Unilateral absence of pulmonary artery associated with contralateral lung cancer
Introduction
Unilateral absence of the pulmonary artery (UAPA) is a rare congenital pulmonary vascular deformity in which the left or right pulmonary artery is completely absent. It is secondary to the resorption of the proximal sixth aortic arch or to a defective septation of the truncus arteriosus during embryogenesis (1). A literature review reveals that almost all reported cases of UAPA had a patent ductus arteriosus or ligamentum arteriosum ipsilateral to the absent pulmonary artery. When the connecting ductus arteriosus closes after birth, the ipsilateral pulmonary artery will lose its blood supply, shrink in size and become invisible on angiogram or echocardiogram (2). UAPA may occur as an isolated anomaly or be accompanied by other congenital cardiovascular malformations. In the absence of cardiac abnormalities, it may remain undiagnosed until adulthood when patients develop respiratory symptoms.
In 1868, Frantzel described the first case of UAPA (3) and Bockeria reported a total of 419 cases by 2010 (4). The estimated prevalence is very low, ranging from 1/200,000 to 1/300,000 (5). The occurrence of lung cancer in patients with UAPA is even rarer and experience with surgical management is very limited. To the authors’ knowledge, only six such cases have been reported in the English medical literature (6-11). In this paper, we describe our experience with UAPA complicated by contralateral lung cancer and make a literature review on this rare clinical condition, focusing on pathology and management strategies.
Case presentation
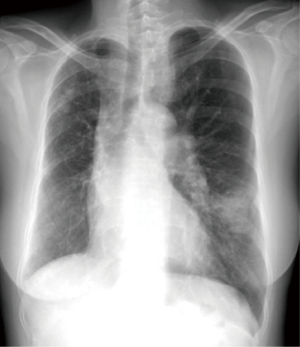
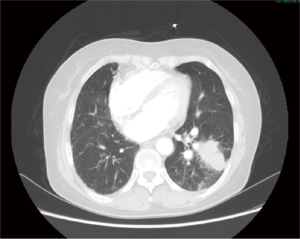
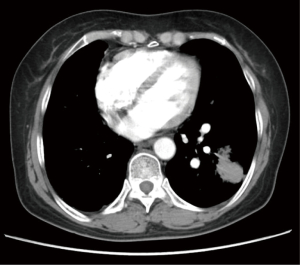
A 60-year-old female presented with a mass in the left lower lobe detected on a chest X-ray during routine medical checkup. Her past history included chronic recurrent bronchitis for 50 years, hypertension and diabetes for 9 years and excision of thyroid adenoma 2 years ago. Chest roentgenograph showed plethoric lung fields, a prominent left hilum and a mass in the left lower lobe measuring approximately 3 cm in diameter; the right hilum was shrunken, the volume of the right hemithorax was decreased, with mediastinal displacement to the right and grossly normal diaphragmatic locations (Figure 1). Pulmonary function tests revealed a forced vital capacity of 1.58 L (64.4% predicted), a forced expiratory volume in one second of 1.14 L (55.1% predicted) and a forced expiratory volume in the first second /forced vital capacity (FEV1/FVC) ratio of 0.92, compatible with moderately severe ventilatory dysfunction. A bronchoscopy revealed normal tracheobronchial anatomy of the right lung and left upper lobe. The orifice of the left lower lobe was slightly stenosed with dilated blood vessels on the mucosal surface. Electrocardiogram and echocardiogram revealed no cardiac defects. Computed tomography (CT) scan of the chest revealed a 3-cm irregular mass in the left lower lobe, interstitial changes in the right lung and mediastinal displacement to the right (Figures 2-4).
A primary diagnosis of lung cancer was made and it was decided that a lobectomy would be performed. Intraoperatively, a mass of 5 cm × 3 cm in diameter was found to be located in the left lower lobe. During one-lung ventilation, repeated decreases in arterial oxygen saturation (SaO2) were noted, which necessitated double lung ventilation. Although the reason for this inadequate ventilation could not be determined, a left lower lobectomy was performed with dissection of mediastinal lymph nodes. Postoperatively the SaO2 was 79–90% with endotracheal ventilation.
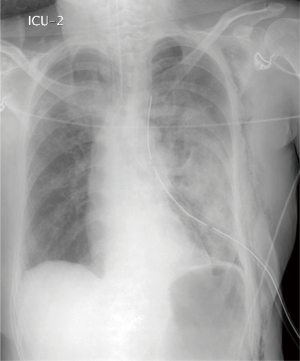
At the first postoperative day, the patient was somnolent. On examination, moist rales were heard in both lungs and tracheal excretions were bloody. Bedside chest roentgenogram showed multiple infiltrations in the left lung and positive end-expiratory pressure was initiated to improve oxygenation. However, the bloody tracheal excretions increased drastically and large moist rales were heard all over both lung fields. A repeat chest roentgenogram showed diffused infiltrations in the left upper lobe (Figure 5). At the second day, the patient deteriorated, her heart rate dropped to 23 beats per minute and she succumbed to ventricular ectopia and cardiac arrest.
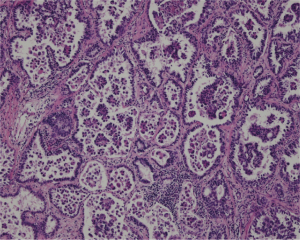
At the morbidity and mortality conference afterwards, reexamination of the chest CT scan revealed that the right pulmonary artery was absent, with diminished vascular markings in the right lung (Figure 3). Pathological examination of the lobectomy specimen revealed that the resected tumor was an adenocarcinoma with papillary and micropapillary features (Figure 6).
Discussion
Unilateral absence of a pulmonary artery is a rare congenital vascular malformation that was first described by Fraentzel in 1868 (3). It often occurs in association with other cardiovascular anomalies, such as congenital aortic deformities and conotruncal defects. Adult patients may develop symptoms such as hemoptysis, recurrent lung infections, and exertional dyspnea. However, approximately 13–15% of patients with UAPA have no symptomatic and UAPA remain undiagnosed until incidentally detected on imaging studies of the chest such as roentgenogram or CT scan (5). In a review by Ten Harkel and colleagues (12), 13.0% of patients (14/108) with UAPA were asymptomatic. Diagnosis of UAPA can be very difficult and should be considered on the basis of medical history, physical examination and imaging studies, including echocardiogram, chest roentgenograms, CT scans, perfusion scintigraphy and angiography (12-15). The typical findings on CT scans or roentgenograms may include elevation of the ipsilateral hemidiaphragm, a diminished hemithorax, a mosaic attenuation pattern, and displacement of the mediastinum, as well as interruption in the pulmonary artery and loss of normal pulmonary vascular markings (12,14-16). However, it should be noted that the affected lung is supplied by the bronchial, diaphragmatic, intercostal, or aortopulmonary collateral arteries that may be visualized on angiogram or echocardiogram (2). While intolerance of physical exercise, hemoptysis and recurring lung infections are common clinical symptoms, most adult patients with UAPA may remain asymptomatic. Up to date, no consensus exists on the management of patients with UAPA (5). Treatment strategies should be tailored to clinical presentations, anatomy and pathophysiology of the pulmonary arteries and associated cardiovascular defects, especially aortopulmonary collaterals. Surgical procedures may include lobectomy or pneumectomy, selective closure of aortopulmonary collaterals or single- or two-stage pulmonary artery anastomosis (5).
A search of the English literature reveals approximately 420 cases of unilateral absence of pulmonary artery (4), while only six cases of lung cancer associated with UAPA have been reported up to date (6-11). The current patient represents the 7th reported case of primary lung cancer in UAPA and the 2nd case of UAPA with primary carcinoma in the contralateral (normal) lung (Table 1). Diagnosis of UAPA with associated lung cancer is even more difficult. Of all 7 patients, CT scan is the most commonly diagnostic modality in 6; pathologic diagnosis was adenocarcinoma in 4, squamous cell carcinoma in 1, metastatic in 1 and not mentioned in 1. The lung cancer was surgically resected in 7/7 cases. In the present case, the diagnosis of UAPA was based upon the CT finding of an interrupted pulmonary artery. Unfortunately, due to our lack of a high index of awareness of this extremely rare anomaly and the negative findings of echocardiogram, it went unnoticed and no additional cardiopulmonary function tests were performed preoperatively.
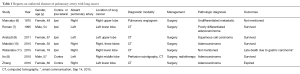
Full table
To the best of our knowledge, the current patient is the second case in which the contralateral (normal) lung was partially resected (8). In the present case, left lower lobectomy was performed through a thoracotomy, and intraoperatively repeated decreases were detected in SaO2 during one-lung ventilation, which necessitated release of the bronchial clamp and switch back to double lung ventilation.
This unusual association and the potential for causal relation between the two entities deserve further study. Knowledge and recognition of this rare and special condition may facilitate better diagnosis and treatment. Based on the lessons learned from the present case and literature review of six previous cases, we believe the following points are helpful in the management of UAPA associated with lung cancer.
First, prior to surgical resection of lung cancer, a high index of awareness of possible associated cardiac anomalies should be harbored, such as the extremely rare UAPA. It must be borne in mind that because lung resection will not only remove some pulmonary function but also some pulmonary vessels, right heart function and pulmonary pressure should be evaluated carefully before surgery. Second, if the lung cancer is ipsilateral to the UAPA, surgical resection, either limited or extensive, would be a safe approach in most cases (Table 1). In patients with absent left pulmonary artery and right lung cancer, limited resection (such as segmentectomy or wedge resection) may be feasible, as shown by the experience of Ito and associates (8). In patients with absent right pulmonary artery and left lung cancer, even limited resection is associated with very high mortality risks, as evidenced by the present case. Therefore, surgical excision should be contraindicated and non-surgical (radiation and chemotherapy) should be considered.
Conclusions
The occurrence of lung cancer in association with unilateral absence of pulmonary artery is a very rare clinical condition. This case highlights the importance of the clinical awareness of this potentially lethal congenital anomaly in light of its extreme rarity. Knowledge and recognition of this rare and special condition may facilitate better diagnosis and treatment of such patients. Management decision should be made based on the side of the lung cancer relative to the absent pulmonary artery.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient’s relative for publication of this manuscript and any accompanying images.
References
- Pool PE, Vogel JH, Blount SG Jr. Congenital unilateral absence of a pulmonary artery. The importance of flow in pulmonary hypertension. Am J Cardiol 1962;10:706-32. [Crossref] [PubMed]
- Welch K, Hanley F, Johnston T, et al. Isolated unilateral absence of right proximal pulmonary artery: surgical repair and follow-up. Ann Thorac Surg 2005;79:1399-402. [Crossref] [PubMed]
- Frantzel O. Angeborener Defekt der rechten Lungenarterie. Virchows Arch Pathol Anat 1868;43:420.
- Bockeria LA, Makhachev OA, Khiriev TKh, et al. Congenital isolated unilateral absence of pulmonary artery and variants of collateral blood supply of the ipsilateral lung. Interact Cardiovasc Thorac Surg 2011;12:509-10. [Crossref] [PubMed]
- Kruzliak P, Syamasundar RP, Novak M, et al. Unilateral absence of pulmonary artery: pathophysiology, symptoms, diagnosis and current treatment. Arch Cardiovasc Dis 2013;106:448-54. [Crossref] [PubMed]
- Mancebo A, Wanner A. Lung tumor in a patient with congenital unilateral hypoplasia of the pulmonary artery. Chest 1975;68:846-7. [Crossref] [PubMed]
- Roman J, Jones S. Case report: congenital absence of the left pulmonary artery accompanied by ipsilateral emphysema and adenocarcinoma. Am J Med Sci 1995;309:188-90. [Crossref] [PubMed]
- Ito M, Yamashita Y, Harada H, et al. Unilateral absence of the left pulmonary artery accompanied by right lung cancer. Ann Thorac Surg 2010;90:e6-8. [Crossref] [PubMed]
- Anstadt MP, Wozniak CJ, Sateesh SK, et al. Lobectomy for lung carcinoma with ipsilateral pulmonary artery agenesis. Am J Respir Crit Care Med American Thoracic Society International Conference Abstracts 2011;183:A3836.
- Makdisi G, Edell ES, Maleszewski JJ, et al. Pulmonary artery agenesis associated with emphysema and multiple invasive non-small cell lung cancers. Ann Thorac Surg 2015;99:2192-5. [Crossref] [PubMed]
- Watanabe Y, Shibuya J, Handa M, et al. Unilateral absence of the right pulmonary artery accompanied by right lung cancer. Ann Thorac Surg 2015;100:1113. [Crossref] [PubMed]
- Ten Harkel AD, Blom NA, Ottenkamp J. Isolated unilateral absence of a pulmonary artery: a case report and review of the literature. Chest 2002;122:1471-7. [Crossref] [PubMed]
- Bouros D, Pare P, Panagou P, et al. The varied manifestation of pulmonary artery agenesis in adulthood. Chest 1995;108:670-6. [Crossref] [PubMed]
- Sakai S, Murayama S, Soeda H, et al. Unilateral proximal interruption of the pulmonary artery in adults: CT findings in eight patients. J Comput Assist Tomogr 2002;26:777-83. [Crossref] [PubMed]
- Griffin N, Mansfield L, Redmond KC, et al. Imaging features of isolated unilateral pulmonary artery agenesis presenting in adulthood: a review of four cases. Clin Radiol 2007;62:238-44. [Crossref] [PubMed]
- Camera L, Fusari M, Calabrese M, et al. Isolated unilateral absence of pulmonary artery mimicking chronic pulmonary embolism at chest X-ray: multidetector-row CT angiographic findings. Clin Imaging 2012;36:845-9. [Crossref] [PubMed]