Early or delayed initiation of renal replacement therapy for critically ill patients—do we know the right time?
Acute kidney injury (AKI) is a common clinical condition among critically ill patients, especially complicated with sepsis or cardiothoracic surgery. Its incidence has been globally reported to reach 30–50% in intensive care units (ICUs) (1,2). Several internationally standardized diagnostic criteria of AKI have been suggested (3,4) and the latest AKI classification criteria was published by Kidney Disease Improving Global Outcomes (KDIGO) in 2012 with the stratification of AKI patients by serum creatinine level and urine output (5). Although ideal management of AKI patients in ICU settings has vigorously been investigated with these AKI diagnostic criteria developments, we have not acquired any pharmacological agents that are effective for AKI in the clinical. On the other hand, renal replacement therapy (RRT) has been employed as a key clinical intervention for severe AKI patients with life-threatening critical illness. However, we have not obtained any clear evidence regarding the optimal timing of RRT initiation for severe AKI.
There has already existed a consensus to introduce RRT for patients with diuretics-resistant severe fluid overload causing pulmonary edema, severe disturbance of electrolytes (hyperkalemia) or acid-base equilibrium (metabolic acidosis). Decision to start RRT for the severe AKI patients without those conditions are, however, likely to be subjective because of a lack of robust evidence. Optimal timing of RRT initiation for severe AKI has recently been investigated by two randomized controlled trials.
Gaudry and colleagues conducted an unblinded, prospective, multicenter, randomized trial in 31 French ICUs, which was named Artificial Kidney Initiation in Kidney Injury (AKIKI) study (6). In this study, 620 stage 3 AKI patients diagnosed by the latest KDIGO criteria who required invasive mechanical ventilation and/or vasoactive agents underwent a randomization into two groups; the early- or the delayed-strategy groups. Patients with an immediate RRT indication, at least one of the following conditions from the beginning were excluded: blood urea nitrogen >112 mg/mL, serum potassium level >6 mmol/L (or >5.5 mmol/L despite medical treatment), pH <7.15, and acute pulmonary edema due to fluid overload. RRT was initiated immediately after randomization for 312 patients in the early-strategy group, while RRT was suspended for 308 patients in the delayed-strategy group until immediate RRT indication described above observed, or oliguria continued for more than 72 h after the randomization. The primary outcome was overall survival at day 60.
There was no significant difference between the early- and delayed-strategy groups in the 60-day mortality (48.5% vs. 49.7%, P=0.79). Although all the patients in the early-strategy group received RRT within a median of 2 h after the randomization, only 51% of the patients in the delayed-strategy group were treated with RRT in the study period and its initiation was a median of 57 h after the randomization. No difference was observed in mechanical ventilation or vasopressors free days, ICU or hospital stay, and the rate of RRT dependency on day 20 and day 60. The incidence of hypophosphatemia and catheter-related blood stream infection (CRBSI), both of which were known as potent complications of RRT, was significantly higher in the early-strategy group than in the delayed-strategy group (hypophosphatemia: 22% vs. 15%, P=0.03; CRBSI: 10% vs. 5%, P=0.03). The diuresis occurred earlier after the randomization in the delayed-strategy group (P<0.001).
This study was the largest randomized control trial so far regarding the appropriate timing of RRT initiation for AKI. Although several previous randomized trials have been conducted to clarify the same issue of RRT initiation, crucial limitations such as sample size, lack of appropriate control group without RRT were pointed out. A recent systematic review suggested no advantage of early initiation strategy of RRT for AKI patients (7). This study included thirty-six studies (seven randomized controlled trials, ten prospective cohorts, and nineteen retrospective cohorts) and failed to show any beneficial effect of early RRT initiation on patient survival and shorter ICU or hospital length of stay. In addition, Jun et al. conducted a post hoc analysis of Randomized Evaluation of Normal versus Augmented Level (RENAL) study, which was one of the two well-known randomized control trials to investigate optimal dosage of RRT. This post hoc analysis concluded that the time from AKI diagnosis to RRT initiation was not a significant predicting factor for the outcomes such as mortality (8).
It is of note that some investigators argued the positive effect of early RRT initiation on prognosis of ICU patients (9,10). A recent single-center randomized control trial, named as Early vs. Late Initiation of Renal Replacement Therapy in Critically Ill Patients With Acute Kidney Injury (ELAIN) trial, was published in the Journal of the American Medical Association (11), just 10 days after the report of AKIKI study was published in the New England Journal of Medicine. The ELAIN study enrolled 231 AKI patients and demonstrated significantly reduced 90-day mortality, recovered renal function, shorter duration of RRT, and length of hospital stay in the early RRT initiation group. Different inclusion criteria between the AKIKI and the ELAIN trials, including the process of RRT initiation, primary outcome and underlying local factors might cause the discordancy of the conclusions from these two RCTs. The differences were summarized in Table 1.
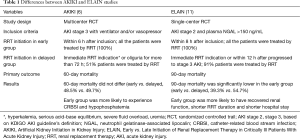
Full table
The AKIKI study contains several critical points to be carefully validated. First, they showed almost half of the population in the delayed-strategy group eventually did not need RRT. Those who avoided RRT in the delayed-strategy group presented significantly lower mortality rate (37.1%) than the early-strategy group (48.5%) and the group of those who finally required RRT in the delayed-strategy group (61.8%). This result inevitably would suggest a potentially harmful effect of delayed strategy of RRT, though the authors attributed this result to the differences of baseline characteristics among each group. Second, the low rate of continuous RRT (only 30%) was reported in the setting that inclusion criteria required invasive mechanical ventilation and/or vasoactive agents. The enrolled patients might not be critically ill especially regarding of circulation problem. Finally, the diuresis reported as a marker of improved kidney function should be carefully interpreted because of the significantly higher rate of diuretic use in the delayed-strategy group comparted with early strategy group (36.5% vs. 1.3%).
It should be addressed that RRT, or any type of therapeutics, is not completely free from adverse effects. Administration of anti-coagulants, vascular access insertion, and high cost of medical professionals and equipment are necessary for RRT. However, “wait and see” attitude toward severe AKI patients was not persuaded by the AKIKI study. Although higher risk and cost were inevitable for earlier RRT initiation, clinicians at bedside were forced to concentrate on detecting the worsening clinical signs that would require immediate intervention of RRT in the delayed-strategy group, as described in the Supplementary Material section of the AKIKI study article. Indeed, the delayed-strategy group in the AKIKI study was more likely to receive medical treatment against volume overload, hyperkalemia, and acidosis compared with the early-strategy group. Although rapid and proper treatments for these abnormalities should be conducted perfectly, the patients in the delayed-strategy group were exposed to the risk of adverse events.
Nevertheless, the results obtained by this well-designed study should be appreciated because we did not have any strong evidence regarding RRT initiation in the field of critical care nephrology. It should be noted that some severe AKI patients might be able to avoid RRT in particular settings because approximately 50% patients in the delayed-strategy group did not need any RRT.
Do we know the right time for starting RRT in AKI? Probably not yet. Two other large RCTs to validate the appropriate timing of RRT initiation are currently ongoing; the STARRT-AKI study in Canada (12) and IDEAL-ICU study in France (13). So far, severity of AKI has been determined by using serum creatinine concentration. However, the validity of short-term changes in serum creatinine level is questioned recently, since it was not directly associated with long-term mortality and prognosis in post hoc analysis of several large AKI trials (14). Additionally, emerging AKI biomarkers such as neutrophil gelatinase-associated lipocalin (NGAL) may help us to identify renal AKI and exclude so-called prerenal AKI, which can be recovered by fluid resuscitation and pressor administration (15). Finally, although evidence established by a number of RCTs can suggest the most appropriate treatment for some specific clinical settings, we still have to investigate when would be the best timing of RRT initiation for every single AKI patient.
Acknowledgements
None.
Footnote
Provenance: This is an invited Commentary commissioned by the Section Editor Zhongheng Zhang (Department of Critical Care Medicine, Jinhua Municipal Central Hospital, Jinhua Hospital of Zhejiang University, Jinhua, China).
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Bagshaw SM, George C, Bellomo R, et al. A comparison of the RIFLE and AKIN criteria for acute kidney injury in critically ill patients. Nephrol Dial Transplant 2008;23:1569-74. [Crossref] [PubMed]
- Nisula S, Kaukonen KM, Vaara ST, et al. Incidence, risk factors and 90-day mortality of patients with acute kidney injury in Finnish intensive care units: the FINNAKI study. Intensive Care Med 2013;39:420-8. [Crossref] [PubMed]
- Bellomo R, Ronco C, Kellum JA, et al. Acute renal failure - definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care 2004;8:R204-12. [Crossref] [PubMed]
- Mehta RL, Kellum JA, Shah SV, et al. Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care 2007;11:R31. [Crossref] [PubMed]
- KDIGO Clinical Practice Guideline for Acute Kidney Injury: Notice. Kidney Int Suppl (2011) 2012;2:1.
- Gaudry S, Hajage D, Schortgen F, et al. Initiation strategies for renal-replacement therapy in the intensive care unit. N Engl J Med 2016;375:122-33. [Crossref] [PubMed]
- Wierstra BT, Kadri S, Alomar S, et al. The impact of "early" versus "late" initiation of renal replacement therapy in critical care patients with acute kidney injury: a systematic review and evidence synthesis. Crit Care 2016;20:122. [Crossref] [PubMed]
- Jun M, Bellomo R, Cass A, et al. Timing of renal replacement therapy and patient outcomes in the randomized evaluation of normal versus augmented level of replacement therapy study. Crit Care Med 2014;42:1756-65. [Crossref] [PubMed]
- Karvellas CJ, Farhat MR, Sajjad I, et al. A comparison of early versus late initiation of renal replacement therapy in critically ill patients with acute kidney injury: a systematic review and meta-analysis. Crit Care 2011;15:R72. [Crossref] [PubMed]
- Liu Y, Davari-Farid S, Arora P, et al. Early versus late initiation of renal replacement therapy in critically ill patients with acute kidney injury after cardiac surgery: a systematic review and meta-analysis. J Cardiothorac Vasc Anesth 2014;28:557-63. [Crossref] [PubMed]
- Zarbock A, Kellum JA, Schmidt C, et al. Effect of early vs delayed initiation of renal replacement therapy on mortality in critically ill patients with acute kidney injury: the ELAIN randomized clinical trial. JAMA 2016;315:2190-9. [Crossref] [PubMed]
- Smith OM, Wald R, Adhikari NK, et al. Standard versus accelerated initiation of renal replacement therapy in acute kidney injury (STARRT-AKI): study protocol for a randomized controlled trial. Trials 2013;14:320. [Crossref] [PubMed]
- Barbar SD, Binquet C, Monchi M, et al. Impact on mortality of the timing of renal replacement therapy in patients with severe acute kidney injury in septic shock: the IDEAL-ICU study (initiation of dialysis early versus delayed in the intensive care unit): study protocol for a randomized controlled trial. Trials 2014;15:270. [Crossref] [PubMed]
- Coca SG, Zabetian A, Ferket BS, et al. Evaluation of short-term changes in serum creatinine level as a meaningful end point in randomized clinical trials. J Am Soc Nephrol 2016;27:2529-42. [Crossref] [PubMed]
- Doi K, Katagiri D, Negishi K, et al. Mild elevation of urinary biomarkers in prerenal acute kidney injury. Kidney Int 2012;82:1114-20. [Crossref] [PubMed]


