Translation from the data of clinical trials to precision medicine: limitation of the current risk score for predicting coronary thrombosis and major bleeding
In his 2015 State of the Union address, President Obama announced that he’s launching the Precision Medicine Initiative—a bold new research effort to revolutionize how we improve health and treat disease (1). Until now, most medical treatments have been designed with a “one-size-fits-all” approach, which can be very successful for some patients but not for others. On the other hand, “precision medicine” is an innovative approach that calls for individual differences depending on people’s genes, biomarkers, environments, and lifestyles. However, in many clinical situations, the outcomes following interventions are associated with multiple clinical or laboratory variables. By replacing, risk prediction models or scoring systems can evaluate the clinical impacts of a therapeutic intervention and consequently help making medical decision (2).
The results of multiple randomized clinical trials have increased the debates regarding the usage of dual antiplatelet therapy (DAPT) after percutaneous coronary intervention (PCI) (3). Understandably, balancing the risk of coronary thrombosis and major bleeding after PCI may be related with optimization of the regimen, potency, and duration of DAPT. However, multiple factors with different pathophysiology must be related with the occurrence of coronary thrombosis and major bleeding after PCI. Over 150 years ago, Rudolf Virchow first suggested a triad of conditions predisposing to thrombus formation—bleeding may be the opposite side in the same triad of conditions. A contemporary concept of Virchow’s triad expands and includes multiple components (4): (I) abnormal vessel wall: endothelial dysfunction, inflammation and atherosclerosis; (II) abnormal blood flow: abnormality in hemorheology and turbulence at bifurcated or stenotic lesions; and (III) abnormal blood constituents: inflammation, abnormalities in platelet function, coagulation, fibrinolysis, and metabolic or hormonal factors.
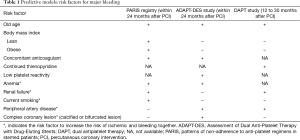
Recently, a number of risk scores to predict the risk of coronary thrombosis and major bleeding in patients receiving DAPT after PCI have been developed and validated; the three major ones were patterns of non-adherence to anti-platelet regimens in stented patients (PARIS) registry (5), Assessment of Dual Anti-Platelet Therapy with Drug-Eluting Stents (ADAPT-DES) registry (6), and DAPT study (7) (Table 1). From the PARIS registry (5), Baber et al. reported on various clinical and procedural risk factors associated with coronary thrombosis and major bleeding during DAPT in PCI-treated patients. Calculated risk estimates were converted into risk scores, categorizing into low, intermediate, and high risk for thrombotic and bleeding events. These scores were validated with the data of the ADAPT-DES registry, which performance showed the moderate power.
Full table
When compared the risk models for major bleeding between the studies, there are some points of similarity but many differences also exist. These models can be used to decide individual duration of DAPT beyond 1 year, based on the absolute benefit-risk ratio. Interestingly, old age was associated with the increased risk of major bleeding from all predictive models together, which finding may support the recommendation that prolonged DAPT following PCI doesn’t obtain any clinical benefit in old patients.
Scores never reflect the entire truth and have multiple limitations in these models. First, many risk factors were overlapped for both ischemic and bleeding property (e.g., renal failure, peripheral artery disease). If we take the physiological character of these risk factors into account, it may be too difficult to find the plausible explanation. In the DAPT analysis (7), these risk factors (i.e., peripheral artery disease, hypertension and renal failure) were excluded from the model of risk score. Second, complexity of coronary anatomy and procedure all are important contributors to the ischemic risks, which were not included in their analysis (5,6). Third, several clinically important biochemical or laboratory factors were not measured or included in their model performance. For example, the levels of high-sensitivity C-reactive protein and cholesterol have been associated with the risk of ischemic events occurrence following PCI (8), which were not included in building the predictive model. Echocardiographic measurement for left ventricular ejection fraction is a like instance. Fourth, the association between biochemical biomarkers and major bleeding can be different over time (9,10), but this factor was not presumed in their analysis. For example, physiological relevance of platelet reactivity for major bleeding appeared higher with earlier as opposed to later events over time (9,10). Finally, most data from these clinical trials were derived from Western population. East Asians have shown lower thrombophilia and higher risk of bleeding compared with Western population during antiplatelet therapy (11), which may influence the required duration and potency of DAPT following PCI. Contrary to the DAPT study (12), among Korean patients who were on 12-month DAPT without complications, an additional 24-month DAPT versus aspirin alone did not reduce the risk of the ischemic events (13).
Whether an approach with a score calculation is more accurate than approaches based on a simple algorithm, expert recommendations, or just physician’s discretion remains still unknown. Aforementioned, the current predictive models for the risk of coronary thrombosis and major bleeding have many limitations. To overcome these limits, measuring several important biochemical or laboratory surrogates are needed to raise the predictive power and cover the trustworthy pathophysiology of clinical events. In addition, some validated surrogates can be used as modifiable factors; a major benefit of these revised scoring systems may be the identification of potentially modifiable factors that can be remedied as a means of reducing thrombotic or bleeding risk among patients receiving DAPT.
Acknowledgements
Funding: This editorial was supported by research grants from the Basic Science Research Program through the National Research Foundation (NRF) of Korea funded by the Ministry of Science, ICT and Future Planning (NRF-2015R1A5A2008833).
Footnote
Provenance: This is an invited Editorial commissioned by the Section Editor Feng Zhang (Department of Cardiology, Zhongshan Hospital of Fudan University, Shanghai, China).
Conflicts of Interest: Dr. Jeong has received honoraria for lectures from AstraZeneca, Sanofi-Aventis, Daiichi Sankyo/Lilly, Haemonetics, Otsuka and Yuhan Pharmaceuticals; and research grants or support from AstraZeneca, Korean Society of Interventional Cardiology, Han-mi Pharmaceuticals, and Haemonetics. The other authors have no conflicts of interest to declare.
References
- The White House. The Precision Medicine Initiative. Available online: https://www.whitehouse.gov/precision-medicine, accessed June 24, 2016.
- Pencina MJ, Peterson ED. Moving From Clinical Trials to Precision Medicine: The Role for Predictive Modeling. JAMA 2016;315:1713-4. [Crossref] [PubMed]
- Montalescot G, Brieger D, Dalby AJ, et al. Duration of Dual Antiplatelet Therapy After Coronary Stenting: A Review of the Evidence. J Am Coll Cardiol 2015;66:832-47. [Crossref] [PubMed]
- Lippi G, Franchini M, Targher G. Arterial thrombus formation in cardiovascular disease. Nat Rev Cardiol 2011;8:502-12. [Crossref] [PubMed]
- Baber U, Mehran R, Giustino G, et al. Coronary Thrombosis and Major Bleeding After PCI With Drug-Eluting Stents: Risk Scores From PARIS. J Am Coll Cardiol 2016;67:2224-34. [Crossref] [PubMed]
- Gaber U, Mehran R, Giustino G, et al. Coronary Thrombosis and Major Bleeding After PCI With Druarge Bleeding After Percutaneous Coronary Intervention. J Am Coll Cardiol 2015;66:1036-45. [PubMed]
- Yeh RW, Secemsky EA, Kereiakes DJ, et al. Development and Validation of a Prediction Rule for Benefit and Harm of Dual Antiplatelet Therapy Beyond 1 Year After Percutaneous Coronary Intervention. JAMA 2016;315:1735-49. [Crossref] [PubMed]
- Park DW, Lee SW, Yun SC, et al. A point-of-care platelet function assay and C-reactive protein for prediction of major cardiovascular events after drug-eluting stent implantation. J Am Coll Cardiol 2011;58:2630-9. [Crossref] [PubMed]
- Mangiacapra F, Patti G, Barbato E, et al. A therapeutic window for platelet reactivity for patients undergoing elective percutaneous coronary intervention: results of the ARMYDA-PROVE (Antiplatelet therapy for Reduction of MYocardial Damage during Angioplasty-Platelet Reactivity for Outcome Validation Effort) study. JACC Cardiovasc Interv 2012;5:281-9. [Crossref] [PubMed]
- Stone GW, Witzenbichler B, Weisz G, et al. Platelet reactivity and clinical outcomes after coronary artery implantation of drug-eluting stents (ADAPT-DES): a prospective multicentre registry study. Lancet 2013;382:614-23. [Crossref] [PubMed]
- Levine GN, Jeong YH, Goto S, et al. Expert consensus document: World Heart Federation expert consensus statement on antiplatelet therapy in East Asian patients with ACS or undergoing PCI. Nat Rev Cardiol 2014;11:597-606. [Crossref] [PubMed]
- Mauri L, Kereiakes DJ, Yeh RW, et al. Twelve or 30 months of dual antiplatelet therapy after drug-eluting stents. N Engl J Med 2014;371:2155-66. [Crossref] [PubMed]
- Lee CW, Ahn JM, Park DW, et al. Optimal duration of dual antiplatelet therapy after drug-eluting stent implantation: a randomized, controlled trial. Circulation 2014;129:304-12. [Crossref] [PubMed]


