Image-guided localization of small lung nodules in video-assisted thoracic surgery
Birth of the hybrid era
For most of the pulmonary nodules discovered incidentally by thoracic imaging, the likelihood of them becoming malignant varies according to their size. For lesions smaller than 4 mm, the probability is only 1%, whereas it is 10–20% for nodules between 8 to 20 mm and 50% for those whose size is greater than 20 mm (1,2). Despite the fact that small nodules tend to be benign rather than malignant, such nodules may require a more invasive approach in terms of diagnosis and excision because of the low accuracy rate and false-negative biopsy samples via conventional percutaneous approaches and bronchoscopy.
Single-port video-assisted thoracic surgery (VATS), which is gaining increasing worldwide popularity (3-5), may be even more problematic for localizing pulmonary lesions. This potentially less invasive approach, compared with conventional VATS, further limit surgeons from effectively palpating lesions through a single intercostal access, particularly lesions located at a distance from the pleural surface or those presenting as part-solid lesions with high ground-glass opacity (GGO) (6). Therefore, preoperative adjunctive localization techniques such as hookwire/microcoil placement or dye labeling conducted under computed tomography guidance have shown promising results in identifying pulmonary lesions. Nevertheless, these approaches inevitably increase the cost, complication, and complexity of care, all of which lead to a considerable logistic burden. The use of hybrid operating room (OR) may have implications in terms of time and cost savings, as well as a reduction in the rate of pneumothorax, marker dislodgement, and dye diffusion. Thus, a less invasive diagnostic and therapeutic option for patients could be provided. More importantly, surgeons could perform precise excisions much more safely, even for multifocal lesions, sparing pulmonary tissues thanks to a robust method of diagnosing and localizing the nodules.
Preclinical study
Mobile cone-beam computed tomography (CBCT) has the ability to provide sub-millimeter spatial resolution combined with soft tissue visibility even at a low radiation dose (~4.3 mGy/scan) for thoracic spine surgery (7). With a significantly reduced contrast, depending on air volume retention in the collapsed lungs during surgery, the visibility of nodules in CBCT can be challenging. In 2013, Uneri and colleagues (8) proposed the use of intraoperative CBCT and two-step deformable image registration to guide the targeting of small lesions in twelve porcine specimens under VATS. This study provided new insights into centralizing the localization, diagnosis, and treatment procedures in a hybrid OR. In detail, a robust model-driven method was used to match the pleural surface and bronchial structures between inflation and deflation, achieving a coarse localization of the target wedge with an associated error of less than 3–5 mm. Subsequently, a finer image-driven stage that employed an intensity-corrected algorithm was used to decrease the registration error to an accuracy of 1–2 mm for both the lesion and surrounding critical structures.
The preliminary results promised to meet the requirements of VATS, since the geometric accuracy quantified by the target registration error in the anatomical targets was 1.9 mm [95% confidence interval (CI) maximum =5.0 mm] for the model-driven stage, and 0.6 mm (95% CI maximum =4.1 mm) for the subsequent image-driven stage. Moreover, this scan protocol demonstrated good visibility in deflated lung tissue with a slightly increased dose (~4.6–11.1 mGy). As a result, clinicians would be confident in identifying a lesion regardless of its radiological density (e.g., GGO) and could evaluate potential handicaps in the hybrid OR; for instance, is there a bronchus sign that indicates a direct route for biopsy via bronchoscopy, or are there any adjacent vascular structures that clinicians should be aware of during implantation of a metallic marker?
In addition, preoperative CT imaging could be incorporated into the intraoperative CBCT, aligning preoperative planning with on-table data, which may potentially provide intraoperative segmentation anatomy for a target lesion (9).
Building a hybrid theater
The integration of real-time on-table image guidance technology into clinical practice is well established in other specialties, including cardiovascular and orthopedic surgery. Anecdotal reports of the use of a portable O-arm CBCT device to detect pulmonary lesions (10) have helped to inform the use of the hybrid technique in the field of thoracic surgery, though the technique may have shortcomings in that it lacks a pre-determined scanning field, which may potentially lead to an increase in intraoperative radiation exposure (6). The idea has also proved to be feasible within pediatric surgery (11). The first comprehensive hybrid suite and procedural flow for thoracic surgery was introduced by the Brigham and Women’s Hospital group in 2013, with the Advanced Multimodal Image-Guided Operating (AMIGO) suite (12) for image-guided VATS (iVATS). The 5,700 square feet AMIGO suite has three separate but integrated rooms that incorporate CT, magnetic resonance imaging, near-infrared imaging, and positron emission tomography, offering tremendous assistance in the multidisciplinary treatment of a variety of diseases. The sophisticated imaging system in the AMIGO suite may have further implications for intraoperatively investigating the extent of invasion in the treatment of thoracic inlet tumors.
A smaller suite, relatively speaking, (approximately 760 square feet) was established in our center (13). This suite also implemented a multidisciplinary design and has proven capable of image-guided electromagnetic navigation bronchoscopy (ENB) (14) and VATS procedures, including the single port approach (13). The high flexibility of the floor-mounted devices allows them to be moved quickly from a distant parked position to the surgical field without interfering with the laminar airflow; thus, the OR can be highly utilized for multidisciplinary work. The detailed contents of the hybrid OR are described in Table 1.
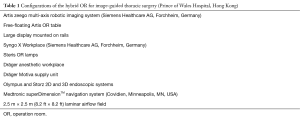
Full table
Image-guided ENB diagnostic procedure in the hybrid OR
As one of the most interesting advanced bronchoscopic techniques, ENB utilizes electromagnetic sensor technology in combination with virtual three-dimensional (3D) bronchial reconstruction of CT images that can be paired with the true bronchoscopic images (15). Once the tip of the localization guide approaches the proximity of the lesion during the navigational phase, the localization guide will then be withdrawn, leaving the extended working channel (EWC) locked onto the bronchoscope. Physicians are then able to deliver a steerable catheter for biopsy or to insert markers. The mean accuracy of the navigation system, measured by the ‘average fiducial target registration error’ (AFTRE), defined as the distance between the marked structures on the planning CT images and the registration points recorded by bronchoscopy, was reported to range from 2.85 to 9.53 mm (mean, 6.12 mm; SD, 1.7 mm) in a pilot study (n=30) (16). Another study with a larger number of enrolled cases (n=92) showed that the mean AFTRE was 9±6 mm (range, 1–31 mm) and that the diagnostic yield was independent of lesion size (17). Indeed, it was suggested that an AFTRE of ≤4 mm would lead to a higher diagnostic accuracy (77.2% vs. 44.4%; P =0.03) (18). It should however be noted that these studies are based on systems and software that are a decade or so ago.
The navigational error may explain the results from a recent multi-institutional study that included 581 patients, in which the diagnostic yield of the ENB technique alone was 38.5%, which was lower than previous studies that ranged from 68% to 71% (19). One argument was that continuous biopsy hits, with limited variation, were of limited added value with regard to target examination when the EWC diverged from the target, leading to an ‘all or none’ phenomenon. Usually, fluoroscopy or radial probe endobronchial ultrasound (EBUS) is employed to indicate the position of the sensor probe in real time. However, such methods do not obviate the fundamental problem of the navigational error: we cannot be sure whether the tip of the catheter is inside the difficult-to-reach lesion. Perhaps more importantly, the movement of the EWC from the torque exerted during deployment of the biopsy tool could also contribute significantly to navigation biopsy error.
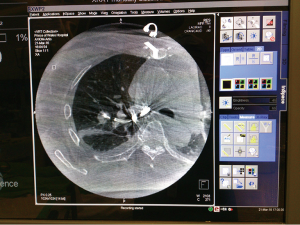
To further improve the accuracy and applicability of this technology, we recently reported the use of integrated CBCT (syngo dynaCT; Siemens Healthcare AG, Forchheim, Germany) and ENB in a hybrid OR, providing unparalleled real-time images to guide and confirm the successful navigation to, and biopsy of, an 8-mm lesion located in the right middle lobe (14). Briefly, the navigation system is switched off after the EWC has been anchored according to the guiding plan with the biopsy tool deployed, and then the Artis zeego multi-axis robotic imaging system (Siemens Healthcare AG, Forchheim, Germany) is moved to the working system without altering the position of the patient. A 6-second suspension of ventilation allows the intraoperative dynaCT to visualize the current biopsy tools and lesion. A non-metallic device mounted on the table is used to hold the bronchoscope still during scanning (Figure 1). Normally, two intraoperative scans are required: one to identify any minor misdirection and the second to confirm the biopsy after any necessary adjustment has taken place. To further decrease the exposure to radiation, two fluoroscopic shots taken from different angles by the dynaCT can orientate the catheter after 2D/3D fusion with the preoperative CT data; thus, the radiation dose is comparable to a preoperative percutaneous biopsy. The image from the dynaCT in the hybrid OR reveals its superior accuracy over fluoroscopy or EBUS in determining the direction of the catheter tip, as it provides undisputable evidence of whether the tip has reached the target (Figure 2). Hence, the navigational error can be decreased, particularly when dealing with GGO lesions of less than 10 mm that are generally poorly visualized on standard fluoroscopy and EBUS.

Recently, Marino et al. (21) reported the largest series to date on ENB-guided trans-bronchial injection of dye followed by VATS sublobar resection. Of the 72 pulmonary nodules that ranged in size from 4–17 mm (median, 8 mm), 70 were successfully identified without complication. In their technique, one shot of methylene blue (<0.5 mL) was injected into the nodule and another shot was given to mark the pleura if the nodule was located more than 5 mm from the pleural surface. One case experienced dye extravasation but was palpated intraoperatively. Undoubtedly, the hybrid technique would allow for the more precise placement of marking dye in close proximity to lesions for resection margin guidance under single-port VATS, representing a future direction for this technology (22).
Image-guided metallic implantation in the hybrid OR
The preoperative implantation of a radiopaque metallic material such as a hookwire or microcoil under CT guidance has been adopted by many thoracic surgeons and has provided the highest level of evidence for the efficacy of intraoperative localization (with a success rate of up to 94% and 100% for the hookwire and microcoil, respectively) (23). The drawback of a lack of tactile sense during single port VATS can be compensated for by visualizing these metallic materials with part of the filament left outside the pleural surface, or detected through intraoperative fluoroscopy. In addition, gentle extrathoracic manipulation of the outer filament of the wire may allow for traction of the lung nodule in directions that would facilitate resection (24). Classically, these techniques require localization to be performed in the radiology suite followed by surgery in the OR. During the time incurred in transporting patients to the OR, patients might experience discomfort and suffer from various complications such as pneumothorax or dislodgement of the localizing material (6). Approximately 24% of patients who undergo hookwire insertion are likely to experience pneumothorax and 2–4% of them may require chest tube drainage prior to surgery. Wire dislodgement from the mounting pleura remains the major factor (2–10%) in the failure of localization, which is a higher rate than for microcoil implantation (2.7%) (23). However, the pneumothorax rate associated with the microcoil cannot be ignored which has been reported to be as high as 13%, though a chest tube was rarely needed in these cases (25).
As discussed above, the iVATS program proposed by the Brigham and Women’s Hospital group attempted to simultaneously centralize the implantation procedure with subsequent surgery in the AMIGO theater, and showed this technique to be advantageous compared to conducting these procedures separately. In their phase I−II study, 23 pulmonary lesions of size 1.30±0.38 cm received conventional thoracoscopic surgery after the placement of two T-shaped fiducials (Kimberly-Clark, Roswell, GA, USA) under intraoperative C-arm CT; of these, 22 were found to be malignant (26). A 5-second end-inspiratory-hold 200° rotation with a 0.36 mGy/projection scanning protocol for the pre-determined field was able to identify the nodule by CBCT. Two T-bar fiducials were implanted afterwards for localization under fluoroscopic guidance according to the trajectory provided by the syngo iGuide needle guidance software (Siemens Healthcare AG, Forchheim, Germany). Notably, the T-bars were successfully implanted in 20 (87.0%) cases, with median procedure duration of 39 min. The average and total procedure radiation doses were low (median: 1,501 mGy × m2; range, 665–16,326 mGy × m2). Interestingly, no implantation-associated complication was found, compared with the traditional two-site approach.
Furthermore, the iVATS protocol may provide a minimally-invasive service through single-port VATS, since our group reported the world’s first image-guided single-port VATS (iSPVATS) major lung resection for a GGO nodule that underwent dynaCT-guided hookwire placement in the hybrid OR (13). Generally, two fluoroscopic shots by the dynaCT are administered to ensure that the lesion is in the isocenter of the CBCT, and optimal tube parameters will be automatically created to provide a 3D real-time image of the thorax. On the syngo X Workplace, the interventional radiologist deploys the hookwire to the chest and the position of the needle is further verified by the control scans. Optionally, the Artis zeego can be equipped with a laser cross indicator to aid the puncturing process under the guidance of the iGuide software mentioned above. Approximately 30 min is needed to localize and place a hookwire; the radiation exposure level for this procedure is comparable to the conventional percutaneous technique in the radiology suite. Pulmonary deflation after the introduction of one-lung ventilation may theoretically cause wire dislodgement, but this could also be solved immediately by re-localizing the lesion in the hybrid unit, as the CBCT is able to visualize the pulmonary structure in a collapsed lung (8). Our hookwire iSPVATS technique would work perfectly for peripheral lesions of even sub-centimeter size, and may reduce the risk of complications associated with marker implantation. Moreover, a precise localization of the lesion may reduce the chance of resecting excessive pulmonary tissue. However, technical limitations remain as nodules that are located near to the apex and diaphragm can be difficult to approach using the percutaneous wire.
Initial results of hookwire placement in a hybrid OR
Thus far, we have attempted 19 consecutive cases under minimally-invasive sublobar resection of small pulmonary nodules with real-time image-guided hookwire localization in the hybrid OR between February 2014 and October 2015. The mean nodule size was 7.7±3.4 mm (range, 2–15 mm) and all of them were accurately localized by hookwire and successfully resected. VATS resections were immediately performed in the hybrid OR after hookwire insertion. Five (26.3%) patients developed pneumothorax after hookwire insertion but none required intervention. The mean operating time was 128.5±60.6 minutes, and the mean blood loss was 25.5±15.0 mL. The mean chest drainage duration was 2.6±0.9 days and the postoperative length of hospital stay was 3.6±1.7 days. No postoperative complications or mortality occurred. In terms of the histology, 14 (73.7%) malignant and five benign lesions were identified, all with adequate resection margins. This preliminary cohort showed that real-time image-guided hookwire localization in the hybrid OR setting is a safe and effective technique for VATS resection for tiny lung nodules (27).
Conclusions
Precise localization is of paramount importance in the management of small pulmonary lesions; especially in the era of single port VATS. Centralization of the diagnostic and localizing procedures within a specially designed hybrid theater could enhance diagnostic accuracy as well as remove the complications associated with the implantation of metallic markers. By using ENB under CBCT guided real-time adjustment, the chance of biopsy errors are reduced, consequently avoiding missing important pathology and unnecessary excision(s) particularly when dealing with multiple lesions. Dye labeling via ENB, which has recently been shown to be a powerful method for localizing small pulmonary lesions for sublobar resection, may also benefit from the hybrid strategy to increase marking precision and resection margin accuracy. The iSPVATS idea, using a hookwire/microcoil, allows for a safer percutaneous procedure in the OR environment and minimizes the chance of dislodgement, which leads to failed localization. Moreover, the CBCT could provide salvage localization in the case of rare dislodgement, as it is capable of visualizing a deflated lung.
The concept of minimally invasive thoracic surgery is evolving from simply reducing the number of surgical incisions to becoming a more sophisticated art of minimizing surgical insult to the patient by for example, lung preserving surgical resections through improved localization procedures, or fast-tracking using techniques such as non-intubated anesthesia (28). It is anticipated that the hybrid OR will play an increasingly important role in this exciting progress as it establishes a cost-effective, one-stop procedural flow for image-guided thoracic surgery. Advanced hybrid ORs, like the AMIGO suite, that incorporate other modalities of imaging may have implications in providing additional information and details for safer and more efficient surgery of the future.
Acknowledgements
None.
Footnote
Conflicts of Interest: CS Ng has an electromagnetic navigational bronchoscopy system SuperDimension Version 7 on loan from Medtronic. And other authors have no conflicts of interest to declare.
References
- MacMahon H, Austin JH, Gamsu G, et al. Guidelines for management of small pulmonary nodules detected on CT scans: a statement from the Fleischner Society. Radiology 2005;237:395-400. [Crossref] [PubMed]
- Midthun DE, Swensen SJ, Jett JR, et al. Evaluation of nodules detected by screening for lung cancer with low dose spiral computed tomography. Lung cancer 2003;41:S40. [Crossref]
- Ng CS, Lau KK, Gonzalez-Rivas D, et al. Evolution in surgical approach and techniques for lung cancer. Thorax 2013;68:681. [Crossref] [PubMed]
- Ng CS, Rocco G, Wong RH, et al. Uniportal and single-incision video-assisted thoracic surgery: the state of the art. Interact Cardiovasc Thorac Surg 2014;19:661-6. [Crossref] [PubMed]
- Zhao ZR, Li Z, Situ DR, et al. Recent clinical innovations in thoracic surgery in Hong Kong. J Thorac Dis 2016;8:S618-S626. [Crossref] [PubMed]
- Zhao ZR, Lau RW, Ng CS. Hybrid theatre and alternative localization techniques in conventional and single-port video-assisted thoracoscopic surgery. J Thorac Dis 2016;8:S319-27. [PubMed]
- Schafer S, Nithiananthan S, Mirota DJ, et al. Mobile C-arm cone-beam CT for guidance of spine surgery: image quality, radiation dose, and integration with interventional guidance. Med Phys 2011;38:4563-74. [Crossref] [PubMed]
- Uneri A, Nithiananthan S, Schafer S, et al. Deformable registration of the inflated and deflated lung in cone-beam CT-guided thoracic surgery: initial investigation of a combined model- and image-driven approach. Med Phys 2013;40:017501. [Crossref] [PubMed]
- Nithiananthan S, Schafer S, Uneri A, et al. Demons deformable registration of CT and cone-beam CT using an iterative intensity matching approach. Med Phys 2011;38:1785-98. [Crossref] [PubMed]
- Ohtaka K, Takahashi Y, Kaga K, et al. Video-assisted thoracoscopic surgery using mobile computed tomography: new method for locating of small lung nodules. J Cardiothorac Surg 2014;9:110. [Crossref] [PubMed]
- Narayanam S, Gerstle T, Amaral J, et al. Lung tattooing combined with immediate video-assisted thoracoscopic resection (IVATR) as a single procedure in a hybrid room: our institutional experience in a pediatric population. Pediatr Radiol 2013;43:1144-51. [Crossref] [PubMed]
- Advanced Multimodality Image Guided Operating (AMIGO). Available online: http://www.brighamandwomens.org/research/amigo/default.aspx, accessed 20th July 2016.
- Ng CS, Man Chu C, Kwok MW, et al. Hybrid DynaCT scan-guided localization single-port lobectomy. Chest 2015;147:e76-8. [corrected]. [Crossref] [PubMed]
- Ng CS, Yu SC, Lau RW, et al. Hybrid DynaCT-guided electromagnetic navigational bronchoscopic biopsy†. Eur J Cardiothorac Surg 2016;49 Suppl 1:i87-8. [PubMed]
- Schwarz Y, Mehta AC, Ernst A, et al. Electromagnetic navigation during flexible bronchoscopy. Respiration 2003;70:516-22. [Crossref] [PubMed]
- Becker HD, Herth F, Ernst A, et al. Bronchoscopic biopsy of peripheral lung lesions under electromagnetic guidance: a pilot study. J Bronchol 2005;12:9-13. [Crossref]
- Eberhardt R, Anantham D, Herth F, et al. Electromagnetic navigation diagnostic bronchoscopy in peripheral lung lesions. Chest 2007;131:1800-5. [Crossref] [PubMed]
- Makris D, Scherpereel A, Leroy S, et al. Electromagnetic navigation diagnostic bronchoscopy for small peripheral lung lesions. Eur Respir J 2007;29:1187-92. [Crossref] [PubMed]
- Ost DE, Ernst A, Lei X, et al. Diagnostic Yield and Complications of Bronchoscopy for Peripheral Lung Lesions. Results of the AQuIRE Registry. Am J Respir Crit Care Med 2016;193:68-77. [Crossref] [PubMed]
- Zhao ZR, Lau RW, Ng CS, et al. Hybrid theater with cone-beam computed tomography (CBCT) image-guided electromagnetic navigation bronchoscopy (ENB) at Prince of Wales Hospital, The Chinese University of Hong Kong. Asvide 2016;3:398. Available online: http://www.asvide.com/articles/1169
- Marino KA, Sullivan JL, Weksler B. Electromagnetic Navigation Bronchoscopy for Identifying Lung Nodules for Thoracoscopic Resection. Ann Thorac Surg 2016;102:454-7. [Crossref] [PubMed]
- Rocco R, Rocco G. Future study direction on single port (uniportal) VATS. J Thorac Dis 2016;8:S328-32. [PubMed]
- Kidane B, Yasufuku K. Advances in Image-Guided Thoracic Surgery. Thorac Surg Clin 2016;26:129-38. [Crossref] [PubMed]
- Ng CS, Hui JW, Wong RH. Minimizing single-port access in video-assisted wedge resection, with a hookwire. Asian Cardiovasc Thorac Ann 2013;21:114-5. [Crossref] [PubMed]
- Finley RJ, Mayo JR, Grant K, et al. Preoperative computed tomography-guided microcoil localization of small peripheral pulmonary nodules: a prospective randomized controlled trial. J Thorac Cardiovasc Surg 2015;149:26-31. [Crossref] [PubMed]
- Gill RR, Zheng Y, Barlow JS, et al. Image-guided video assisted thoracoscopic surgery (iVATS) - phase I-II clinical trial. J Surg Oncol 2015;112:18-25. [Crossref] [PubMed]
- Yu PS, Lau RW, Capili GF, et al. Minimally-Invasive Sublobar Resection of Tiny Pulmonary Nodules with Real-Time Image Guidance in the Hybrid Theatre. Innovations 2016;11:S98-S99.
- Zhao ZR, Lau RW, Ng CS. Non-intubated video-assisted thoracic surgery: the final frontier? Eur J Cardiothorac Surg 2016. [Epub ahead of print]. [Crossref] [PubMed]


