Preoperative computed tomography-guided dye injection to localize multiple lung nodules for video-assisted thoracoscopic surgery
Introduction
The detection of small early lung cancer is increasing, in part due to the implementation of lung cancer screening programs using low-dose computed tomography (CT) (1). Percutaneous CT-guided core biopsy is a minimally invasive tool used to diagnose early lung cancer (2,3). However, the false negative rate of CT-guided biopsies is high, particularly if the lesions are small, necrotic, or coexist with inflammatory processes (4). A small CT-guided biopsy specimen size may underestimate the histological grade or stromal invasion in early lung cancer (5). Video-assisted thoracoscopic surgery (VATS) has been demonstrated to be both diagnostically and therapeutically beneficial for the resection of small lung nodules, and especially for subsolid lung nodules (6). For early lung cancer, VATS with sublobar resection has been reported to be equivalent to lobectomy in terms of recurrence and overall survival (7). However, it is challenging to visualize or palpate small and deep lung nodules during VATS due to a limited field of view. Some small nodules, especially nonsolid or subsolid nodules, have similar rigidity to normal lung parenchyma due to replacement growth in early lung cancer. The rate of conversion from VATS to thoracotomy to locate small lung nodules has been reported to be as high as 63% without preoperative image-guided localization (8). CT-guided preoperative localization was introduced to help surgeons accurately locate such small lung nodules (9). Various CT-guided localization methods have been developed, including Lipiodol (10), wire (11), and microcoil (12). In this study, we investigated the safety and feasibility of CT-guided Patent Blue V (PBV) dye localization in multiple pulmonary lung nodules.
Methods
From January 2013 to December 2015, a total of 704 patients received preoperative CT-guided PBV dye localization for VATS at our hospital. Among them, 100 consecutive patients underwent CT-guided PBV dye location for more than two lesions during the same procedure (26 males, 74 females, mean age ± standard deviation 60±11 years). Clinical parameters including age, gender, history of smoking, cancer, prior lung surgery, operative method, and postoperative hospitalization stay were reviewed (Table 1).
Full table
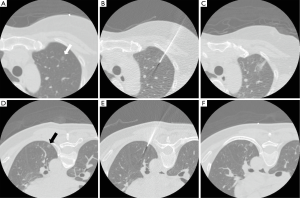
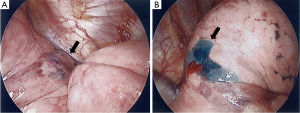
The CT-guided PBV dye localization procedure has previously been described in detail (13). All of the patients were required to stop taking antiplatelet agents 5 days before the procedure, had a platelet count of more than 80×103/µL, and normal prothrombin and activated partial thromboplastin time. Before the CT-guided localization procedure, the patients were placed in the supine, prone, or oblique position according to the planned needle path after reviewing prior CT images. The path was planned to be as short as possible while avoiding transfissural punctures or being oriented towards major vascular structures. These procedures were performed on a 16-slice CT scanner (GE LightSpeed; GE Healthcare, Milwaukee, Wisconsin, USA) using a low-dose exposure, thin slice protocol (1.25 mm thickness, 1.3 pitch, 0.7 sec/rotation, 120 kV, 50 mA). After injecting 10 mL of local anesthetic (Xylocaine, 2%, Recipharm Monts, Monts, France), a 22-gauge Chiba needle was gradually advanced under CT-guidance until it reached the target lesion. A total of 0.1–0.3 mL PBV dye (2.5%; Guerbet, Aulnay-sous-Bois, France) was then injected via the Chiba needle. The needle was then withdrawn to subpleural lung parenchyma to allow for a second injection of dye to ensure visibility during VATS if the nodule was deeply located (Figure 1). These two areas were both stained so that once the stained lung surface was identified by the surgeon, electrocauterization could be performed to reveal another stained deep target region, which could then be resected by endoscopic stapling. Post-localization CT scanning was performed to evaluate potential complications. The patients were then transferred back to the surgical ward to await surgery (Figure 2). Oxygen delivery was given via a nasal cannula and strict bed rest was required until surgery. The localization procedures were performed by one of ten radiologists (with 5–25 years of experience in thoracic imaging) in our department.
The number of nodules localized in each patient, nodule size, nodule consistency, depth from the pleura or fissure, length the needle traversed in the lung, amount of injected dye, failure rate, complications, CT localization and operative procedural time were recorded. The measurements were performed using a commercial PACS system (IMPAX 6.5; Agfa HealthCare, Mortsel, Belgium). Technical failure was defined as the surgeon being unable to visualize the stained area. The CT localization procedure time was defined as the time interval from the first to the last (post-procedure) CT scan, which was calculated from image metadata. Pneumothorax was graded as mild (<1 cm), moderate (1–2 cm), or large (>2 cm). Hemorrhage was graded as mild (less than one segment), moderate (less than one lobe), or large (more than one lobe).
This retrospective study was approved by the Institutional Review Board of our hospital. The requirement of informed consent was waived.
Results
Table 1 shows the patients’ information and nodule characteristics. There were a total of 217 nodules in the 100 patients. Eighty-five patients had two nodules, 13 had three nodules, and two had four nodules that underwent CT-guided localization. Most patients were nonsmokers (n=87). In the 13 patients with a smoking history, four had visible emphysema on CT images. Forty-one patients had a history of cancer. Fourteen patients had a history of prior lung surgery (three on the same side as the targeted nodules, 11 on the contralateral side).
There were 61 nodules in the right upper lobe, 26 nodules in the right middle lobe, 47 nodules in the right lower lobe, 44 nodules in the left upper lobe (LUL), and 39 nodules in the left lower lobe (LLL). The mean size of the nodules was 0.8±0.4 cm (range, 0.3–2.2 cm). Only one nodule was larger than 2 cm in diameter. Among these 217 nodules, there were 90 solid nodules (41%), 25 part-solid nodules (12%), 99 ground glass nodules (GGN) (46%), and three cavitary nodules (1%). The mean depth of the nodule from the pleura or fissure was 0.7±0.7 cm (range, 0–3.9 cm). Final histopathological diagnosis showed that 151 nodules were malignant (70%) and 66 were benign.
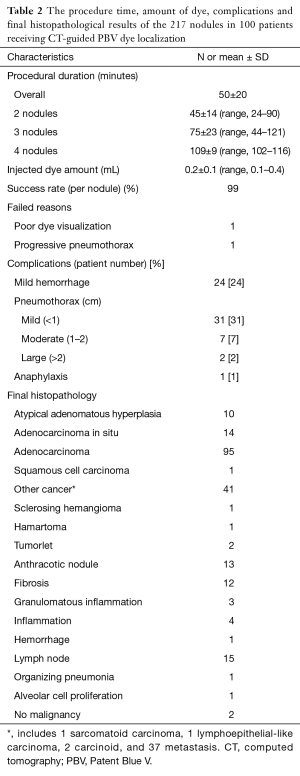
The procedural time of CT-guided localization, amount of dye and operative results are listed in Table 2. The mean procedural time for localization was 45±14 minutes for two nodules, 75±23 minutes for three nodules, and 109±9 minutes for four nodules. The overall mean procedural time was 50±20 minutes. The average volume of injected dye was 0.2±0.1 mL (range, 0.1–0.4 mL). Five nodules required transfissural punctures to reach the lesion, two of which showed only mild pneumothorax post-procedurally. Another three nodules required two needle passes because of inconsistent respiration.
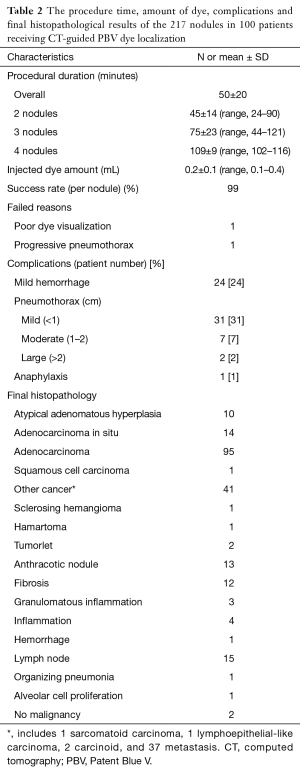
Full table
Dye localization failed in two nodules (technical success rate 99%). Poor dye identification was found in one of these lesions, and progressive pneumothorax with the needle being unable to reach the target in the other. Both patients successfully underwent wedge resection after the surgeons carefully determined the location of the nodule from preoperative CT images.
Mild lung hemorrhage occurred in 24 patients, and pneumothorax occurred in 40 patients (mild 31, moderate 7, and large 2). All patients with pneumothorax remained asymptomatic, and none required further drainage before surgery. One patient who underwent localization for two nodules developed a skin rash and hypotension after being injected with 0.4 mL PBV dye. After resuscitation, the patient recovered and successfully underwent nodule resection (14).
The mean operative time was 134±73 minutes. Wedge resection was performed for 191 nodules, segmentectomy for 22 nodules, and lobectomy for four nodules. Segmentectomy or lobectomy was performed instead of wedge resection if the surgeon judged the section margin to be limited. The mean overall admission period was 6.4±4.4 days.
Discussion
Our results showed that CT-guided PBV dye localization for multiple pulmonary nodules had a high technical success rate (99%), and thus aided the thoracic surgeons to locate multiple small pulmonary nodules and perform resection. The complications were well-tolerated, except for one case with anaphylaxis after PBV dye injection (14). PBV dye has been widely used in breast sentinel lymph node biopsies, with incidence rates of an anaphylactic reaction ranging from 0.6–2.7% (15,16).
Various methods and materials have been proposed for preoperative localization including using a localization wire (11), radiotracer (17), Lipiodol (10), and a microcoil (12). The disadvantages of PBV dye localization are due to its physical property. It may be harder to visualize the injected dye in severely anthracotic and pigmented lung surfaces. PBV dye diffuses and is absorbed with time, and therefore surgery is preferred on the same day. In addition, the surgeons cannot use palpation as with wire or microcoil localization to assist in locating the nodules. The advantages of dye injection are its simplicity. Small gauge needles are used in CT-guided dye localization, which minimizes patient discomfort and the risk of complications, even if transfissural punctures are needed. In addition, no additional radiation exposure (such as from a radiotracer or intraoperative fluoroscopy) is required for either the patient or surgeon. Overall, the technical success rate enabling visualization of the injected dye and resection was high in this study (99%), which is comparable to other localization techniques.
CT-guided dye localization has limitations with deep lesions due to non-visualization of the dye on the lung surface. However, we found that by injecting the PBV dye at the lesion site and subpleural lung for visual confirmation, the surgeons could locate the direction of the small deep lung nodule and perform resection.
There are several limitations to this study. First, it is a retrospective study, and prospective studies are needed to mitigate bias and explore the efficacy and effectiveness of CT-guided dye localization. Second, different surgical techniques are used for resection (VATS, robotic-assisted thoracoscopic surgery, non-intubated VATS), and this can cause great variability in assessing surgical efficacy. However, the high technical success rate using CT-guided dye location is probably not directly relevant to different surgical methods of VATS.
Conclusions
CT-guided PBV dye localization for multiple pulmonary nodules is a feasible and safe method, with high technical success rate. It can facilitate surgeons to perform multiple sublobar resections in one surgery.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the National Taiwan University Hospital Research Ethics Committee (No. 201607035RINB) and the requirement of informed consent was waived in this retrospective study.
References
- National Lung Screening Trial Research Team, Aberle DR, Adams AM, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 2011;365:395-409. [Crossref] [PubMed]
- Chang YC, Yu CJ, Lee WJ, et al. Imprint cytology improves accuracy of computed tomography-guided percutaneous transthoracic needle biopsy. Eur Respir J 2008;31:54-61. [Crossref] [PubMed]
- Choi SH, Chae EJ, Kim JE, et al. Percutaneous CT-guided aspiration and core biopsy of pulmonary nodules smaller than 1 cm: analysis of outcomes of 305 procedures from a tertiary referral center. AJR Am J Roentgenol 2013;201:964-70. [Crossref] [PubMed]
- Montaudon M, Latrabe V, Pariente A, et al. Factors influencing accuracy of CT-guided percutaneous biopsies of pulmonary lesions. Eur Radiol 2004;14:1234-40. [Crossref] [PubMed]
- Lu CH, Hsiao CH, Chang YC, et al. Percutaneous computed tomography-guided coaxial core biopsy for small pulmonary lesions with ground-glass attenuation. J Thorac Oncol 2012;7:143-50. [Crossref] [PubMed]
- Naidich DP, Bankier AA, MacMahon H, et al. Recommendations for the management of subsolid pulmonary nodules detected at CT: a statement from the Fleischner Society. Radiology 2013;266:304-17. [Crossref] [PubMed]
- Cao C, Gupta S, Chandrakumar D, et al. Meta-analysis of intentional sublobar resections versus lobectomy for early stage non-small cell lung cancer. Ann Cardiothorac Surg 2014;3:134-41. [PubMed]
- Suzuki K, Nagai K, Yoshida J, et al. Video-assisted thoracoscopic surgery for small indeterminate pulmonary nodules: indications for preoperative marking. Chest 1999;115:563-8. [Crossref] [PubMed]
- Dowling RD, Keenan RJ, Ferson PF, et al. Video-assisted thoracoscopic resection of pulmonary metastases. Ann Thorac Surg 1993;56:772-5. [Crossref] [PubMed]
- Watanabe K, Nomori H, Ohtsuka T, et al. Usefulness and complications of computed tomography-guided lipiodol marking for fluoroscopy-assisted thoracoscopic resection of small pulmonary nodules: experience with 174 nodules. J Thorac Cardiovasc Surg 2006;132:320-4. [Crossref] [PubMed]
- Gossot D, Miaux Y, Guermazi A, et al. The hook-wire technique for localization of pulmonary nodules during thoracoscopic resection. Chest 1994;105:1467-9. [Crossref] [PubMed]
- Powell TI, Jangra D, Clifton JC, et al. Peripheral lung nodules: fluoroscopically guided video-assisted thoracoscopic resection after computed tomography-guided localization using platinum microcoils. Ann Surg 2004;240:481-8; discussion 488-9. [Crossref] [PubMed]
- Lin MW, Tseng YH, Lee YF, et al. Computed tomography-guided patent blue vital dye localization of pulmonary nodules in uniportal thoracoscopy. J Thorac Cardiovasc Surg 2016;152:535-544.e2. [Crossref] [PubMed]
- Wu TT, Chang YC, Lee JM, et al. Anaphylactic reaction to patent blue V used in preoperative computed tomography-guided dye localization of small lung nodules. J Formos Med Assoc 2016;115:288-9. [Crossref] [PubMed]
- Barthelmes L, Goyal A, Newcombe RG, et al. Adverse reactions to patent blue V dye - The NEW START and ALMANAC experience. Eur J Surg Oncol 2010;36:399-403. [Crossref] [PubMed]
- Bézu C, Coutant C, Salengro A, et al. Anaphylactic response to blue dye during sentinel lymph node biopsy. Surg Oncol 2011;20:e55-9. [Crossref] [PubMed]
- Bellomi M, Veronesi G, Trifirò G, et al. Computed tomography-guided preoperative radiotracer localization of nonpalpable lung nodules. Ann Thorac Surg 2010;90:1759-64. [Crossref] [PubMed]


