Tubeless video-assisted thoracoscopic surgery (VATS) under non-intubated, intravenous anesthesia with spontaneous ventilation and no placement of chest tube postoperatively
Introduction
With the development of video-assisted thoracoscopic surgery (VATS) techniques and technology for anesthesia control, non-intubated anesthesia with spontaneous ventilation has been widely applied in VATS. This approach can be applied in most VATS procedures, including lobectomy, segmentectomy, and radical resection of lung cancer. Certain experienced surgeons can even perform highly challenging surgeries (e.g., bronchoplasty) under spontaneous ventilation (1-9). Spontaneous ventilation-based anesthesia techniques have unique advantages relative to intubated anesthesia: (I) only simple intravenous drug use, avoiding the residual effects of muscle relaxants; (II) fewer postoperative complications; and (III) more rapid recovery.
Chest tube placement always causes pain, and its duration is known to be one of the most important factors influencing hospital stay and costs. Early tube removal allows patients to breathe deeply with less pain, which leads to more compliance with chest physiotherapy, as demonstrated by a concomitant improvement in patients’ ventilatory function (10). With the goal of postoperative drainage, Atsushi Watanabe established the following criteria for avoiding chest tube placement: (I) an absence of air leaks during an intraoperative alternative sealing test; (II) an absence of emphysematous changes on inspection; (III) an absence of severe pleural adhesions; and (IV) an absence of prolonged pleural effusion requiring preoperative chest drainage (11). These criteria also provide the basis for the clinical study of tubeless VATS under spontaneous ventilation-based anesthesia. Here, “tubeless VATS” means VATS under non-intubated anesthesia and with no placement of a chest tube postoperatively.
For carefully selected patients, tubeless VATS operations have been carried out at our center. In the present study, we analyzed clinical data in an attempt to evaluate the feasibility and safety of this technique and to assess the role of this technique in promoting rapid recovery as well.
Methods
General data
The anesthesia protocol was reviewed and approved by the Institutional Ethics Committee of the First Affiliated Hospital of Guangzhou Medical University (No. NTEA001). Prior to anesthesia, doctors visited each patient to explain the anesthesia process and method; informed consent was obtained from all enrolled patients, who signed both a “Consent to Anesthesia with Nontracheal Intubation” form and a “Consent to General Anesthesia with Tracheal Intubation” form. Between December 2012 and December 2015, 173 patients were enrolled. Patients were eligible when they had an ASA grade of I–II, BMI <25, normal cardiopulmonary function, and no evidence of the preoperative factors requiring chest drainage mentioned by Atsushi Watanabe (11). The surgical procedures included sympathectomy, bullae resection, and mediastinal tumor resection. In total, 91 patients received tubeless VATS, and 82 patients received intubated general anesthesia-based VATS. All operations were performed by the same group of thoracic surgeons and anesthesiologist team. Patients who underwent tubeless VATS under intravenous anesthesia comprised the intervention group, and patients who received VATS under general anesthesia with a double-lumen tube comprised the control group.
Anesthesia and surgical procedures
The endotracheal intubation for anesthesia was performed in accordance with the routine double-lumen endotracheal intubation procedure. Non-intubated anesthesia was performed by regional anesthesia administration and target sedation, as previously reported (7). If a complication (e.g., bleeding, hypoxemia or hypercapnia) occurred during the surgery and could not be resolved by non-invasive management, a single-lumen tube was inserted under the guidance of a fiber-optic bronchoscope while the patient was in the lateral position, and a blocker was used to achieve lung isolation.
Surgical procedures: the surgical approach for the non-intubated VATS procedures was the same as those for conventional thoracoscopic surgery. The incision in the chest wall could cause collapse of the lung and even iatrogenic pneumothorax.
Drainage management: in the intubated group, when the surgery was finished, a single 28Fr intercostal drain was inserted through the first port site following hemostasis. In the tubeless group, the following sealing test was performed: A silicone chest tube was inserted into the pleural cavity, and the wounds in the chest wall were temporarily closed. The chest tube was then placed under water, and the patient was ventilated at 20 cmH2O of maximum inspiratory pressure. If no air leak was present, the tube was removed, and the incision was closed immediately.
Postoperative management
Routine postoperative monitoring
Each patient’s electrocardiogram (ECG), heart rate (HR), blood pressure (Bp), pulse oxygen saturation (SpO2), respiratory rate (RR), and urine output were constantly monitored in the first 12 h. Postoperative pain was assessed at rest after the patient awoke completely. This involved the patient drawing a pain score from 0 (absent) to 10 cm (most severe imaginable) on a 10-cm line chart. Chest X-ray examination and ultrasonography were performed on all patients 1 h after the operation to exclude internal thoracic hemorrhage and assess the expansion of the lobes, and these examinations were performed again after 12 h.
Lung recruitment maneuver assessment
The lung recruitment maneuver was assessed by chest X-ray at 1 h, 12 h and 1 week (outpatient) postoperation, and the criteria were as follows: good if atelectasis ≥70%, medium if atelectasis ≥50% and <70% and poor if atelectasis <50%.
Postoperative pleural effusion assessment
Pleural effusion was assessed by chest ultrasound at 1 h, 12 h and 1 week (outpatient) postoperation, and the criteria were as follows: mild if liquid anteroposterior diameter <4 cm, medium if liquid anteroposterior diameter ≥4 and <8 cm and severe if diameter ≥8 cm.
Postoperative chest catheterization assessment
Thoracocentesis was performed in the presence of chest drainage catheterization when medium or poor atelectasis or severe pleural effusion was observed. Extubation was performed on all the catheterized patients according to routine criteria.
Indication and methodology for extubation
The indications for extubation of all the extubated patients (including patients in the control group, with intubated anesthesia with single-lung mechanical ventilation, and patients converted from non-intubated anesthesia to tracheal intubation due to extensive pleural adhesion) were as follows: (I) remaining lung complete re-inflation without a residual cavity, as indicated by chest X-ray; (II) no leakage bubble present in the drainage bottle during coughing; (III) non-bloody, non-chylous and non-purulent drainage liquid; and (IV) volume of pleural drainage ≤100 mL in 24 h. The entire drainage tube was extubated at the end of a deep breath, and the drainage entrance was covered with Vaseline gauze to avoid the entry of air.
Data collection and analysis
The following intra- and post-operative clinical data were collected from both groups (intervention and control): intraoperative anesthesia, intraoperative blood loss (mL), postoperative feeding time, the duration of postoperative antibiotic use (antibiotics were stopped when there were no symptoms/signs of pulmonary infection and when the white blood cell count decreased to the normal level), the volume of postoperative pleural drainage, the duration of postoperative chest tube placement, and the duration of the postoperative hospital stay.
Two-sample t-tests were applied to evaluate differences between the treatments. Post-surgical complications were recorded and compared via paired t-tests. Count data were compared using the chi-squared test and Fisher’s exact test within SPSS software version 13.0. P values <0.05 were considered significant.
Results
From December 2012 through December 2015, tubeless VATS was performed on 91 patients. Of these patients, 89 underwent an effective operation and exhibited good postoperative recovery, while 2 had their operation aborted for the following reasons: one patient presented with left pleural adhesions during the sympathetic denervation of the bilateral thoracic segments and was converted to intubated anesthesia, without any postoperative complications. The other patient underwent bullae resection, but due to poor atelectasis, as suggested by the postoperative chest X-ray, chest tube placement was performed, and the tube was retained for 1 d before discharge. Meanwhile, the other surgeries went smoothly in the 82 cases in the intubated group.
Assessment of anesthetic procedure (shown in Table 1)
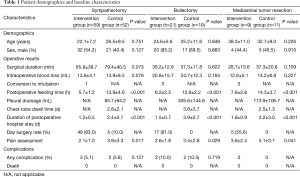
Full table
The surgery went smoothly in the control group with intubated anesthesia with single-lung mechanical ventilation. In the tubeless group, one (10.1%) patient was converted from non-intubated anesthesia to tracheal intubation due to extensive pleural adhesion. Moreover, intraoperative indwelling urinary catheter placement and postoperative retention of the chest tube were performed, and the surgery went smoothly after the approach conversion. In addition, removal of the chest and urinary tubes was performed 1 d postoperation, and the patient was allowed to be discharged 2 d post-operation. All the other 90 patients experienced lung collapse caused by artificial pneumothorax; thus, the exposure of the surgical field was satisfactory, and the surgery went smoothly.
Operative results and postoperative recovery (Table 1)
Sympathectomy: the patients in the tubeless and intubated groups showed significant differences in the postoperative fasting time (5.7±1.2 vs. 13.9±4.6 h), the mean duration of the postoperative hospital stay (1.2±0.5 vs. 2.4±0.7 d) and postoperative pain scores (2.1±1.0 vs. 3.9±3.3) (P<0.05), indicating faster recovery of the patients in the tubeless VATS group. Furthermore, the postoperative pleural drainage volume in the intubated group was 85.7±64.2 mL, while no drainage tube was required in the tubeless group. In addition, no significant difference was found in intraoperative blood loss (13.6±4.1 vs. 14.9±8.5 mL), the operation time (65.8±38.7 vs. 79.4±40.5 min) or postoperative complications (5.1% vs. 3.8%) between the tubeless and the intubated groups.
Bullectomy: the patients in the tubeless and the intubated groups showed significant differences in the postoperative fasting time (6.2±2.5 vs. 12.9±2.2 h), the mean duration of the postoperative hospital stay (1.5±0.7 vs. 3.9±2.7 d) and postoperative pain scores (2.6±1.8 vs. 3.4±2.8) (P<0.05), indicating faster recovery of the patients in the tubeless group. Furthermore, the postoperative pleural drainage volume in the intubated group was 305.6±144.6 mL, while no drainage tube was required in the tubeless group. In addition, no significant difference was found in intraoperative blood loss (20.8±15.7 vs. 24.7±12.3 mL), the operation time (39.2±12.6 vs. 37.3±11.8 min) or postoperative complications (10% vs. 10.5%) between the tubeless and the intubated groups.
Mediastinal tumor resection: the patients in the tubeless and intubated groups showed significant differences in the postoperative fasting time (7.6±2.8 vs. 14.3±3.7 h), the mean duration of the postoperative hospital stay (1.8±0.9 vs. 3.2±3.0 d) and postoperative pain scores (3.6±2.4 vs. 5.1±3.7) (P<0.05), indicating faster recovery of the patients in the tubeless group. Furthermore, the postoperative pleural drainage volume in the intubated group was 113.9±106.7 mL, while no drainage tube was required in the tubeless group. In addition, no significant difference was found in intraoperative blood loss (12.6±5.1 vs. 14.2±6.8 mL), the operation time (28.7±15.6 vs. 37.3±20.8 min) or postoperative complications (0% vs. 0%) between the tubeless and the intubated groups.
Discussion
According to results from a series of clinical studies conducted at our center, intravenous anesthesia with spontaneous ventilation can avoid the residual effects of muscle relaxants, lower the incidence of systemic complications, and thus achieve faster recovery of respiratory muscle function. The advantages of tubeless VATS have been verified by further maturation of the technique, including a shortened operation time and a minimally invasive approach. In the present study, we found that day VATS without intubation preoperation or placement of a chest tube postoperation could be achieved in selected patients.
Tubeless VATS promotes thoracic day surgery
The concept of “day surgery” was first proposed by Dr. Nicol from the Royal Hospital for Children in Glasgow, England, in 1909 (12). Currently, the most common day surgeries include cataract extraction, laparoscopy, laparoscopic repair of inguinal hernias, tonsillectomy and laparoscopic cholecystectomy (13). However, day surgery has not been widely applied in departments of thoracic surgery, and especially not in VATS. According to previous UK experience with approximately 98 cases of thoracic day surgery, VATS was only performed in 31 (31.6%) cases for lung biopsy, while mediastinoscopy and bronchoscopy were performed in the remaining patients. The authors claimed that an ambulatory drainage device was needed for the patient to be discharged; moreover, good patient selection was required (14). Molins et al. reported a prospective study of 300 patients who were treated with thoracic day surgery, including 210 patients treated with mediastinoscopy; 58 patients, with bilateral thoracic sympathectomy; and 32 patients, with lung biopsy (15). Malik et al. reported a study of 16 cases of bullectomy, and 13 of 16 cases were discharged in 1 d with connection to an ambulatory drainage system (16). Therefore, the current types of thoracic day surgery are restricted to bilateral thoracic sympathectomy, mediastinoscopy, bronchoscopy, and simple lung biopsy, and the presence of a chest tube has become a hindrance to thoracic day surgery (17).
Based on 1,500 cases of non-intubated VATS (data not shown), we found that a significantly decreased postoperative pleural drainage volume could be expected in tubeless patients compared to patients with intubated anesthesia via a double-lumen tube. We believe that the reason may be early postoperative feeding, which could have resulted in increased enteral nutrition absorption and metabolism and decreased pleural effusion. Moreover, we found significantly decreased inflammatory cytokine levels in the lung and decreased lung infection in comparison to the results for the bronchoalveolar lavage fluid and serum inflammatory cytokines, which could also have led to a decreased amount of pleural effusion (7). Therefore, we performed the surgery in the current study according to Atsushi Watanabe’s criteria for avoiding chest tube placement during VATS, including a routine test for air leaks, assistance of exhaust by negative pressure, a lack of an indwelling chest tube and close postoperative monitoring; all these modalities can make thoracic day surgery a reality. In the patients with bilateral thoracic sympathectomy, 83% were discharged within 24 h post-operation, whereas 81% of patients with bullectomy were discharged within 1 d post-operation. Even 56% of patients with mediastinal tumor resection satisfied the criteria for day surgery, and none of them was admitted for a second time within a week.
Of the 90 patients in this study, only 1 (1%) patient presented with poor atelectasis after operation, and no other complication was found relative to the surgery with intubation, suggesting that non-intubated VATS is safe and feasible in selected patients.
Anesthesia without tracheal intubation is superior to anesthesia with endotracheal intubation
In comparison to our previous results, we found faster recovery in thoracic surgery patients treated with tubeless VATS under intravenous anesthesia. In the present study, a significantly superior postoperative fasting time and mean duration of the postoperative hospital stay were found in patients in the non-intubated group compared to those in the intubated group, indicating superiority in terms of quick recovery. Furthermore, postoperative pain scores also decreased due to a lack of both intubation and chest tube placement, suggesting that the advantages of this technique include decreasing postoperative discomfort, which promotes postoperative activity and functional exercise, thereby accelerating postoperative recovery. In addition, a significantly decreased hospital stay and medical costs can be achieved by avoiding the use of an indwelling chest tube and performing thoracic day surgery on tubeless patients. At the same time, a decreased mental burden, enhanced patient satisfaction and an improved rate of utilization of existing health resources could also be expected.
Tubeless VATS requires a more advanced operative team
During tubeless VATS, the main challenges for the anesthetist include intraoperative conversion of the anesthesia method, allowing control over more complex conditions, such as hypoxemia and hypercapnia. Moreover, day surgery requires accurate selection of the anesthetic and dosage. For the surgery, the main challenges include correct preoperative assessment; intact and systematic patient selection criteria, which are fundamental to ensuring the operation’s safety; gentle and accurate intraoperative skills, which are also essential for surgery, decreasing the postoperative inflammatory level; and careful postoperative management, which is also necessary due to the lack of placement of a chest tube. Based on 1,500 cases of non-intubated VATS, we successfully established a team for thoracic day surgery. Moreover, a full specification access system and a security system were developed to ensure the safety of the treatment process, including patient selection, preoperative preparation, the operative method, postoperative management, discharge criteria and the follow-up system.
Our experience has shown that tubeless VATS is a safe and feasible surgery with certain advantages in selected patients with thoracic disease and that we can achieve day surgery in these cases. However, determination of how to establish a full specification access system and security system must also be addressed in future investigations.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The anesthesia protocol was reviewed and approved by the Institutional Ethics Committee of the First Affiliated Hospital of Guangzhou Medical University (No. NTEA001). Prior to anesthesia, doctors visited each patient to explain the anesthesia process and method; informed consent was obtained from all enrolled patients, who signed both a “Consent to Anesthesia with Nontracheal Intubation” form and a “Consent to General Anesthesia with Tracheal Intubation” form.
References
- Chen JS, Cheng YJ, Hung MH, et al. Nonintubated thoracoscopic lobectomy for lung cancer. Ann Surg 2011;254:1038-43. [Crossref] [PubMed]
- Pompeo E, Mineo D, Rogliani P, et al. Feasibility and results of awake thoracoscopic resection of solitary pulmonary nodules. Ann Thorac Surg 2004;78:1761-8. [Crossref] [PubMed]
- Tsunezuka Y, Oda M, Matsumoto I, et al. Extended thymectomy in patients with myasthenia gravis with high thoracic epidural anesthesia alone. World J Surg 2004;28:962-5: discussion 965-6.
- Sugimoto S, Date H, Sugimoto R, et al. Thoracoscopic operation with local and epidural anesthesia in the treatment of pneumothorax after lung transplantation. J Thorac Cardiovasc Surg 2005;130:1219-20. [Crossref] [PubMed]
- Pompeo E, Tacconi F, Mineo D, et al. The role of awake video-assisted thoracoscopic surgery in spontaneous pneumothorax. J Thorac Cardiovasc Surg 2007;133:786-90. [Crossref] [PubMed]
- Pompeo E, Tacconi F, Frasca L, et al. Awake thoracoscopic bullaplasty. Eur J Cardiothorac Surg 2011;39:1012-7. [Crossref] [PubMed]
- Liu J, Cui F, Li S, et al. Nonintubated video-assisted thoracoscopic surgery under epidural anesthesia compared with conventional anesthetic option: a randomized control study. Surg Innov 2015;22:123-30. [Crossref] [PubMed]
- Guo Z, Shao W, Yin W, et al. Analysis of feasibility and safety of complete video-assisted thoracoscopic resection of anatomic pulmonary segments under non-intubated anesthesia. J Thorac Dis 2014;6:37-44. [PubMed]
- Shao W, Phan K, Guo X, et al. Non-intubated complete thoracoscopic bronchial sleeve resection for central lung cancer. J Thorac Dis 2014;6:1485-8. [PubMed]
- Refai M, Brunelli A, Salati M, et al. The impact of chest tube removal on pain and pulmonary function after pulmonary resection. Eur J Cardiothorac Surg 2012;41:820-2; discussion 823. [Crossref] [PubMed]
- Watanabe A, Watanabe T, Ohsawa H, et al. Avoiding chest tube placement after video-assisted thoracoscopic wedge resection of the lung. Eur J Cardiothorac Surg 2004;25:872-6. [Crossref] [PubMed]
- Nicoll JM. The surgery of infancy. BMJ 1909.753-6.
- Toftgaard C, Parmentier G. Internationalterminology in ambulatory surgery and its worldwide practice. In: Lemos P, Jarrett P, Philip B. editors. Day Surgery—Development and Practice. London: IAAS, 2006:35-60.
- Ghosh-Dastidar MB, Deshpande RP, Rajagopal K, et al. Day surgery unit thoracic surgery: the first UK experience. Eur J Cardiothorac Surg 2011;39:1047-50. [Crossref] [PubMed]
- Molins L, Fibla JJ, Pérez J, et al. Outpatient thoracic surgical programme in 300 patients: clinical results and economic impact. Eur J Cardiothorac Surg 2006;29:271-5. [Crossref] [PubMed]
- Malik M, Black EA. Fast-track video-assisted bullectomy and pleurectomy for pneumothorax: initial experience and description of technique. Eur J Cardiothorac Surg 2009;36:906-9; discussion 909. [Crossref] [PubMed]
- Molins L, Fibla JJ, Mier JM, et al. Outpatient thoracic surgery. Thorac Surg Clin 2008;18:321-7. [Crossref] [PubMed]


