Hybrid video-assisted thoracoscopic surgery lobectomy and en-bloc chest wall resection for non-small cell lung cancer
Case presentation
An active 75 years old male smoker presented with a 6-week history of haemoptysis and persistent right sided chest pain; bilateral finger clubbing being the only positive finding on examination.
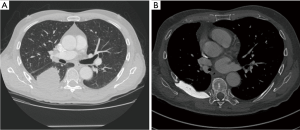
Computed tomography (CT) (Figure 1) and positron emission tomography-computed tomography (PET-CT) scans demonstrated a 6 cm × 5 cm mass in the apical segment of his right lower lobe abutting the pleural surface, with biopsy revealing a well-differentiated squamous cell carcinoma cT3N0M0.
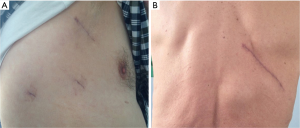
A videothoracoscopic approach (Figure 2) was chosen in view of the posterolateral location of the tumour in proximity to the incision line of the conventional thoracotomy incision. Initial uniportal exploratory VATS demonstrated tumour arising from the right lower lobe, abutting the posterior segment of the upper lobe and invading the chest wall in the lower hemithorax.
A right lower lobectomy with systematic lymph node dissection was performed via conventional anterior three-port VATS. The exact extension of chest wall involvement assessed under videoscope-guidance, and the limits of chest wall resection required to achieve adequate clear margins were so defined. A targeted 10 cm posterior incision (Figure 2) was performed to allow resection of posterior arches of the right 6th to 9th ribs, 7th and 8th transverse processes and related musculature. The chest wall defect was reconstructed with double-layer composite and rigid prosthesis (polypropylene mesh reinforced with gentamicin-impregnated methylmethacrylate cement).
The patient made an uneventful recovery with drain removal on day 2. He was discharged home on post-operative day 3.
The final histology report demonstrated a 14 cm × 9 cm mass infiltrating the upper lobe visceral pleura, the four ribs and paravertebral musculature, with clear margins throughout and no evidence of lymph node invasion pT3N0M0 stage IIB
After a multidisciplinary discussion an adjuvant chemotherapy regimen was planned and 3 courses of adjuvant Cisplatin and Vinorelbine was subsequently administered.
At 18-month follow-up, the patient is doing well, having returned to a normal level of activity with an isolated complaint of occasional low grade right sided chest pain well controlled by simple analgesia and no evidence of recurrence of disease at follow-up CT (Figure 1).
Discussion
The use of VATS for major pulmonary resections is replacing thoracotomy as the standard approach for the treatment of early stage lung cancer. This is due to at least equivalent oncologic outcome, lower overall complication rates, faster recovery from surgery with improved quality of life and shorter hospital stay with economic benefits.
Since the description of the first VATS lobectomy more than 20 years ago, there has been significant expansion in the applications of this approach, as surgeons deal with more ever advanced cases (nodal involvement, previous chemo- and/or radiotherapy, larger lesions, complex bronchial- and/or vascular reconstructions). The role and efficacy of VATS for these more complex procedures remains unknown.
Approximately 5% to 8% of patients presenting with lung cancer have chest wall invasion, with complete en bloc lung and chest wall resection remain the best chance of cure: with an expected 5-year survival of up to 40–50% in case of complete resection and the absence of nodal involvement.
The first description of the use of VATS for this purpose was provided by Widmann et al. in 2000 (1) who performed a complete thoracoscopic left upper lobe wedge resection en bloc with two ribs for a T3 chest wall adenocarcinoma without reconstruction of the defect, in a patient having undergone preoperative radiotherapy.
Since then, the use of minimally invasive techniques in this context—to accomplish, to facilitate or to assist the chest wall resection—has been reported only occasionally with few case reports or small series. There remains insufficient evidence in the literature regarding feasibility, safety and long term results; hence this approach still remain uncommon.
Opponents of the technique stress that any benefit brought about by VATS avoiding rib spreading and the incision of chest wall muscles and soft tissues is obscured by the insult that is extensive rib resection.
Numerous different techniques have been described: Demmy et al. (2) approach the rib resection with the internal view using a conventional rib cutter inserted through the ports and completing the video-lobectomy at the end in standard fashion; the lobe en-bloc with ribs could be retrieved through the utility mini-thoracotomy. This option appears adequate for small posterior located chest wall resections where neither large incisions nor reconstruction are required. Berry et al., from Duke University (3), presented a hybrid procedure using a longitudinal paraspinal counterincision over the site of invasion after completion of the thoracoscopic lobectomy dissection. Through this, standard tools can disconnect spinal elements under direct view or thoracoscopic guidance for a more precise chest wall resection and reconstruction. Gonzalez-Rivas follows the same technique and principles but through a single incision according to the VATS uniportal technique (4). Finally Bayarri et al. (5) used a single-port VATS incision to confirm chest wall invasion when suspected on CT scan and to determine the boundaries and location of involvement. In this manner they place the incision over the involved area without the need for extensive thoracotomies, subsequently completing the pulmonary resection through the space available after the rib excision without rib spreading (lung resection via the chest wall defect). They advocate at least three advantages: no need of large experience in VATS lobectomy, obtaining additional information by intra-operative staging (pleural, chest wall and lymph node), and appropriate guide to place the incision and avoid rib spreading.
Most of the reported thoracoscopic rib resections are apical or posterior (given the fact that these are essentially covered ribs, with scapula and dorsal musculature overlying) and involve few ribs (four or fewer). This lowers the definitive need for chest wall reconstruction and permits use of the anterior approach for the resection
Different instruments have been reported for thoracoscopic rib resection (endoscopic rib cutters, Gigli saw or long-handled osteotome), however, any conventional instrument could be considered appropriate particularly when undertaking an external approach under thoracoscopic vision.
The case has been highly selected (posterior involvement of 2 ribs) to offer the advantages of thoracoscopic lung resection and minimize trauma to the chest wall by means of the hybrid approach.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this mauscript and any accompanying images.
References
- Widmann MD, Caccavale RJ, Bocage JP, et al. Video-assisted thoracic surgery resection of chest wall en bloc for lung carcinoma. Ann Thorac Surg 2000;70:2138-40. [Crossref] [PubMed]
- Demmy TL, Nwogu CE, Yendamuri S. Thoracoscopic chest wall resection: what is its role? Ann Thorac Surg 2010;89:S2142-5. [Crossref] [PubMed]
- Berry MF, Onaitis MW, Tong BC, et al. Feasibility of hybrid thoracoscopic lobectomy and en-bloc chest wall resection. Eur J Cardiothorac Surg 2012;41:888-92. [Crossref] [PubMed]
- Gonzalez-Rivas D, Fernandez R, Fieira E, et al. Single-incision thoracoscopic right upper lobectomy with chest wall resection by posterior approach. Innovations (Phila) 2013;8:70-2. [Crossref] [PubMed]
- Bayarri CI, de Guevara AC, Martin-Ucar AE. Initial single-port thoracoscopy to reduce surgical trauma during open en bloc chest wall and pulmonary resection for locally invasive cancer. Interact Cardiovasc Thorac Surg 2013;17:32-5. [Crossref] [PubMed]