EBUS-TBNA by a new Fuji EBUS scope (with video)
Introduction
Since the introduction of transbronchial needle aspiration (TBNA) (1) and bronchoscopic lymph node mapping (2) by Wang, TBNA has been widely used worldwide (3). With development of equipment and technologies, the recently emerged ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) have become a more dependable and attractive TBNA procedure than conventional TBNA procedure. Many multicenter researches and meta-analysis has confirmed its high sensitivity, specificity, and accuracy (4-6). As it is well known, the direction of view of the current EBUS scope is 35-45 degrees forward oblique (6-8). This makes the manipulation of the scope difficult not only for a novice but also for an experienced bronchoscopist. “Training is mandatory for performing a successful and safe EBUS-TBNA”. The endoscopic view is interfered or totally lost in order to obtain an ultrasound view during TBNA biopsy (9). Ideally, it is desirable to maintain the endoscopic view while performing TBNA under ultrasound visualization. Here we report our experience of this possibility by a new EBUS scope made by Fuji in human and teaching model.
Materials and methods
Instrument used was Fuji EBUS scope (Fujifilm, Japan, EB-530US) which has an integrated convex transducer with a frequency of 5-12 MHz at the tip of the bronchoscope. The scope has a CCD (Charge Coupled Device) image chip technology with two light guides. The outer diameter of the insertion tube and the tip are 6.3 and 6.7 mm. It provides a 120 degrees field of view at a 10 degrees forward oblique angle. The Olympus 22 guage, 21 guage EBUS needle and the WANG® MW319, SW221 needle (ConMed, USA) could be used for TBNA.
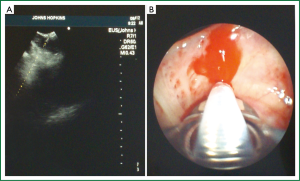
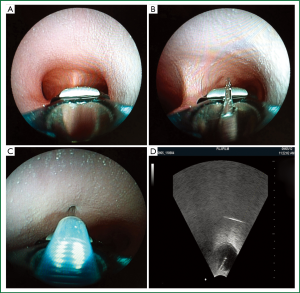
Before the trial, we tested the EB-530US scope on a Bronchial cast and an EBUS Teaching Phantom model (ATS laboratories, USA, EBUS-250) by a 19 guage (DT-W519) and 21 guage (DT-W421) needle (DeTian Medical, Changzhou, China) (Figure 1A-D) (Video 1). Two interventional pulmonologists and one gastrointestinal endoscopist performed EBUS-TBNA and transesophageal ultrasound needle aspiration (TENA), respectively.
Patient was a 59 year-old male with a mediastinum and hilar lymphadenopathy and history of asthma, diabetes, and allergic bronchopulmonary aspergillosis. He was referred for diagnosis by EBUS-TBNA. Conventional TBNA (C-TBNA) with an Olympus 2.2 mm lumen scope and MW-319 needle at station 7 (sub-carina, IASLC) (10) was performed followed by an EBUS -TBNA with a Fuji scope and Olympus 22 g EBUS needle (Video 1). Two punctures were made with standard method of C-TBNA and EBUS-TBNA.
Results
Using this new EBUS scope, vocal cords was easily passed. Every lobe was entered and examined up to the segmental bronchial openings. The specimen obtained by C-TBNA with a MW-319 needle was reported as granuloma by rapid on site cytological evaluation (ROSE). The specimen obtained by EBUS-TBNA was reported as lymphocyte with granuloma from the clot histology.
Discussion
One of the significant differences of EBUS scope is an angled side port exit at the distal tip of the working channel. The direction of the view is also angled to 35-45 degrees (Olympus-Pentax) forward oblique. As a result, the distal tip of the scope with the ultrasound probe is invisible.
Angled exit can afford the use of a stiffer needle, which is easier to control then the more flexible needle used in conventional TBNA. However, the angled view when scope is in straight position makes passage of the scope through the vocal cord and advancing the scope inside the air way much more difficult. In order to have a full view of bronchial lumen, scope tip has to be flexed backward and also it is invisible. Rather than advancing in scope with a full view the scope has to be advanced with a partial forward oblique view, like driving a car on the road by looking partially at the roof and the road. When TBNA is performed in order to obtain an ultrasound view, the tip of the scope has to be flexed forward and the endoscopic view is totally lost because the tip of scope is against the bronchial mucosa with the visual lens. This makes the procedure of TBNA by EBUS scope unnecessary complicated and difficult. Passing the larynx is a challenge and good examination of all airways is impossible. Almost all EBUS-TBNA are preceded the conventional bronchoscopic examination (9). Switching the scopes complicates the procedure and is more uncomfortable for conscious patients under the local anesthesia.
The direction of view of the Fuji EBUS scope is only 10 degrees, this eliminated the need of flexing the scope backward to visualize the lumen of the airway and makes the scope easier to manipulate as a standard scope. With a smaller (6.7 mm) outside diameter of the distal end of the scope and the 10 degrees of forward oblique view this scope is easier through the vocal cord and can be drives into lobar bronchus and visualize every segmental bronchus including both upper lobe (Figure 1A-C), and both superior segment of right and left lower lobe.
In one view, the distal end opening of the scope, the balloon, the distal end of the scope where the transducer located and the needle with the puncture site can all be visualized simultaneously with the ultrasound image without special effort (Figure 2A,B).
The exit angle of the working channel and diameter is similar to the Pentax scope. The needle was bent into a bow shape after first pass makes the subsequent biopsy more difficult. With further improvement to decrease the exit angle, enlarge the working lumen and decrease the exterior diameter of the scope, it has great potential of becoming a true hybrid scope to eliminate the need of two scopes, one for routine airways examination and one for EBUS-TBNA.
Because of the constant visualization by the bronchoscopic view with simultaneous ultrasound image, the Fuji EBUS scope will make EBUS-TBNA simple to do and easier to learn. The conventional TBNA expert will need minimal training to do EBUS TBNA, and may even liberate the EBUS expert from the dependency of EBUS scope. Importantly, our practice on the teaching model indicated that, using this new Fuji EBUS scope, EBUS-TENA is becoming easier and feasible, since it was regarded as the most accessibility to the mediastinum and hilar lymph nodes (11).
As we reported, continuous improvement of the equipment, instruments, and methodology is needed (11-13). In fact, the EBUS bronchoscope has already begun this evolution (14,15). The Olympus scope has increased the working channel from 2.0 to 2.2 mm. The Pentax scope has further reduced its outside diameter. Now with the innovation design of Fuji scope, it will make some radical changes in the technique of TBNA with or without EBUS. It will simplify EBUS-TBNA and deserve further evaluation and study.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Wang KP, Terry PB. Transbronchial needle aspiration in the diagnosis and staging of bronchogenic carcinoma. Am Rev Respir Dis 1983;127:344-7. [PubMed]
- Wang KP. Staging of bronchogenic carcinoma by bronchoscopy. Chest 1994;106:588-93. [PubMed]
- Harrow EM, Abi-Saleh W, Blum J, et al. The utility of transbronchial needle aspiration in the staging of bronchogenic carcinoma. Am J Respir Crit Care Med 2000;161:601-7. [PubMed]
- Tanner NT, Pastis NJ, Silvestri GA. Training for Linear Endobronchial Ultrasound among US Pulmonary/Critical Care fellowships: A survey of fellowship directors. Chest 2012; [Epub ahead of print]. [PubMed]
- Agarwal R, Srinivasan A, Aggarwal AN, et al. Efficacy and safety of convex probe EBUS-TBNA in sarcoidosis: a systematic review and meta-analysis. Respir Med 2012;106:883-92. [PubMed]
- Adams K, Shah PL, Edmonds L, et al. Test performance of endobronchial ultrasound and transbronchial needle aspiration biopsy for mediastinal staging in patients with lung cancer: systematic review and meta-analysis. Thorax 2009;64:757-62. [PubMed]
- Herth FJ, Eberhardt R. Actual role of endobronchial ultrasound (EBUS). Eur Radiol 2007;17:1806-12. [PubMed]
- Yasufuku K, Chiyo M, Sekine Y, et al. Real-time endobronchial ultrasound-guided transbronchial needle aspiration of mediastinal and hilar lymph nodes. Chest 2004;126:122-8. [PubMed]
- Nakajima T, Yasufuku K. The techniques of endobronchial ultrasound-guided transbronchial needle aspiration. Innovations (Phila) 2011;6:57-64. [PubMed]
- Rusch VW, Asamura H, Watanabe H, et al. The IASLC lung cancer staging project: a proposal for a new international lymph node map in the forthcoming seventh edition of the TNM classification for lung cancer. J Thorac Oncol 2009;4:568-77.
- Wang KP, Feller-Kopman D, Mehta A, et al. Endobronchial ultrasound and esophageal ultrasound: just because we can, does not necessarily mean we should. Chest 2011;140:271-2; author reply 272-3. [PubMed]
- Wang KP. Turner, Symanowski J. A Retrospective Review of Different Methods of Endobronchial Ultrasound-guided Transbronchial Needle Aspiration: A Preliminary Study. J Bronchology Interv Pulmonol 2011;18:94-6. [PubMed]
- Wang KP. Transbronchial needle aspiration and percutaneous needle aspiration for staging and diagnosis of lung cancer. Clin Chest Med 1995;16:535-52. [PubMed]
- Wang KP. EBUS-TBNA of lesions in mediastinum. J Thorac Dis 2010;2:124. [PubMed]
- Yarmus L, Feller-Kopman D, Browning R, et al. TBNA: Should EBUS be Used on all Lymph Node Aspirations? J Bronchology Interv Pulmonol 2011;18:115-7. [PubMed]