Preoperative misdiagnosis analysis and accurate distinguish intrathymic cyst from small thymoma on computed tomography
Introduction
The incidence of thymoma is 1.5 cases per million and thymoma is the most common primary neoplasm of the anterior mediastinum, consisted of 47–50% of anterior mediastinal tumors (1-3). Almost half of the early thymoma patients were asymptomatic. With the wide popularity of computed tomography (CT) in clinical and physical examination, mediastinal masses were often incidentally found in asymptomatic patients undergoing CT scans for unrelated reasons. Davis et al. found that 76% of the asymptomatic patients with mediastinal masses had benign lesions (4). In a study conducted in asymptomatic people at high risk for lung cancer who were undergoing CT screening, 71 (0.77%) had a mediastinal mass seen at baseline screening, of which 41 (58%) were thymic. After these mediastinal masses were surgically removed, some pathologically proven cases of thymic cyst were misdiagnosed as thymoma preoperatively due to misinterpretation of CT images (5). Clinical misdiagnosis could lead to high non-therapeutic thymectomy rate, resulting many patients in unnecessary invasive surgery and its associated morbidity. Many published literatures have reported that non-therapeutic thymectomy rates were ranging from 22% to 68% (6,7). CT scans could accurately reveal the characteristics of the masses and was reported to reach a staging accuracy of 87.5%, with the specificity and sensitivity is 90% and 83.3%, respectively (8). Preoperative CT scans could help the surgeons to determine the clinical stage of thymic masses, and consider other potential therapy instead of proceeding directly to thymectomy (9,10). Thus awareness of the imaging characteristics of mediastinal masses is essential to improve the diagnostic accuracy and patient management. Although the CT imaging features of thymoma and intrathymic cysts have been described in prior published studies (11,12), to our knowledge, few investigators have compared and contrasted the CT imaging features of these small lesions with diameter within 3 cm. The purpose of the present study is try to discover the role of preoperative CT scans in distinguish of small thymoma and intrathymic cysts.
Methods
Study population
We retrospectively reviewed the medical records of the patients who had undergone mediastinal neoplasm resection between January 2014 and July 2015 at department of thoracic surgery, Tianjin Chest Hospital. All patients fulfilled the following inclusion criteria were selected: (I) undergone mediastinal masses resection under the thoracoscope; (II) pathologically diagnosed as thymoma or intrathymic cyst; (III) the longest diameter was less than or equal to 3 cm; (IV) CT scans performed within 2 weeks before thymectomy; (V) no other therapy before thymectomy. The study was approved by the Medical Ethics Committee of Tianjin Chest hospital and written informed consent was obtained from the patients.
A total of 316 patients undergone mediastinal masses resection under the thoracoscope during January 2014 and July 2015, 33 of them met the inclusion criteria for the present study, 1 of them had no available CT record and was excluded. Two patients were pathologically diagnosed as thymic hyperplasia. Therefore this study subjects consisted of 30 patients: 17 intrathymic cysts (all cases were unilocular cysts) and 13 thymomas. Twelve (7 intrathymic cysts and 5 thymomas) of them had contrast-enhanced CT scans for further examination before surgery. All 30 patients underwent complete tumor resection. All histopathologic specimens were reviewed and confirmed by two pathologists with more than 5 years of experiences.
Clinical features (clinical data, preoperative CT reports, and pathology reports) were collected by review of the electronic medical record. All thymoma patients were without myasthenia gravis.
CT examination and analysis
The CT examinations were performed using Siemens Somatom Definition dual-source CT (Philips MX 16-slice CT, Cleveland, USA). CT scans was conducted in dual-energy mode, the parameters of tube A were 140 kV, 55 mA, the FOV was 550 mm × 550 mm; and tube B were 80 kV, 210 mA, the FOV was 260 mm × 260 mm. The width of collimator was 64 mm × 1.2 mm, and the screw pitch was 0.5, the rate of tube was 0.33 s/r, and the thickness was 0.75 mm. Before the CT scanning, patients were practiced to hold their breath to avoid motion artifacts. In all patients, the scan range was from the thoracic inlet to 1–3 cm under the diaphragmatic level. Contrast medium (ioversol injection, Hengrui Medicine Co. Ltd, Jiangsu, 320 mg iodine/mL) was injected in double phase injection solution, after injection of 40–50 mL ioversol 40 mL saline was injected using a double-syringe power injector at a rate of 4.5–5.0 mL/s. The trigger threshold method was adopted, and the interest area was set in the aorta, scan was triggered when the CT value was 100 HU after 4 s delay. All imaging data were analyzed at Syngo Dual Energy Software workstation. A round or oval area that was smaller than lesion was selected in four CT layers, and the average CT value of the four areas was reported by software, the mean CT values of the lesion were calculated by averaging the four CT values. CT images were reviewed and interpreted separately by two chest radiologists who were unaware of the pathological classification, final CT results were reached by consensus. For cystic, the CT value is 0 (±20) HU without enhanced, and the CT value of solid mass is >20 HU with enhanced.
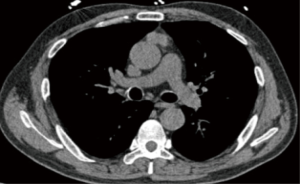
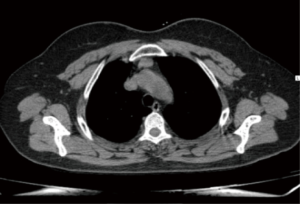
Preoperative CT scans were available for 30 patients (Figures 1,2), and contrast-enhanced CT images were obtained in 12 of 30 patients. The following features were assessed: location, the longest diameter, density, satellitic focus, contour, CT and enhanced CT values. The location of the lesion was categorized as left, right or midline in the anterior mediastinum. The longest diameter of the lesion was measured where the lesion appeared largest on an axial image. Contour was subclassified as “smooth” in the absence of spiculation, ill-defined border, or lobulation, or as “lobulated” if there was one or more lobulations. The pattern of density was assessed by visual inspection and recorded as “homogeneous” if the lesion was the same attenuation and as “heterogeneous” if there were any areas of low or high attenuation within the lesion.
Statistical analysis
Fisher’s exact test was used to compare the difference between the frequency of clinical and CT features in two groups, and quantitative data (operation age, CT values, the longest diameter, ΔCT value) was described as median (quartile), and was compared with Wilcoxon Two-Sample Test. ROC curve of CT values was drawn to explore the best CT threshold to distinguish intrathymic cyst and small thymoma. P value <0.05 was defined as significant. All statistical analysis was performed with SPSS 16.0 software (SPSS Inc., Chicago, IL, USA).
Results
Clinical characteristic of patients
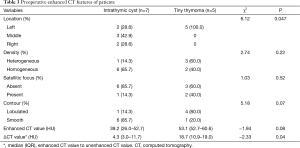
The study group consisted of 30 patients (14 men and 16 women) aged 31 to 72 years (median age, 57 years). All small thymoma patients were without myasthenia gravis. As shown in Table 1, there was no difference in operation age, gender and myasthenia gravis.
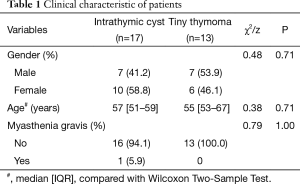
Full table
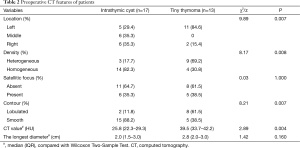
Preoperative CT features
Tiny thymoma was more common in the left than intrathymic cyst (84.62% vs. 29.41%, P=0.007), the density of 14 (82.35%) intrathymic cysts were homogeneous, while only 4 (30.77%) small thymomas were (P=0.008). The contour of intrathymic cyst was more smoothly than small thymoma (88.24% vs. 38.46%, P=0.007). Satellitic focus and the longest diameter had no statistical significance between intrathymic cyst and small thymoma. The CT value of small thymoma 39.5 HU (IQR, 33.7–42.2 HU) was significantly higher than intrathymic cyst [25.8 HU (IQR, 22.3–29.3 HU), P=0.004]. As shown in Table 2.
Full table
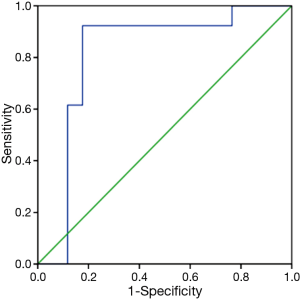
We analyzed the diagnostic accuracy according to CT value of patients using ROC curve analysis. A sensitivity of 0.923 and a false positivity value (1-specificity) of 0.176 comprised the left upper corner of the ROC curve, with the corresponding cut-off value of the CT value at 31.2 HU. The area under the ROC curve (AUC) was 0.814 (P=0.004) (Figure 3).
Contrast-enhanced CT scans
Preoperative contrast-enhanced CT images were obtained in 12 (7 intrathymic cyst and 5 tiny thymoma) patients. All small thymoma distributed in the left, while 2 (28.57%) intrathymic cyst located in left, there was borderline significant difference in location between small thymoma and intrathymic cyst (P=0.047). The ΔCT value of tiny thymoma 18.7 HU (IQR, 10.9–19.0 HU) was higher than intrathymic cyst [4.3 HU (IQR, 3.0–11.7 HU), P=0.04]. Density, Satellitic focus, contour and CT value distributed no statistic difference between the two groups (P>0.05). As shown in Table 3.
Full table
Discussion
In our clinical observation, lesions with diameter <3 cm were often easily misdiagnosed preoperatively, if patients with intrathymic cyst could be diagnosed preoperatively, unnecessary invasive surgery could be avoided, and patients will benefit a lot from it. Thus we focus on masses <3 cm to explore the preoperative misdiagnosis reasons and the accurate method to distinguish the masses. As small thymoma and intrathymic cysts which diameter <3 cm have overlapping clinical and radiological features, they are both asymptomatic in all the cases, it becomes a challenge for clinicians to reach an accuracy preoperative diagnosis. Percutaneous needle biopsy is recommended as a gold standard, however, it is difficult to apply because of those tiny lesions locate posterior to the sternum and anterior to the heart and brachiocephalic vessels (13,14). Therefore, the clinical diagnosis and treatment are often depending on imaging assessment (10). Although many studies have described that preoperative CT scans can accurately reveal the morphologic features of lesions, such as size, location, shape and contours, there still exists potential interpretation variability between observers and even within the same observer. A recent study revealed that incorrect preoperative diagnoses often occurred with cysts under 28 mm in size, even with contrast CT (12). The main reason for misdiagnosis of intrathymic cyst as tiny thymoma was the CT value of intrathymic cyst was much higher than that of general cyst, even close to the density of thymoma, The CT attenuation was >20 HU in most intrathymic cysts cases, leading to the preoperative radiological diagnosis of thymoma (15). In the present study, the mean CT value of intrathymic cyst (25.49 HU) was significantly higher than general cyst, it is well known that some cases of intrathymic cysts have higher CT attenuation than simple fluid due to protein-rich contents, or if haemorrhage or infection occurs as a complication and may be misdiagnosed as solid, mass like thymoma (16-18), thus are surgically resected due to the suspicion of neoplasm or malignancy based on imaging.
In the present study, the median age was 57 years old with a range of 31–72 years old, which is similar to the available studies showed that the median age at diagnosis was 56–59 years (19-21). A recent study reported that indeterminate thymic lesions in younger patients (<43 years) tend more often to be benign (22). In our tiny thymoma group, the age range was 43–72 years old, while the age was 31–65 years old in intrathymic cysts patients. There is no clear age difference between the two groups. Myasthenia gravis is a common autoimmune disorder in thymic disease and was reported in several sporadic case reports of thymic cysts (23,24), while there was only one intrathymic cyst patient with myasthenia gravis in the present study. Thus the details of the association need to be verified in future larger studies.
In terms of preoperative CT features of patients, small thymoma was more common in the left than intrathymic cyst, and in small thymoma patients, no lesions located in the middle, which was somewhat comparable to some available studies which found that <25% of thymic epithelial tumors were in the midline (25,26). In our study, the density was more homogenous and the contour was more smoothly in intrathymic cyst than small thymoma, which is consist with the conclusions in study of Ackman et al. (27). It was reported that if a tumor is lobulated and has heterogeneous density, it is often a highly invasive thymoma or thymic carcinoma (3). And high risk thymomas demonstrated more irregular shape and contour than low-risk thymomas in WHO classification (28).
In a study conducted in 66 patients who had undergone thymectomy for benign thymic lesions or early stage malignant thymic neoplasms, the axes of malignant tumors were larger than benign lesions (22). Since thymic carcinomas exhibit more aggressive behavior and a poorer outcome compared with benign lesions, they have been shown to be significantly larger (25). However, due to the small number of the study, we found that the longest diameter of small thymoma was only slightly longer than intrathymic cyst, thus the details and significance of size in small thymoma and intrathymic cysts remain to be investigated in larger cohorts.
The median CT value of thymic cyst was reported to be 24.8 HU with range of −19.9–58.2 HU in a recent 6-year consecutive thymectomy cohort (27), and Araki et al. found that in intrathymic cysts cases, the mean CT attenuation was 38 HU (range, 6–62 HU) on contrast-enhanced CT, and was 45 HU (range, 26–64 HU) on unenhanced CT (P=0.41) (15). In the present study, for intrathymic cyst, the median CT value of CT and contrast-enhanced CT was 25.8 HU (range, 9.9–47.3 HU) and 39.2 HU (range, 8.3–59.0 HU) respectively, which was less than those reports, maybe the diameter of our patients was less than 3 cm could account for this difference. We then analyzed the preoperative diagnostic accuracy according to CT value using ROC curve to select the best cut-off point. Because the AUC of 0.814 was indicative of moderate accuracy for this standard, CT value was determined to be a significant factor affecting the preoperative diagnostic accuracy. The cut-off point for CT value deduced using ROC curve analysis was 31.2 HU (sensitivity =92.3%, specificity =82.3%). Therefore, CT value less than 31.2 HU were more often diagnosed as intrathymic cyst in thymic lesions with the longest diameter less than 3 cm.
Our study had several limitations. First, our study was a retrospective study, which was susceptible to potential selection bias. Since almost all the cases without surgery chose observation and the pathology results were unavailable, thus only resected cases were included. Autoimmune diseases such as myasthenia gravis seemed very few in our cases, because myasthenia gravis was only found in masses with diameter larger than 3 cm and was excluded in our study. Second, the relatively small number of patients from a single institution, and enhanced CT are performed in a limited number of patients might have limited the significance of CT features. Further studies with larger study populations and multicenter design would certainly be valuable to confirm our results. However, thymic lesions with diameter less than 3 cm are rare, and this is the first study to compare the preoperative CT image features of tiny thymoma and intrathymic cyst, and try to clarify the main reasons and suggestions for preoperative misdiagnosis of tiny thymoma and intrathymic cyst.
Conclusions
In conclusion, the clinical and preoperative CT characteristics of small thymoma and intrathymic cyst with diameter less than 3 cm were described. Left location, heterogeneous density, higher CT value and lobulated contour were more frequently found in tiny thymoma, and we recommended that when CT value was 31.2 HU, it could act as a threshold for distinguish tiny thymoma and intrathymic cyst for clinicians.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Medical Ethics Committee of Tianjin Chest Hospital and written informed consent was obtained from the patients.
References
- Marom EM, Milito MA, Moran CA, et al. Computed tomography findings predicting invasiveness of thymoma. J Thorac Oncol 2011;6:1274-81. [Crossref] [PubMed]
- Ruffini E, Filosso PL, Mossetti C, et al. Thymoma: inter-relationships among World Health Organization histology, Masaoka staging and myasthenia gravis and their independent prognostic significance: a single-centre experience. Eur J Cardiothorac Surg 2011;40:146-53. [Crossref] [PubMed]
- Liu GB, Qu YJ, Liao MY, et al. Relationship between computed tomography manifestations of thymic epithelial tumors and the WHO pathological classification. Asian Pac J Cancer Prev 2012;13:5581-5. [Crossref] [PubMed]
- Davis RD Jr, Oldham HN Jr, Sabiston DC Jr. Primary cysts and neoplasms of the mediastinum: recent changes in clinical presentation, methods of diagnosis, management, and results. Ann Thorac Surg 1987;44:229-37. [Crossref] [PubMed]
- Henschke CI, Lee IJ, Wu N, et al. CT screening for lung cancer: prevalence and incidence of mediastinal masses. Radiology 2006;239:586-90. [Crossref] [PubMed]
- Jurado J, Javidfar J, Newmark A, et al. Minimally invasive thymectomy and open thymectomy: outcome analysis of 263 patients. Ann Thorac Surg 2012;94:974-81; discussion 981-2. [Crossref] [PubMed]
- Kent MS, Wang T, Gangadharan SP, et al. What is the prevalence of a "nontherapeutic" thymectomy? Ann Thorac Surg 2014;97:276-82; discussion 82. [Crossref] [PubMed]
- Tian J, Chen W, Du S, et al. Ct manifestations and staging of invasive thymomas: A comparison with pathology. Journal of Clinical Radiololgy 2003;22:195-8.
- Nakagawa K, Asamura H, Matsuno Y, et al. Thymoma: a clinicopathologic study based on the new World Health Organization classification. J Thorac Cardiovasc Surg 2003;126:1134-40. [Crossref] [PubMed]
- Yanagawa M, Tomiyama N. Prediction of thymoma histology and stage by radiographic criteria. Thorac Surg Clin 2011;21:1-12. v. [Crossref] [PubMed]
- Tomiyama N, Honda O, Tsubamoto M, et al. Anterior mediastinal tumors: diagnostic accuracy of CT and MRI. Eur J Radiol 2009;69:280-8. [Crossref] [PubMed]
- Gochi F, Omasa M, Yamada T, et al. Factors affecting the preoperative diagnosis of anterior mediastinal cysts. Gen Thorac Cardiovasc Surg 2015;63:349-53. [Crossref] [PubMed]
- Mehran R, Ghosh R, Maziak D, et al. Surgical treatment of thymoma. Can J Surg 2002;45:25-30. [PubMed]
- Murakawa T, Nakajima J, Kohno T, et al. Results from surgical treatment for thymoma. 43 years of experience. Jpn J Thorac Cardiovasc Surg 2000;48:89-95. [Crossref] [PubMed]
- Araki T, Sholl LM, Gerbaudo VH, et al. Intrathymic cyst: clinical and radiological features in surgically resected cases. Clin Radiol 2014;69:732-8. [Crossref] [PubMed]
- Nishino M, Ashiku SK, Kocher ON, et al. The thymus: a comprehensive review. Radiographics 2006;26:335-48. [Crossref] [PubMed]
- Jeung MY, Gasser B, Gangi A, et al. Imaging of cystic masses of the mediastinum. Radiographics 2002;22:S79-93. [Crossref] [PubMed]
- Avila NA, Mueller BU, Carrasquillo JA, et al. Multilocular thymic cysts: imaging features in children with human immunodeficiency virus infection. Radiology 1996;201:130-4. [Crossref] [PubMed]
- Strollo DC, Rosado-de-Christenson ML. Tumors of the thymus. J Thorac Imaging 1999;14:152-71. [Crossref] [PubMed]
- de Jong WK, Blaauwgeers JL, Schaapveld M, et al. Thymic epithelial tumours: a population-based study of the incidence, diagnostic procedures and therapy. Eur J Cancer 2008;44:123-30. [Crossref] [PubMed]
- Engels EA, Pfeiffer RM. Malignant thymoma in the United States: demographic patterns in incidence and associations with subsequent malignancies. Int J Cancer 2003;105:546-51. [Crossref] [PubMed]
- McErlean A, Huang J, Zabor EC, et al. Distinguishing benign thymic lesions from early-stage thymic malignancies on computed tomography. J Thorac Oncol 2013;8:967-73. [Crossref] [PubMed]
- Okumura S, Ohta T, Fujioka M, et al. A case of multilocular thymic cyst with myasthenia gravis. Nihon Kyobu Geka Gakkai Zasshi 1995;43:917-21. [PubMed]
- Yamamura H, Mase T, Shioi K, et al. A case of thymic cyst and thymoma with myasthenia gravis. Kyobu Geka 1997;50:975-7. [PubMed]
- Jung KJ, Lee KS, Han J, et al. Malignant thymic epithelial tumors: CT-pathologic correlation. AJR Am J Roentgenol 2001;176:433-9. [Crossref] [PubMed]
- Jeong YJ, Lee KS, Kim J, et al. Does CT of thymic epithelial tumors enable us to differentiate histologic subtypes and predict prognosis? AJR Am J Roentgenol 2004;183:283-9. [Crossref] [PubMed]
- Ackman JB, Verzosa S, Kovach AE, et al. High rate of unnecessary thymectomy and its cause. Can computed tomography distinguish thymoma, lymphoma, thymic hyperplasia, and thymic cysts? Eur J Radiol 2015;84:524-33. [Crossref] [PubMed]
- Ozawa Y, Hara M, Shimohira M, et al. Associations between computed tomography features of thymomas and their pathological classification. Acta Radiol 2015. [Epub ahead of print]. [Crossref] [PubMed]