Thymic epithelial tumors in a worldwide perspective: lessons from observational studies
Progress in the understanding of thymic epithelial tumors (TET) are expected by improvement in tumor management as well as from discoveries in biological sciences. The data provided by the routine activity in health care of patients are as precious as the most advanced molecular investigation in tumor research. Therefore the recent JTD issue authored by the Chinese Alliance for Research in Thymomas (ChART), focused on thymic epithelial malignancy and covering a vast majority of clinical issues on these rare tumors, provides a summary of a longstanding experience on TET from the perspective of an authoritative scientific society/collaborative research group. Among the papers included in the ChART issue focusing on TET, an interesting paper from Zhu et al. is referring on the evaluation of clinicopathological features and outcome indicators in a TET series occurred at the Shanghai Chest Hospital (SCH) (1). The paper also discuss and compares the current findings with the previous results of a clinicopathological study on a 200 case cohort from the same Institution, published in 2002 (2). The “resection status” of the cases included in the study from Fang et al. was published in 2005 (3). Therefore we aim to comment here shortly the 2 case cohorts (the present and the historical cohort) together with the surgical report on the “R” status; in addition we considered for comparison other studies derived from other areas of the world, provided by single Institutions or based on large multicenter databases (DBs) dealing with clinicopathological and prognostic features in TET.
TET management at the Shanghai Chest Hospital
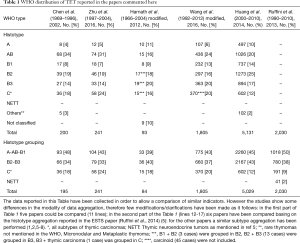
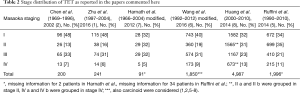
The present cohort (1) provides a detailed profile of 241 TET patients treated during 1997–2004, with a mean follow-up time of 6.4 to 14.5 years (median: 7.8 years). The centralized pathological review of the series has been performed on the basis of the 2004 WHO classification (4), involving the SCH Pathology Staff and one Pathologist (Prof. A.M.) who was also co-Author in the previous study (2). In the present cohort the WHO histological subtype, Masaoka stage and neoadjuvant treatment have been found independent determinants of overall survival (OS) in patients with thymomas and thymic carcinomas (TCs). It is worth to note that the two cohorts, the previous and the current, show very similar histotype distribution, with a slight increase in the TC percentage in the present cohort (Table 1) (24% vs. 18%). We noticed that in the current series no “combined” TET, such as described in the 2004 WHO classification, have been reported. Also the Stage distribution is rather similar in the two cohorts (Table 2). As an interesting feature, both series show a high percentage of cases detected in Stage I according to Masaoka (9): 48%. In Stage III and IV a definite increase of B2 and B3 thymoma was actually found in comparison with the other histological types, stage III disease representing the prevailing esordium of TC [Table 1 in the original article, (1)]. The “resection status” of the present series was compared with the “R” status from the previous cohort (3): the R0 was reached in similar percentage (88% vs. 85%) (1,2). In the historical cohort, including cases occurring from 1969 to 1996 (mean follow-up time of 15 years, range, 1–246 months), most of them only surgically treated, tumor stage was the most important determinant of survival and the WHO histologic subtype was found to be an independent prognostic factor in Stage I and II, among which WHO Type A, AB, and B1 thymomas formed altogether a low-risk group. Patients with high-risk TET were indicated as possible target for novel adjuvant radiochemotherapy regimens. It should be pointed out that these two categories—low and high risk group thymomas diagnosed on the basis of the 1999 WHO classification (10)—were first mentioned in this paper. By comparison with the historical cohort, the prognosis of patients with B2 and B3 thymoma in the present series (1) has improved, probably partly due to the increased application of adjuvant therapies. However, the prognosis of patients with TCs remained unsatisfactory. The findings suggested that neoadjuvant treatment protocols should be improved. In the same issue of JTD Wei et al. (11) provide their experience in the induction therapy with thymomas and TCs in the framework of the ChART database (DB) (derived from several tertiary centers in China), reporting detailed informations on thymoma downstaging. Further data on the criteria to neoadjuvant therapy adoption and a treatment algorithm have been recently presented (12), and could be discussed among the health care professionals involved in TET care all around the world.
Full table
Full table
In the present cohort (1), the 5-year OS according to Masaoka stage of Thymoma and TC was 59% and 50%, respectively. The 5-year OS of patients with A, AB, B1, B2, B3 thymomas and TCs reported were 100%, 100%, 94%, 80%, 94%, and 45% respectively. As far as progression free survival (PFS) is concerned, the 5-year PFS were 100%, 96%, 78%, 80%, 78% and 39% (for PFS data were available for 217 cases out of 241). OS and PFS were significantly different between thymoma and TC patients. By contrast, no significant differences in OS nor PFS were found among B1, B2 and B3 thymoma patients. Similarly, PFS of A and AB thymoma patients showed no significant differences. The association between disease progression and histological type, as well as between outcome and histological types, were highly significant. Thus a possible future study focused on the same series might concern the relapsed cases and their treatment. As far as the historical cohort (2) is concerned, it should be pointed out that the paper from Chen et al. in 2002 was one of the two papers (13) first evaluating TET with the tool of the 1999 WHO classification addressing the pathological review of all cases, and providing data on its prognostic value. Nowadays the situation is changed, as the WHO classification, although debated, has gained general wide acceptance, through the 2004 and the 2015 editions (4,14). A worldwide collaboration among health care professionals has been established also due to the activity of the International Thymic Malignancy Interest Group (ITMIG), promoting collaboration and workshops on refinements of diagnostic criteria as well as several studies dealing with TET Staging and treatment (15,16).
TET observational studies: comparison with other series
It would be impossible to comment here the whole amount of clinicopathological data on TET series recently provided by several Institutions and clinical researchers from all around the world. Therefore we aimed to comment briefly the findings provided in the present (1) and from the historical cohort series (2) with preliminary data from the ChART database including 18 centers in China, presented in the same issue of JTD and addressed on the Myasthenia Gravis (MG) occurrence in a 1,850 case cohort (6), with the findings deriving from an European series described by Harnath et al., in 2012 (7), with data from the European Society of Thoracic Surgeons (ESTS) (5), and finally with those from the ITMIG retrospective DB reported by Huang et al. (8), concerning the first aggregated data in a worldwide-based case series. Moreover a very complex analysis of the histotype impact of a large Thymoma series has been furtherly reported on the basis of the ITMIG retrospective DB (17), however, TC cases were not included in this series and therefore a direct comparison of data was not possible here.
Thus, referring to an overview of histological profile distribution, in the preliminary data assembly of the ITMIG retrospective DB, six hundred two (602 cases) TCs were reported out of 5,131 TET cases, corresponding to 12% of tumors (8), therefore in line with other reports but slightly fewer than in the paper from Zhu et al. (Table 1). By comparison, in the ESTS series (Table 1) (15), the reported incidence for TC was 9% with comparison to the SCH series (18% for the historical and 24% for the present cohort); in the Harnath series there were 15/93 (16%) TCs. In the ITMIG aggregated data, neuroendocrine tumors were not included (18). Similarly, we didn’t included neuroendocrine neoplasms in our comments to other studies discussed here. Thus, at first glance, a slightly higher incidence of TC cases is suggested from Chinese data with respect to European cases and in the worldwide ITMIG retrospective DB. A male prevalence of TC cases was found by Zhu et al., and the same finding was reported by the ITMIG DB, whereas other series did not showed prevalence of the male gender in TC cases. This observation could foster further studies on the incidence of TC and on the related pathogenetic factors in China. By histological subgroupings, which showed prognostic value (2,13,19,20), no relevant change in the risk group distribution in the cohorts considered was found by comparing the ESTS DB with other cohorts (Table 1). Myasthenia gravis (MG) was less frequent in the SCH series, as already discussed by the Authors, because the SCH doesn’t have a referral Neurology department. However, the presence of MG was associated with improved survival in the present cohort, similarly to the findings reported by Ströbel et al. (19). As already mentioned, not only the SCH series, but also the ChART series shows a high percentage of cases detected in Stage I according to Masaoka (48% in the SCH series, and 40% in the paper from Wang et al.) (Table 2).
Conclusions
Observational studies provide several relevant informations also in the evaluation of rare tumors. Thanks to the recently growing attention to TET, cohort studies were often reported, providing amount of data useful to detect prognostic factors and in promoting progresses in treatment. The centralized pathological review of the Institutional series is an essential prerequisite, although large DB-derived series usually do not receive a pathological review due to its complexity and to the still limited diffusion of telepathological tools. Nevertheless, it appears that in the last fourteen years a considerable progress has been achieved in diagnostic and therapeutical approaches to TET, and high level care standard has been achieved. Among factors influencing this progress there are the technological surgical improvement and the standardization of care. A substantial improvement is certainly due to the increasing spontaneous collaborative efforts in the multidisciplinary team involved in TET care, as evident from the ChART activity. An important input was also given by the worldwide diffusion and promoting capability of ITMIG and of its collaborative projects. However, from the present, although limited, review of retrospective data it appears that probably genetic and/or environmental factors could play a role in contributing to the history of TET patients. Progress in understanding the biology of the disease in different ethnographic frameworks and genetic contexts should be considered prioritary. Molecular data and—among these—the upcoming results of the Cancer Genome Atlas of Thymoma (TCGA-THYM) (https://tcga-data.nci.nih.gov/tcga/) are expected to provide relevant findings on the oncological pathways involved and on somatic changes in neoplastic vs. normal tissues. However, observational studies still constitute the fundament of any cancer research, by providing the “basic datasets” for molecular correlations and therapeutical developments.
Acknowledgements
The author thanks Dr. Simona Baselice for her editorial assistance.
Footnote
Provenance: This is a Guest Editorial commissioned by the Journal of Thoracic Diseases Editor Wentao Fang, MD, Professor (Department of Thoracic Surgery, Shanghai Chest Hospital, Shanghai, China).
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Zhu L, Zhang J, Marx A, et al. Clinicopathological analysis of 241 thymic epithelial tumors-experience in the Shanghai Chest Hospital from 1997-2004. J Thorac Dis 2016;8:718-26. [Crossref] [PubMed]
- Chen G, Marx A, Chen WH, et al. New WHO histologic classification predicts prognosis of thymic epithelial tumors: a clinicopathologic study of 200 thymoma cases from China. Cancer 2002;95:420-9. [Crossref] [PubMed]
- Fang W, Chen W, Chen G, et al. Surgical management of thymic epithelial tumors: a retrospective review of 204 cases. Ann Thorac Surg 2005;80:2002-7. [Crossref] [PubMed]
- Travis WD, Brambilla E, Müller-Hermelink HK, et al. Pathology and Genetics of Tumours of the Lung, Pleura,Thymus and Heart. World Health Organization Classification of Tumours. Lyon: IARCPress 2004.
- Ruffini E, Detterbeck F, Van Raemdonck D, et al. Tumours of the thymus: a cohort study of prognostic factors from the European Society of Thoracic Surgeons database. Eur J Cardiothorac Surg 2014;46:361-8. [Crossref] [PubMed]
- Wang F, Pang L, Fu J, et al. Postoperative survival for patients with thymoma complicating myasthenia gravis-preliminary retrospective results of the ChART database. J Thorac Dis 2016;8:711-7. [Crossref] [PubMed]
- Harnath T, Marx A, Ströbel P, et al. Thymoma-a clinico-pathological long-term study with emphasis on histology and adjuvant radiotherapy dose. J Thorac Oncol 2012;7:1867-71. [Crossref] [PubMed]
- Huang J, Ahmad U, Antonicelli A, et al. Development of the international thymic malignancy interest group international database: an unprecedented resource for the study of a rare group of tumors. J Thorac Oncol 2014;9:1573-8. [Crossref] [PubMed]
- Masaoka A, Monden Y, Nakahara K, et al. Follow-up study of thymomas with special reference to their clinical stages. Cancer 1981;48:2485-92. [Crossref] [PubMed]
- Lucchi M, Basolo F, Ribechini A, et al. Thymomas: clinical-pathological correlations. J Cardiovasc Surg (Torino) 2006;47:89-93. [PubMed]
- Wei Y, Gu Z, Shen Y, et al. Preoperative induction therapy for locally advanced thymic tumors: a retrospective analysis using the ChART database. J Thorac Dis 2016;8:665-72. [Crossref] [PubMed]
- Girard N, Ruffini E, Marx A, et al. Thymic epithelial tumours: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2015;26 Suppl 5:v40-55. [Crossref] [PubMed]
- Okumura M, Ohta M, Tateyama H, et al. The World Health Organization histologic classification system reflects the oncologic behavior of thymoma: a clinical study of 273 patients. Cancer 2002;94:624-32. [Crossref] [PubMed]
- Travis WD, Brambilla E, Burke AP, et al. WHO Classification of Tumours of the Lung, Pleura, Thymus and Heart. 4th edition. Lyon: IARCPress 2015. Available online: http://whobluebooks.iarc.fr/
- Marx A, Ströbel P, Badve SS, et al. ITMIG consensus statement on the use of the WHO histological classification of thymoma and thymic carcinoma: refined definitions, histological criteria, and reporting. J Thorac Oncol 2014;9:596-611. [Crossref] [PubMed]
- Detterbeck F, Korst R. The International Thymic Malignancy Interest Group thymic initiative: a state-of-the-art study of thymic malignancies. Semin Thorac Cardiovasc Surg 2014;26:317-22. [Crossref] [PubMed]
- Weis CA, Yao X, Deng Y, et al. The impact of thymoma histotype on prognosis in a worldwide database. J Thorac Oncol 2015;10:367-72. [Crossref] [PubMed]
- Detterbeck FC, Stratton K, Giroux D, et al. The IASLC/ITMIG Thymic Epithelial Tumors Staging Project: proposal for an evidence-based stage classification system for the forthcoming (8th) edition of the TNM classification of malignant tumors. J Thorac Oncol 2014;9:S65-72. [Crossref] [PubMed]
- Ströbel P, Bauer A, Puppe B, et al. Tumor recurrence and survival in patients treated for thymomas and thymic squamous cell carcinomas: a retrospective analysis. J Clin Oncol 2004;22:1501-9. [Crossref] [PubMed]
- Ströbel P, Hohenberger P, Marx A. Thymoma and thymic carcinoma: molecular pathology and targeted therapy. J Thorac Oncol 2010;5:S286-90. [Crossref] [PubMed]


