Perforation of esophagus and subsequent mediastinitis following mussel shell ingestion
Introduction
Mediastinitis is a very fatal disease entity with high mortality and can occur after esophageal perforation following ingestion of a foreign body that is trapped and penetrates the esophagus. Iatrogenic injury of the esophagus from surgery or endoscopic procedure is the most common cause of perforation and ensuing mediastinitis, and injury from foreign body ingestion is a common cause of this serious medical condition. Esophageal perforation due to a foreign body usually occurs from swallowing sharp objects such as fish or chicken bones (1). Although reports on shell fragments trapped in the esophagus that were successfully removed by esophagoscopy are sporadic, to date, reports on mediastinitis caused by esophageal rupture induced by mussel shell have not been published (2,3). Time elapsed from the injury to initiation of treatment is the most significant factor that affects mortality after esophageal perforation (4,5). In the present case, the patient visited the clinic 4 days after ingestion of a mussel shell fragment, which resulted in the perforation of the esophagus and mediastinitis. Thus, along with a review of the previous literature, we present a case of mediastinitis caused by esophageal perforation from a mussel shell fragment.
Case presentation
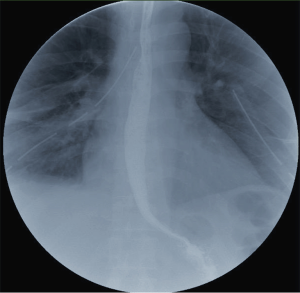
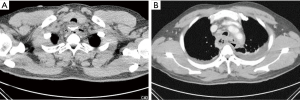
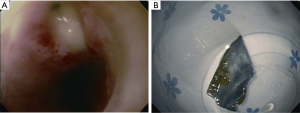
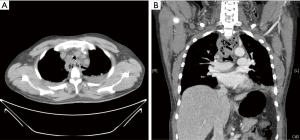
A 46-year-old male (170 cm, 74 kg) visited our emergency department complaining of dysphagia and odynophagia. He ate a spicy seafood noodle soup containing mussel shells 4 days prior. Neck pain developed while he was swallowing the soup which persisted ever since. The lancinating pain was located in the upper back, thorax and neck area. His blood pressure, heart rate and body temperature were 124/74 mmHg, 96 beats/min and 38 °C, respectively. Blood tests showed an elevated white blood cell count (WBC: 28.3×109/L), erythrocyte sedimentation rate (ESR: 55 mm/h) and C-reactive protein (CRP: 30.49 mg/dL). Anteroposterior chest radiography was normal, but cervicothoracic computed tomography (CT) showed a radio-opaque foreign body in proximal esophagus at the level of thoracic inlet and abscess formation in the mediastinum (Figure 1). The airway was compressed and pneumomediastinum was identified. Esophagogastroduodenoscopy revealed interstitial emphysema in the esophagus and mussel shell fragment with esophageal perforation at proximal esophagus 20 cm distant from the incisor. Rigid esophagoscopy was performed under general anesthesia and a rectangular and sharp-edged mussel shell fragment (2 cm × 2.5 cm in size) was removed using a grasping forcep (Figure 2). After changing to the lateral position, right thoracotomy, debridement of mediastinal abscess and irrigation were performed. A drain was placed in the upper mediastinum and a gastric tube was inserted. The patient was extubated and sent to the intensive care unit (ICU). However, he had difficulty breathing with low tidal volume of 200 mL and tachypnea over 30 beats/min. We reintubated the patient with 7.5 Fr single lumen endotracheal tube. Five days later, despite management including continuous parenteral antibiotic therapy and ventilatory care, the patient’s condition did not improve. Blood tests showed an ESR of 42 mm/h, CRP of 22.82 mg/dL and WBC of 14×109/L. Follow-up CT scan showed severe compression of the trachea and severe mediastinitis with abscess (Figure 3). An additional thoracotomy to remove abscess and irrigate was performed. During anesthesia, we used an endobronchial blocker for lung isolation (outer diameter 3.0 mm type A Coopdech bronchial blocker, Daiken Medical Co. Ltd, Osaka, Japan) through the preexisting endotracheal tube of ID 7.5 Fr because of severe edematous larynx, trachea and bronchus. The patient was positioned to left lateral decubitus and the position of the blocker tip was confirmed using a fiber optic bronchoscope (Olympus SC16-3, 2.8 mm, Japan). Mediastinal debridement, the drainage of abscess pocket and the irrigation with 10,000 mL of warm saline were performed. A chest tube was inserted. After the operation, the patient was sent to the ICU with an endotracheal tube. Aerobic staphylococcal bacteria in pleural fluid, streptococcus salivarius bacteria and acinetobacter baumannii were cultured from the abscess. After proper parenteral nutrition and broad spectrum antibiotics, the patient gradually recovered. He was extubated on postoperative day 8. On day 20, subsequent esophagography showed no evidence of extravasation of contrast, obstruction or stricture. The patient was discharged 33 days after the second operation (Figure 4).
Discussion
Many complications may arise from foreign bodies in the esophagus and life-threatening conditions such as retropharyngeal abscess, mediastinitis and vascular injuries may develop (6). Thus, early removal of foreign bodies is mandatory to prevent the progression to mediastinitis. However, in the pediatric population, discovery of a foreign body is frequently delayed, and sometimes leads to esophageal perforation. In adults, sharp objects such as fish or chicken bone may cause injury. Once perforation in the esophagus occurs, the risk of mediastinitis is high (7,8). The common site for perforation usually depends on the cause of injury. Foreign body-induced esophageal perforation usually occurs in the proximal third, and iatrogenic perforation during procedures such as endoscopy occurs mainly in the middle or distal third of the esophagus (5). In our patient, the foreign mussel shell fragment was found 20 cm down from the incisor teeth within mid-esophagus.
The possibility of esophageal perforation may differ based on the type of shell ingested. Upon review of previous articles, esophageal perforation by mussel shell fragment and subsequent mediastinitis is very rare. Mussels have a thinner outer shell compared to other shellfish. Thus, on anteroposterior chest radiography, discovering the fragment may be difficult since the shell may be radiolucent and usually impacted parallel to the coronal section of body (3). Therefore, when particular foreign bodies such as shell fragments are suspected to be trapped in the esophagus, a lateral chest radiography, anteroposterior chest radiography and chest CT scan should be obtained to make the correct diagnosis. In our case, perforation of the esophagus may have occurred shortly after the ingestion of the mussel shell fragment. Thus, when taking the patient history, if a patient is found to have ingested a mussel shell, necessary diagnostic processes and removal are imperative to prevent further consequences. Notably, a sharp object in the esophagus must be removed within 24 hours to minimize the risk of perforation, mediastinitis or abscess (9). Although the gold standard for treating esophageal perforation does not exist, etiology, location, time from perforation and existence of sepsis have been considered the main prognostic factors after surgical treatment (5,10). Primary repair may be a sufficient treatment when esophageal perforation has occurred within 24 hours (4,11). However, after 24 hours, a fistula may form or the risk of complications in neighboring tissues is high. Due to severe mediastinitis in this patient, the surrounding tissue around the esophageal perforation was weak. Therefore, we decided to wait for spontaneous healing after the abscess was removed and irrigated and a drain was placed. However, the patient’s condition did not improve after the first operation. Only after the second operation and aggressive antibiotic therapy based on abscess culture results, the patient’s condition improved. However, we cannot eliminate the possibility of better prognosis using other surgical methods (such as esophagectomy) during the first operation. According to Salo et al. (12), significantly different mortality rates exist between primary repair (67%) and esophagectomy (13%) groups in patients with delayed esophageal perforation and presence of septic condition. Reports on mortality after development of subsequent mediastinitis vary. However, if a surgery was performed within 24 hours of esophageal perforation, the patients showed a significantly higher survival rate than those who had a delayed diagnosis and a surgery 24 hours after the injury (5,13,14). Additionally, survival rate after a surgery for mediastinitis of iatrogenic or traumatic origin showed a better survival rate when the surgery was performed in descending necrotizing mediastinitis. Several published studies reported that overall health status, physiological reserve, extent of associated injuries and number of preoperative comorbidities had a more significant effect on mortality than age or gender (5,14).
Although our patient had a potentially high risk of mortality due to delayed diagnosis after 4 days of ingestion and presence of septic condition that may lead more frequently to complications such as disseminated intravascular coagulation, acute respiratory distress syndrome and multiple organ failure, our patient’s young age, previous good overall health status with large physiological reserve and no history of preexisting disease resulted in satisfactory progress after the surgery without the development of serious complications. In thoracic anesthesia, a single lung ventilation is performed using a double lumen tube (DLT) or bronchial blocker. In the present case, we chose the bronchial blocker rather than DLT for the following reasons: (I) the patient was already intubated with an ID 7.5 single lumen endotracheal tube; (II) we predicted the insertion of the DLT would be very difficult because of edematous and compressed larynx, trachea and bronchus; and (III) the patient was to receive ventilatory care in the ICU during the postoperative period. If postoperative ventilatory support is needed, the DLT is replaced with a single lumen tube immediately after the surgery.
In conclusion, when foreign body impaction is suspected, rapid and accurate diagnostic confirmation is necessary. After diagnosis, prompt removal is mandatory to prevent esophageal perforation and development of subsequent mediastinitis. In particular, if the suspected foreign body is a sharp-edged mussel shell, lateral chest radiography and CT scan must be performed for a correct diagnosis and initiating treatment within 24 hours after the perforation is necessary to prevent mediastinitis and to lower mortality risk.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Sng KK, Koh AJ, Tan NC, et al. An Eastern perspective on oesophageal perforation: a high incidence of ingested bones. ANZ J Surg 2008;78:573-8. [Crossref] [PubMed]
- Kim H, Kim HK, Kang GR, et al. Successful removal of indigested shell using a rigid esophagoscope and a pneumatic lithotriptor. Ann Thorac Surg 2009;88:1019-21. [Crossref] [PubMed]
- Kim S, Kim HH, Jang GH, et al. Mussel shell impaction in the esophagus. Case Rep Gastroenterol 2013;7:112-6. [Crossref] [PubMed]
- Eroglu A, Can Kürkçüogu I, Karaoganogu N, et al. Esophageal perforation: the importance of early diagnosis and primary repair. Dis Esophagus 2004;17:91-4. [Crossref] [PubMed]
- Vallböhmer D, Hölscher AH, Hölscher M, et al. Options in the management of esophageal perforation: analysis over a 12-year period. Dis Esophagus 2010;23:185-90. [Crossref] [PubMed]
- Berry AC, Draganov PV, Patel BB, et al. Embedded pork bone causing esophageal perforation and an esophagus-innominate artery fistula. Case Rep Gastrointest Med 2014;2014:969862.
- Allotey J, Duncan H, Williams H. Mediastinitis and retropharyngeal abscess following delayed diagnosis of glass ingestion. Emerg Med J 2006;23:e12. [Crossref] [PubMed]
- Katsetos MC, Tagbo AC, Lindberg MP, et al. Esophageal perforation and mediastinitis from fish bone ingestion. South Med J 2003;96:516-20. [Crossref] [PubMed]
- Anderson KL, Dean AJ. Foreign bodies in the gastrointestinal tract and anorectal emergencies. Emerg Med Clin North Am 2011;29:369-400. ix. [Crossref] [PubMed]
- Bresadola V, Terrosu G, Favero A, et al. Treatment of perforation in the healthy esophagus: analysis of 12 cases. Langenbecks Arch Surg 2008;393:135-40. [Crossref] [PubMed]
- Eroglu A, Turkyilmaz A, Aydin Y, et al. Current management of esophageal perforation: 20 years experience. Dis Esophagus 2009;22:374-80. [Crossref] [PubMed]
- Salo JA, Isolauri JO, Heikkilä LJ, et al. Management of delayed esophageal perforation with mediastinal sepsis. Esophagectomy or primary repair? J Thorac Cardiovasc Surg 1993;106:1088-91. [PubMed]
- Andrade-Alegre R. Surgical treatment of traumatic esophageal perforations: analysis of 10 cases. Clinics (Sao Paulo) 2005;60:375-80. [Crossref] [PubMed]
- Jabłoński S, Brocki M, Kordiak J, et al. Acute mediastinitis: evaluation of clinical risk factors for death in surgically treated patients. ANZ J Surg 2013;83:657-63. [Crossref] [PubMed]