100,000 and 6.47/100,000. In rural areas, they were 29.47/100,000, 14.91/100,000 and 20.69/100,000, lower than those in urban areas (Table 4).
Table 4
| Area | Sex | Deaths | Mortality (1/105)
|
CASR (1/105) | WASR (1/105) | Cumulative rate 0-74 (%) | Rank | |
|---|---|---|---|---|---|---|---|---|
| Rate | (%) | |||||||
| All areas | Both | 14,337 | 16.77 | 9.29 | 7.75 | 10.76 | 1.30 | 4 |
| Male | 10,067 | 23.29 | 10.39 | 11.42 | 15.86 | 1.91 | 4 | |
| Female | 4,270 | 10.11 | 7.44 | 4.22 | 5.96 | 0.70 | 6 | |
| Urban | Both | 6,090 | 10.59 | 5.82 | 4.65 | 6.47 | 0.75 | 5 |
| Male | 4,580 | 15.80 | 7.07 | 7.39 | 10.27 | 1.19 | 5 | |
| Female | 1,510 | 5.30 | 3.80 | 2.04 | 2.91 | 0.33 | 7 | |
| Rural | Both | 8,247 | 29.47 | 16.57 | 14.91 | 20.69 | 2.52 | 4 |
| Male | 5,487 | 38.51 | 17.06 | 20.57 | 28.55 | 3.45 | 4 | |
| Female | 2,760 | 20.09 | 15.68 | 9.39 | 13.16 | 1.57 | 3 | |
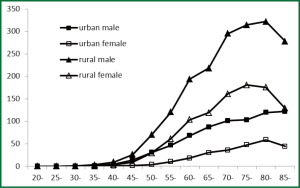
The mortality trend for esophageal cancer in different age groups was similar to the trend of incidence. Both for males and females, in urban and in rural, the mortality reached peak for subjects of 80-84 years old. (Table 5, Figure 2).
Table 5
| Age group | All areas
|
Urban
|
Rural
|
||||||
|---|---|---|---|---|---|---|---|---|---|
| Both | Male | Female | Both | Male | Female | Both | Male | Female | |
| all | 16.77 | 23.29 | 10.11 | 10.59 | 15.80 | 5.30 | 29.47 | 38.51 | 20.09 |
| 0- | 0.16 | 0.00 | 0.34 | 0.26 | 0.00 | 0.55 | 0.00 | 0.00 | 0.00 |
| 1- | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| 5- | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| 10- | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| 15- | 0.04 | 0.07 | 0.00 | 0.06 | 0.11 | 0.00 | 0.00 | 0.00 | 0.00 |
| 20- | 0.03 | 0.05 | 0.00 | 0.04 | 0.07 | 0.00 | 0.00 | 0.00 | 0.00 |
| 25- | 0.10 | 0.14 | 0.06 | 0.06 | 0.04 | 0.08 | 0.18 | 0.35 | 0.00 |
| 30- | 0.12 | 0.12 | 0.12 | 0.14 | 0.14 | 0.14 | 0.08 | 0.08 | 0.09 |
| 35- | 0.61 | 0.84 | 0.38 | 0.47 | 0.61 | 0.33 | 0.90 | 1.29 | 0.49 |
| 40- | 1.96 | 2.94 | 0.95 | 1.31 | 2.23 | 0.38 | 3.26 | 4.38 | 2.12 |
| 45- | 5.79 | 9.69 | 1.75 | 4.51 | 8.19 | 0.68 | 8.68 | 13.11 | 4.13 |
| 50- | 15.11 | 24.63 | 5.29 | 10.83 | 19.52 | 1.91 | 26.01 | 37.52 | 13.98 |
| 55- | 28.29 | 43.14 | 13.35 | 16.39 | 27.46 | 5.45 | 56.72 | 79.47 | 32.82 |
| 60- | 46.88 | 69.08 | 24.60 | 25.25 | 42.34 | 8.51 | 93.59 | 124.73 | 60.72 |
| 65- | 67.54 | 99.24 | 36.57 | 39.04 | 59.78 | 19.35 | 124.32 | 174.58 | 72.37 |
| 70- | 92.88 | 131.15 | 57.71 | 52.62 | 78.23 | 29.48 | 189.69 | 254.54 | 127.54 |
| 75- | 116.43 | 165.97 | 72.40 | 71.59 | 106.39 | 40.37 | 232.88 | 323.57 | 154.27 |
| 80- | 145.31 | 200.47 | 101.54 | 86.70 | 127.31 | 53.67 | 293.60 | 394.67 | 218.17 |
| 85- | 139.91 | 207.10 | 97.39 | 96.26 | 151.22 | 60.58 | 253.82 | 361.38 | 190.12 |
Discussion
Cancer registry annual report provides updated cancer statistics in cancer registration areas in China (6-8). This paper analyzed incidence and mortality rates of esophageal cancer in 2009 of China, based on 72 population-based cancer registries’ data. Data shows that the crude incidence and mortality rate of esophageal cancer in registration areas were 22.14/100,000 and 16.77/100,000. The age-standardized incidence and mortality rates by World population were 14.81/100,000 and 10.76/100,000. Esophageal cancer was more common in males than in females, in urban areas than in rural areas. The most recent cancer statistics on esophageal cancer might provide basic information for esophageal cancer prevention and control.
Esophageal cancer retains its status of top 4th leading cause of cancer deaths and the fifth most common diagnosed cancer in China in 2009. The incidence rate of esophageal cancer relatively increased compared the data in 2003-2007 (19.34 per 10,000) (9). The time trend shown that incidence rates of esophageal cancer had been increasing, however, after age standardization, it kept decreasing in recent 10 years (10). Aging population is a major cause for the increasing burden of esophageal cancer in China and incident cases is predicted to increase (10).
Esophageal cancer is the result of both effect of environmental factors, and lifestyle is one of the most important influencing factors (11-16). However, the exact mechanism is still not clear. The risk factors of esophageal cancer are discrepant in different countries and regions. For example, in developed country smoking, alcohol drinking and Barrett esophagitis are main risk factors (17-20), and in developing country nitrosamine, mold pollution, lack of vitamin, unhealthy lifestyles and smoking are main risk factors (14). If the genetic background can not be changed, change the bad dietary habits and behavior patterns are the most effective prevention of esophageal cancer. Hence, we should carry out health education in population in the long run, and appeal keeping away from the risk factors of esophageal cancer.
Esophageal cancer has very poor prognosis because most tumors are asymptomatic until at advanced stage which are un-resectable with the intention of curing the patient. Promising results have been reported that screening with use of endoscopy may improve prognosis from esophageal cancer (21). It is expected that through primary and secondary prevention, the prevalence of the disease may be controlled in the future.
NCCR is the authoritative source of information on cancer incidence and mortality in China. NCCR collects and publishes these statistics from population-based registries. The population coverage is increasing year by year. Since 2009, the ministry of health built up more cancer registries and provided specific funding to support the development of cancer surveillance. Until the end of 2012, there were 222 cancer registries around China, covering 14% of the whole population. Notably, the new built-up cancer registries need at least 5-year time to ensure data quality and reliability.
The data provided here are the most up-to-date data on incidence and mortality, reflecting the only available population-based information on esophageal cancer of China. In our study, urban population coverage took great part in the overall population, therefore, the representativeness of the data needs to be explained with caution (22). Chinese government is still making effort to improve the quality of the cancer registration data especially in rural areas. The accuracy and representativeness of the population-based cancer statistics would be better in the future.
Acknowledgements
All staff from local cancer registries that have made a great contribution for providing their cancer registration database was acknowledged.
Disclosure: The authors declare no conflict of interest.
References
- Wei WQ, Yang J, Zhang SW, et al. Esophageal cancer mortality trends during the last 30 years in high risk areas in China: comparison of results from national death surveys conducted in the 1970’s, 1990’s and 2004-2005. Asian Pac J Cancer Prev 2011;12:1821-6. [PubMed]
- Guo B, Huang ZL. Esophageal cancer mortality trends in rural and urban China between 1987 and 2009. Asian Pac J Cancer Prev 2011;12:2105-10. [PubMed]
- Curado MP, Shin HR, Storm H, et al. Cancer Incidence in Five Continents, Vol. IX. IARC Scientific Publications No. 160. Lyon: IARC, 2007.
- Parkin DM. Comparability and quality control in cancer registration. IARC, 1994.
- Ferlay J, Burkhard C, Whelan S, et al. Check and Conversion Programs for Cancer Registries. IARC Technical Report No. 42. Lyon, 2005.
- National Office for Cancer Prevention and Control, National Center for Cancer Registry, Disease Prevnetion and Control Bureau, MOH. Chinese Cancer Registry Annual Report (2008). Beijing: Military Medical Science Press, 2009:9.
- National Office for Cancer Prevention and Control, National Center for Cancer Registry, Disease Prevnetion and Control Bureau, MOH. Chinese Cancer Registry Annual Report (2009). Beijing: Military Medical Science Press, 2010:6.
- National Office for Cancer Prevention and Control, National Center for Cancer Registry, Disease Prevnetion and Control Bureau, MOH. Chinese Cancer Registry Annual Report (2010). Beijing: Military Medical Science Press, 2011:2.
- Chen WQ, Zheng RS, Zhang SW, et al. Cancer Incidence and Mortality in China 2003-2007. China Cancer 2012;21:161-70.
- Zeng HM, Zheng RS, Zhang SW, et al. Analysis and prediction of esophageal cancer incidence trend in China. Zhonghua Yu Fang Yi Xue Za Zhi 2012;46:593-7. [PubMed]
- Wang AH, Sun CS, Li LS, et al. Genetic susceptibility and environmental factors of esophageal cancer in Xi’an. World J Gastroenterol 2004;10:940-4. [PubMed]
- Xing D, Tan W, Lin D. Genetic polymorphisms and susceptibility to esophageal cancer among Chinese population Oncol Rep 2003;10:1615-23. (review). [PubMed]
- Wu M, Van’t Veer P, Zhang ZF, et al. A large proportion of esophageal cancer cases and the incidence difference between regions are attributable to lifestyle risk factors in China. Cancer Lett 2011;308:189-96. [PubMed]
- Wang JB, Fan JH, Liang H, et al. Attributable causes of esophageal cancer incidence and mortality in China. PLoS One 2012;7:e42281. [PubMed]
- Wu M, Zhang ZF, Kampman E, et al. Does family history of cancer modify the effects of lifestyle risk factors on esophageal cancer? A population-based case-control study in China. Int J Cancer 2011;128:2147-57. [PubMed]
- Liu M, Su M, Tian DP, et al. Heredity, diet and lifestyle as determining risk factors for the esophageal cancer on Nanao Island in Southern China. Fam Cancer 2010;9:229-38. [PubMed]
- Vioque J, Barber X, Bolumar F, et al. Esophageal cancer risk by type of alcohol drinking and smoking: a case-control study in Spain. BMC Cancer 2008;8:221. [PubMed]
- Ishikawa A, Kuriyama S, Tsubono Y, et al. Smoking, alcohol drinking, green tea consumption and the risk of esophageal cancer in Japanese men. J Epidemiol 2006;16:185-92. [PubMed]
- Bonnin-Scaon S, Lafon P, Chasseigne G, et al. Learning the relationship between smoking, drinking alcohol and the risk of esophageal cancer. Health Educ Res 2002;17:415-24. [PubMed]
- Shaheen N, Ransohoff DF. Gastroesophageal reflux, barrett esophagus, and esophageal cancer: scientific review. JAMA 2002;287:1972-81. [PubMed]
- Murakami S, Hashimoto T, Noguchi T, et al. The utility of endoscopic screening for patients with esophageal or head and neck cancer. Dis Esophagus 1999;12:186-90. [PubMed]
- Li GL, Chen WQ. Representativeness of population-based cancer registration in China--comparison of urban and rural areas. Asian Pac J Cancer Prev 2009;10:559-64. [PubMed]