Three-field lymph node dissection in treating the esophageal cancer
Introduction
Esophageal cancer is thought to be one of the lethiferous neoplasm with a 5-year overall survival (OS) rate of approximately 50% in some Japanese series (1), whereas in some western countries this value can be lower as 25% (2). Extensive works have been conducted to look for the optimal treatment and to improve the present therapy options, especially for the optimal choice for the dissection of the lymph node. However, there’s still a controversial in the decision of the extent of the lymph node dissection now. Some research has reported that the esophageal cancer correlate with a high rate of nodal and distant metastasis, even at the early stage, and it cannot reach the complete cure without help of the lymph node dissection (3). Furthermore, some Japanese series claimed that extended lymphadenectomy may prevent recurrence and prolong survival after resection of thoracic esophageal carcinoma (4). At the same time, the discussion of the mortality and morbidity as well as the pattern of the lymph node dissection is another debate concerns. The aim of this article is to review the role of the lymph node dissection by introducing the merits and demerits in 3-field lymphadenectomy, and the development in lymphadenectomy’s selection, treatment and diagnosis.
Material and methods
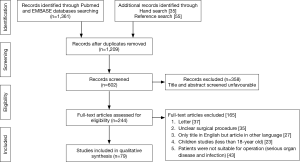
All literatures were searched in the PubMed and EMBASE databases using the terms of Esophageal Neoplasm [Mesh], Lymphatic Metastases [Mesh], Lymph Node Excision [Mesh], Minimally Invasive Surgery, and Robotic-assisted Surgery. Cross references were added and reviewed to complete the reference list. The literatures were examined by reading abstract and full text. The English literatures published from 1961 to 2015 were included. The data in Tables 1-6 were extracted from the related studies, which are comparable, and associated cases were referred and used in this article. And the literatures’ search strategy and study selection are exhibited in Figure 1.
Full table
Full table
Full table
Full table
Full table
Full table
Background
Lymph node metastasis
At present, the need of the extended lymphadenectomy is still under debate, because of several factors, such as the early lymphatic spread and complex distant metastasis of the esophageal cancer. Anatomically, the esophageal can be divided into three parts, which locate in three compartments of the body. And the cancer cells can spread through the lymphatic system longitudinally. So the unique pattern of the lymph node metastasis happened in any lymph node from the neck to the abdomen (28). Several series have showed that the lymph node metastasis were found in the celiac and gastric lymph nodes, nevertheless, these metastasis were originating from the cancer above the tracheal bifurcation, and the lymph nodes at this level thought to drain into the thoracic duct (35). And the upper thoracic esophageal cancer is accompanied with higher rate of pure cervical lymph node metastasis buy the lower rate of locoregional lymph node metastasis when compared to lower thoracic group (28,35,36). With more and more practical experiences and knowledge accumulated in order to improve the treatment of the esophageal cancer since the 19th century. Many surgeons gradually realized the importance of the clearance of the regional lymph nodes in the treatment of the esophageal cancer. After that, Nakayama (37) proposed the clearance of the celiac artery nodes and Logan (5) reported the role of the mediastinal node dissection in the 1960s. In the 1970s, according to the reported frequency of supraclavicular nodes, Sannohe et al. (38) first conducted the lymph node dissection in the bilateral supraclavicular, right intrathoracic and abdominal regions in 36 patients with the thoracic esophageal cancer. In the 1980s, with the development of the surgical techniques, perioperative and postoperative care, many surgeons preferred the extensive lymph node dissection in the treatment of esophageal cancer because of the decreased mortality as well as the improved OS rate. Later in 1994, the types of lymphadenectomy were classified as standard, extended, total, or three-field lymphadenectomy in the Consensus Conference of the International Society for Diseases of the Esophagus (ISDE) (39).
Cervical lymph node metastasis
When referred to the 3-FL, the primary difference between the 2-FL and 3-FL is the clearance of the cervical lymph node, thus recognize the role of the cervical lymph node metastasis correctly make it easier find the benefits 3-FL brings to the patients.
In the last century, the cervical lymph node metastasis was not normally defined, and according to the 9th edition of the Guidelines for clinical and pathologic studies on carcinoma of the esophagus published from Japanese Society for Esophageal Diseases in 1999 (40), the cervical lymph nodes were classified into four groups: 101 (para-esophageal nodes), 102 (deep cervical nodes), 103 (retropharyngeal lymph nodes), 104 (supraclavicular lymph nodes), and each group was divided into left and right sides. However there’s no series reported the prognosis of this classification until Chen et al. (26) reported that there was no significant difference in terms of 5-year survival rates among the 101 alone group, group of 104 alone and the group of 101 and 104 (24.1%, 16.2% and 11.7%, respectively P=0.117). And it elucidated that the different parts of the cervical lymph node metastasis shall be regarded as one common regional lymph node metastasis, which support the AJCC cancer staging manual 7th ed. (41). Furthermore, the AJCC cancer staging manual 7th ed. (41) proposed that the subdivision of “M” stage depend on the presence of the non-regional lymph node involvement should be vanished, which regard cervical lymph node as the regional lymph node. Hsu et al. (42) found there’s no survival difference among patients in N1, M1a and non-regional LNM-related M1b (23.2%, 22.0% 18.5%, respectively, P>0.05), and there’s definite survival difference between patients with and without distant metastasis (P<0.001). Therefore the cervical lymph node metastasis would be better considered as “N” staging instead of “M” staging (24).
The impact of recurrent laryngeal nerve lymph node metastasis
Anatomically, the lymph nodes near the recurrent laryngeal nerve are located at the junction of the neck and chest where the cervical and mediastinal lymph nodes frequently intersected. It is reported that the high risk of metastasis to the lymph nodes near both sides of recurrent laryngeal nerve. Kato et al. (21) found the right recurrent laryngeal nerve lymph nodes was the most frequent site of lymph node metastasis (16.3% in Kato’s series), while Fujita et al. (28) reported the most frequent lymph node recurrence after operation was seen in the lymph nodes near left recurrent laryngeal nerve. Meanwhile, in Ye et al. (43) study, the rate of LN metastasis near the bilateral recurrent laryngeal nerve was 34.2%, in which 15.8% involving the left LNs and 20.8% involving the right LNs. The rate of skip metastasis to the LNs near the recurrent laryngeal nerve was 4.2%. Therefor the dissection alone the both sides of the lymph nodes near the recurrent laryngeal nerve is necessary with regard to its high rate of the lymph node metastasis. Furthermore, Yoshioka et al. (44) reported the rate of cervical lymph node metastasis was 51.6% in patients with lymph node metastasis near the recurrent laryngeal nerve, while the rate was 11.6% in patients without lymph node metastasis near the recurrent laryngeal nerve (P<0.05). At the same time, Ye et al. (43) reported the significant higher rate of 3-year survival in patients with lymph node metastasis near the recurrent laryngeal nerve after radical surgery with 3-FL than patients without recurrent laryngeal nerve lymph node metastasis (29.3% vs. 58.2%, respectively P<0.05). Malassagne et al. (45) showed the similar outcomes with the lower rate of 5-year survival in patients with metastatic recurrent laryngeal nerve lymph node after 3-FL than that of patients with non-LN metastasis (21% vs. 47%, respectively, P<0.05). With too much series, it can be considered that the recurrent laryngeal nerve lymph node is a reliable and strong indicator of cervical lymph node metastasis, and it equally is an important factor affecting the postoperative survival rate of patients with esophageal cancer (43-45). Therefore the recurrent laryngeal nerve lymph node can be regarded as “sentinel node” for cervical lymph node metastasis of esophageal cancer.
Lymph node dissection
Although the 1994’s ISDE conference classified the four types of the lymphadenectomy, the terminologies rarely used in some articles or literatures. At present, the commonly used terms are Ide. classification, which include standard 2-field (2S), extended 2-field (2F) and 3-field resections (3F) (46). Commonly, the region of the lymphadenectomy involve the bilateral lower cervical lymph nodes (including the lymph nodes of the cervical paraesophageal and both sides of supraclavicular), the upper, middle and lower mediastinal lymph nodes (including the lymph nodes of the paraesophageal and the lymph nodes along bilateral recurrent nerves) and the superior abdominal lymph nodes (including the lymph nodes around the cardiac, celiac artery and esophageal hiatus). The 3-FL involves all of these regions, while the extended 2-FL covers all regions except the bilateral cervical lymph nodes. And standard 2-FL is not included the upper mediastinal lymph nodes. In some eastern countries like Japan and China, where the main type of the esophageal cancer is the squamous cell, and it usually locates in the middle and lower esophagus. So the 2-FL, which is referred to the 2F, as a standard surgical treatment has been widely used (14,16,23), and the 3-FL also has been frequently conducted in China in recent years (26,27). However, in some western countries, the adenocarcinoma of the lower esophagus or the esophagogastric junction is common. And the cervical and upper mediastinal lymph node dissection seems distant from where the tumor locates and is rarely conducted. Furthermore, they seldom preform 3-FL because of the not obvious survival rate improving, like Watanabe et al. (47) compared the 5-year survival rate between the 2-FL and 3-FL, the outcomes of which are 54.9% and 47.6% respectively, and there’s no significant difference between two groups, therefore the 2-FL here is referred to the 2S. Occasionally in some western studies, there’s distinguish between 2S and 2F, and D’Journo et al. (48) reported the extended 2-field (2F) improve the 5-year disease-free survival when compared to standard 2-field (2S) (41% versus 10% P<0.05), especially in patients with N0 disease (median survival: 44 versus 17 months, P=0.001), and got almost the same mortality (9% versus 11%, P=0.68) but a bit more non-fatal morbidity, especially the pulmonary complications. Nevertheless the 2F are rarely conducted in western world, because the patients satisfy the needs of 2F are usually submitted to multimodal therapeutic protocols (49), the 2F are not a standard therapy currently.
Although there are too many studies reported the outcomes of the extensive lymph node dissection, there’s still a controversy in how to choose the proper operation to treat different esophageal cancers. Thus it is necessary to review the different types of studies associated with the esophagectomy and lymphadenectomy, collecting the related information on the basis of the modalities of the operation, tumor type, complications, survival, mortality and morbidity in the perioperative and postoperative period, in order to conclude some suggestions for surgeons.
3-FL versus 2-FL
En-bloc esophagectomy (EBE) vs. transhiatal esophagectomy (THE)
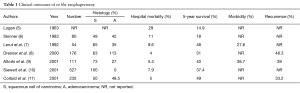
When referred to the esophagectomy we cannot avoid the subject: the EBE, which is frequently performed in most eastern and western countries. From Logan (5) first propagated EBE in 1963 and Skinner (6) broadened the use of EBE in treating thoracic and abdominal esophageal cancer in 1983, more and more studies were conducted to find its benefit in improving the survival (the 5-year survival: from 14.9% to 49% in Table 1) (5-11) and decreasing the mortality (the hospital mortality is ranged from 4–29% in Table 1) (5-11) and recurrence (48.3% to 33.2%) (8,9,11) after the operation. However, several studies from westerns countries also have reported the benefits THE had brought to patients with esophageal adenocarcinoma (6,9), but Hulscher et al. (50) conducted a prospective randomized study comparing EBE with THE for esophageal adenocarcinoma. The 5-year overall and disease-free survival rates (39% and 39%, respectively) after EBE were marginally better than those (27% and 29%, respectively) after THE (P<0.05). Although THE brings the benefits for esophageal adenocarcinoma in lower thorax and esophagogastric junction, the EBE does the same even better effect for patients wherever the tumor locates and whatever the tumor type is. Nevertheless, a more extended esophagectomy also brings the rising morbidity (27.6% and 38.7%) (7,9), and the pulmonary complication is the most common cause of the morbidity and the septic complication is the next (6,7,9).
Clinical outcomes
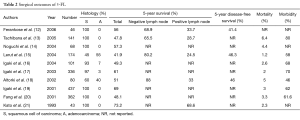
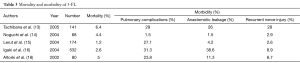
Tachibana et al. (51) has once reviewed the surgical outcomes of extended esophagectomy with 3-field lymph node dissection after 1980 and made the conclusion that the extended esophagectomy with 3-FL would be a safe treatment with low morbidity and acceptable mortality rates. Meanwhile, there’s also some series showed the similar surgical outcomes in Table 2 with the 5-year OS rates range from 41.9% to 73.2% (12-21,51), which is better than the outcome of 2-FL in Table 4 (14,16,22-24). The mortality rates maintained between 1.2% and 10.4%, which is lower than that in 2-FL (14,16,22-25). Akiyama (52) reported the significant survival difference between 2-FL and 3-FL (38.3% versus 55.0% P=0.0013) after R0 resection in 717 patients. Nishihira et al. (4) once conducted a prospective randomized trial, comparing the outcomes after 3-FL and 2-FL, and the hospital death was 3% in 3-FL group and 7% in 2-FL group. The 5-year survival was 66.2% and 48.0%, and the recurrence rate was 19.9% and 24.1%, which drew the conclusion that 3-FL may prevent recurrence and prolong survival after thoracic esophagectomy. However, from Table 3, the morbidity after 3-FL is high, which is ranged from 46–80% (13,15-20), and it is not difficult to find the most frequently happened after 3-FL was pulmonary complications (13-16,18), comparing with the anastomotic leakage and recurrent nerve injury. Fang et al. (20) report with the significant higher respiratory failure (70.6% versus 31.6%, P=0.045) and death rate (47.1% versus 15.8%, P=0.047) in primary postoperative complications group than in secondary complications group after 3-FL, and it accounts for not only the more morbidity but also the more mortality after three-field lymph node dissection in Table 2.
There are two randomized controlled studies demonstrated the better survival benefit of the 3-FL. Nishihira et al. (4) reported a prospective randomized trial of extended and conventional lymphadenectomy, which was referred to 3-FL and 2-FL respectively. The 5-year survival was 66.2% versus 48.0%, and hospital death occurred in 3% and 7%, respectively, which concluded the extended lymphadenectomy is better than the conventional lymphadenectomy. And Kato et al. (53) got the similar results as Nishihira et al. (4) did (the 5-year survival was 48.7% in 3-FL group and 33.7% in 2-FL group, respectively, P<0.01). Although these two studies are randomized trials, there are still some limitations to make these two studies less convinced. The advantages of Nishihira’s studies are the strict criteria of the patients’ selection and the strict randomization they followed, while the number of the patients finally included in this trial was too small, which were 32 cases in extended group and 30 cases in conventional group. Though Kato’s reported finally included the 150 cases, the lack of the strict randomization becomes the drawback of their trail.
Tumor location
When compared with the location of the esophageal cancer, 3-FL is recommended to the cancer with cervical or upper mediastinal lymph node metastasis wherever the cancer locates. It can be demonstrated that the upper mediastinal esophageal cancer has a higher risk of the cervical lymph node metastasis than the middle and lower mediastinal esophageal cancer in Table 5 (26-28). At the same time, Chen et al. (26) reported that the cervical lymph node metastasis was independent of tumor location. Fujita et al. (28) and Kato et al. (21) proposed the most frequently lymphatic recurrence after operation was found in the left upper recurrent nerve nodes and the right supraclavicular, celiac and abdominal paraaortic nodes, in contrast, the right recurrent nerve nodes metastasis was the most frequently found at operation. Meanwhile, Fang et al. (54) explained that the cervical lymph node metastasis is significantly correlated with the upper and/or middle mediastinal esophageal cancer (both P<0.01), while there’s no association with the lower and abdominal esophageal cancer. It seemed that the cervical lymph node dissection is more benefit for patients with the upper and middle thoracic esophageal cancer. At the same time Fujita et al. (55) found the better survival rate in 3-FL with the lymph node metastasis from the upper and middle thoracic esophageal cancer than in 2-FL (1-year survival: 87.3% versus 73.8%; 3-year survival: 50.8% versus 44.6%; 5-year survival: 39.7% versus 35.4%, respectively). Also when take lower thoracic esophageal cancer into consideration, and Igaki et al. (16) recommended the 3-FL in squamous cell carcinoma of lower thoracic esophagus presented with the upper/middle mediastinal lymph node metastasis (5-year survival rate after 2-FL and 3-FL was 5.6% and 30.0%, respectively P=0.005). Meanwhile Shim et al. (22) who compared the upper thoracic esophageal cancer with 2-FL and 3-FL, and found there’s no survival benefit in 3-FL without cervical lymph node metastasis (5-year survival of 3-FL vs. 2-FL: 44% vs. 52% P=0.65, respectively). Therefore when treated with esophageal cancer with cervical and/or upper mediastinal lymph node metastasis, it would be better choose the 3-FL no matter where the cancer locates.
Number of removed lymph nodes
There’s a consensus that the better survival is related to the more harvested lymph nodes. And there are some series in relation to this problem. Peyre et al. (56) analyzed 2,303 esophageal cancer patients (1,381 adenocarcinoma, 922 squamous) from 9 international centers who had accepted R0 esophagectomy, and he concluded that the number of the dissected lymph node was an independent predictor of survival after having esophagectomy, and minimum of 23 regional lymph nodes dissected harvest a better survival. On the basis of the worldwide data, the AJCC cancer staging manual 7th ed. (41) recommends the more lymph nodes resected, the better survival harvested, and the dissected number should follow the increasing pT stage (C 10 for T1; C 20 for T2; and C 30 for T3 and T4). However, Lagergren et al. (57) reported the cohort study of 606 patients who had undergone the esophagectomy revealed that patients in 25–52 lymph nodes dissected didn’t cause a statistically significant decrease in all-cause-5-year mortality compared with the patients in 0–10 lymph nodes dissected (HR: 0.86; 95% CI: 0.63–1.17), whereas the great number of metastatic nodes and the high ratio of positive and negative lymph nodes were related to the improvement of the mortality rates. Equally, van der Schaaf et al. (58) demonstrated the same results by reporting the 1,044 patients who had undergone the esophagectomy. Patients with the 7–15 nodes removed and/or 16–114 nodes removed didn’t decrease the 5-year mortality when compared with the <7 nodes removed (HR: 1.13; 95% CI: 0.95–1.35 and HR: 1.17; 95% CI: 0.94–1.46, respectively), especially in early T stages (Tis–T1) (HR: 1.53; 95% CI: 1.13–2.06). Thus, the view point of the more number of dissected lymph nodes, the better survival harvested will be challenged by the current results, and further research is needed to change clinical practice.
Tumor types in 3-FL
We have mentioned that there’s difference exists in type of esophageal cancer between eastern and western countries. The adenocarcinoma of the esophagus is the main tumor type in western countries. Thus the way of treating the esophageal cancer is contradicted. Series showed in Tables 2,4 have already demonstrated that 3-FL in patients with squamous cell carcinoma of the thoracic esophagus with higher survival and less mortality and morbidity when compared with 2-FL (14,16). Even some western scholars have reported the outcomes of 3-FL as well. Lerut et al. (15) have reported 174 cases of R0 resection with 3-FL, which included 96 adenocarcinoma of lower thoracic esophagus and the esophagogastric junction, the 5-year survival was 41.9% and 5-year disease-free survival was 46.3% and the local recurrence rate was 5.2%. In the meantime, there are also 48 cases of adenocarcinoma of thoracic esophagus included in Altork’s (18) research who reported 29 cases with cervical and thoracic lymph node metastasis and 3 cases with lymph node metastasis to celiac axis, even the 5-year survival in stage III was reached to 54%. Thus, the benefit in survival, lymph node metastasis, mortality and tumor recurrence the 3-FL bring to can be seen in both squamous cell cancer and adenocarcinoma of esophagus.
Patterns of the recurrence
Fang et al. (54) once proposed that although there were various methods in treating the esophageal cancer, the long-term survival was still unsatisfactory with regard to the large quantities of the recurrent diseases developed in patients after radical esophagectomy. Therefore, comparing the patterns of recurrence after 2-FL and 3-FL is another way to adopt the proper lymphadenectomy in treating esophageal cancer. There’s a consensus that the lymph node recurrence is the main part of the recurrence both in patients who had undergone the esophagectomy with 2-FL and 3-FL (59,60). And the lymph node recurrence in the cervical, mediastinal, and abdominal regions are the most essential prognostic factors as many series proposed (8,61,62). Equally, Kato et al. (63) once compared the pattern of recurrence in 50 pT3 patients after esophagectomy with 3-FL and the 100 pT3 patients after 2-FL. The lymphatic recurrence was found less frequently in 3-FL group (34.8%) than in 2-FL group (63.3%) (chi2 =5.1149). It is not difficult to find that the lymph node recurrence is the major pattern of the locoregional recurrence following radical surgery, especially the cervical lymph nodes and the recurrent laryngeal nerve lymph nodes are not dissected routinely in some countries like China (26), and the patients undergone the radical surgery with 3-FL contribute less recurrence rate than 2-FL, and several studies support this idea identically (4,64,65).
Technical improvement in 3-FL
Although the extended lymphadenectomy improve the postoperative survival for patients with thoracic esophageal cancer, the treatment is not suit for every patient. At present, this procedure should be applied for selected patients with good physical conditions in order to relieve the greater surgical stress and to improve the accuracy and specific of lymphadenectomy.
Diagnostic improvement
Several studies reported the 2-FL or 3-FL based on the cervical ultrasonography (US) in patients with esophageal cancer, in order to detect the presence of the cervical lymph node metastasis. Natsugoe et al. (66) showed the sensitivity, specificity, and accuracy of US diagnosis were 74.5%, 94.1%, and 87.6%, respectively in patients who had undergone the radical esophagectomy through right thoracotomy with 3-FL. And Shan et al. (67) compared endobronchial ultrasonography (EBUS) with conventional preoperative endoscopic ultrasonography (EUS) and computerized tomography (CT) examination to evaluate their ability to detect the recurrent laryngeal nerve lymph node metastasis in patients with esophageal cancer. The sensitivities of the preoperative evaluations of recurrent laryngeal nerve lymph node metastasis by EBUS, EUS and CT were 67.6%, 32.4% and 29.4%, respectively. The sensitivity of EBUS was significantly different from that of EUS or CT, especially in the detection of right recurrent lymph node metastasis. Meanwhile he also proposed the combination of the EBUS and EUS will provide more precise information in determining not only the perioperative tumor staging but also the proper lymphadenectomy for the esophageal cancer. There’s another imaging technique used by superparamagnetic iron oxide (SPIO)-enhanced magnetic resonance imaging (MRI) to estimate the need for neck lymphadenectomy in submucosal esophageal cancer, the idea of which was proposed by Motoyama et al. (68). The detection rate was 95%, and there’s no recurrence of the cervical lymph node. The overall recurrence rate was 5%. In the meantime, several studies proposed the “sentinel node” is a good method to improve the accuracy of lymphadenectomy (43-45).
Operational improvement
Saito et al. (69) reported the two stages technique, which means radical esophagectomy with 3-FL is applied for those whose physical condition is well, while if the patients with the poor physical condition, the subtotal esophagectomy with regional lymphadenectomy is performed for them firstly, after approximately one month, the second operation including the esophageal reconstruction with gastric tube and the neck and abdominal lymph node dissection will be conducted. This method not only extended the range of conducting the 3-FL, but also improved the accuracy of 3-FL (68%). At the same time, in order to reduce the surgical stress, Noguchi et al. (14) developed the two-step 3-FL for patients with thoracic esophageal cancer. In the first step operation, the total thoracic esophagectomy through a right thoracotomy with mediastinal and abdominal lymph node dissection is performed. If the recurrent laryngeal nerve lymph node metastasis is pathologically positive, the cervical lymph node dissection is performed 3 weeks after the first step operation. In this method, the specificity is 53%, and though there’s no significant difference in 5-year survival between the second step group and first step group (58% vs. 61%, respectively, P>0.05), 78 of the 146 patients avoided the cervical lymph node dissection without negative therapeutic outcomes.
With the development of the thoracoscopic surgery, many surgeons use the minimally invasive surgery (MIE) techniques in radical esophagectomy with 2-FL or 3-FL (70-72), and it is considered that when compared with the traditional open radical resection, not only dose MIE improve the accuracy of detecting the positive lymph nodes, especially in detecting positive recurrent laryngeal nerve lymph nodes, which resulted in the upstaging of TNM and increased the accuracy of tumor staging [17.11% in Shen et al.’s (70) report and 23.6% in Zhang et al.’s (72) report], but also it brings the lower postoperative morbidity (12–28.6% versus 34–41.2%) (71-74) which is technically safe and feasible for esophageal cancer.
Since Horgan et al. (75) first reported their experience in using robotic-assisted technology to perform a transhiatal total esophagectomy in 2003, many surgeons have taken it into practice. The robotic-assisted technology provides the wider view of operating field with its three-dimensional view, which guarantees the precise and accurate dissection of the tissues near the esophageal, especially the more extensive dissection of the lymph nodes. The mean number of removed lymph nodes ranged from 14 to 43.5 in Table 6 (29-34). At the same time, with the help of robotic-assisted system, a more extensive of lymph node dissection can be easily achieved (34), and the R0 resection was achieved from 94.7% to 97.5% (29,31,33,34). van der Sluis et al. (76) conducted the first randomized controlled trial to compare the robot-assisted minimally invasive thoraco-laparoscopic esophagectomy (RATE) with open transthoracic esophagectomy as surgical treatment for resectable esophageal cancer from January 2012, whose follow-up will be 5 years. Although the trail has not been accomplished yet, the more removed lymph nodes, lower rate of perioperative complications, lower blood loss during the operation, shorter hospital stay and the better prognosis are what we expected from the outcomes of this randomized controlled trial.
Discussion
It is believed that EBE provides more advantages in survival rates of patients with esophageal cancer, especially combined with the 3-field lymphadenectomy, because of the thoroughly tumor resection and lymph node dissection. There’re many studies compared the benefits between the 2-FL and 3-FL, and all these studies proposed were the suggestions of the suitable lymph node dissection in different aspects of the oncological characteristics of the esophageal cancer. Thus, whether choose the 3-FL or 2-FL as the part of the operation of the esophageal cancer, it all depends on the patient’s situation, characters of the tumor and the surgeon’s experiences.
For the benefits in survival rates of different lymphadenectomy, it can be discussed in different parts.
First, as for the location of the esophageal cancer, in early years it suggested that 3-FL brought better survival benefits for the upper and middle thoracic esophageal cancer than 2-FL, especially for the tumor accompanied with the cervical or upper mediastinal lymph node metastasis. In the meantime, the lower thoracic esophageal cancer gets more advantages of survival rates from 2-FL than 3-FL. It is because of the anatomic characters of the lymph node metastasis of the esophageal cancer. Meanwhile, there are cohort studies reported that the cervical lymph node metastasis is more often happened in the upper thoracic esophageal cancer than in the lower thoracic esophageal cancer. Therefore it is less useful in performing the 3-FL in the lower thoracic esophageal cancer and more helpful in treating the upper thoracic esophageal cancer conversely. However the further researches challenged the results of the previous studies. They advocated that if the esophageal cancer accompanied with the upper and/or middle mediastinal lymph node metastasis, it is better to take 3-FL as the paramount consideration, regardless of the location of the esophageal cancer. Equally, when esophageal cancer with no lymph node metastasis, the outcomes of the postoperative survival rates was not significantly different neither in the extent of the lymph node dissection nor in the location of the esophageal cancer, according to the cohort studies showed in this review. So it can be concluded when treated with esophageal cancer with upper and/or middle mediastinal lymph node metastasis, it would be better choose the 3-FL, which can bring the better survival. However, if the patient presented with no metastasis in upper and/or middle mediastinal, either the 3-FL or the 2-FL is recommended.
Second, it is not difficult to find that the lymph node recurrence is the major pattern of the locoregional recurrence following radical surgery, and the patients undergone the radical surgery with 3-FL contribute less recurrence rate than 2-FL (4,64,65). At the same time, the lymph node recurrence in the cervical, mediastinal, and abdominal regions are the important prognostic factors after esophagectomy (8,61,62), especially the lymph node recurrence happened in the cervical regions (18). The Japanese Society for Esophageal Diseases in 1999 (40) once divided the cervical lymph nodes into four groups and a cohort studies demonstrated that there’s no significant difference with the 5-year survival rate in different groups, and there’s also no difference with the survival rate on subdivision of “M” stage according to the appearance of the cervical lymph node metastasis. Thus the cervical lymph node is gradually regarded as “N” rather than “M”, and the results was embodied in AJCC 7th ed. Staging (41). Based on the results of the cervical lymph node metastasis, the impact of the cervical lymph node dissection is reported in a number of studies. Meanwhile, there are some studies reported that the cervical lymph node metastasis is significantly more common in patients with positive recurrent laryngeal nerve lymph nodes rather than negative recurrent laryngeal nerve lymph nodes (45). Moreover, high as the rate of the recurrent laryngeal nerve lymph nodes metastasis was, according to the rate of the right laryngeal nerve lymph node metastasis from 15.8% to 16.3% (21,28), the recurrent laryngeal nerve lymph node dissection was less undergone in some areas. It drew the doctor’s attention, and many studies were concentrated on finding the survival benefits of the recurrent laryngeal nerve lymph node dissection. It’s believed that the dissection of the recurrent laryngeal nerve lymph node would bring a better OS after operation than those without the recurrent laryngeal nerve lymph node dissection. And the patient with positive recurrent laryngeal nerve lymph nodes who has undergone the radical esophagectomy with 3-FL will get more benefits of postoperative survival rate than patients with 2-FL (43-45). At the same time Kato et al. (63) have once reported that the rate of local recurrence in 3-FL group was lower than that in Ivor-Lewis group (17% versus 38%) regardless of whether there’s cervical or upper mediastinal lymph node metastasis or not. The 9% decrease was found in the rate of mediastinal lymph node metastasis after 3-FL and the rate of postoperative cervical lymph node metastasis decreased 10% after 3-FL. Even in patients with esophageal adenocarcinoma, 3-FL also decreased the postoperative recurrence. Altorki (77) found that ten patients happened the recurrence but only one patient happened local recurrence. Thus 3-FL broads the extent of lymph node dissection and plays an important role in decreasing the rate of postoperative recurrence.
Third, there’re also some studies proposed the survival benefits in 3-FL was because of the upstaging of TNM (52,78). The cervical and upper mediastinal lymph node metastasis are usually found during and after 3-FL, which cause upstaging of TNM from stage III to stage IV, even from stage I or II to stage IV. Altorki (77) found the higher 5-year survival rate in patients in stage III after 3-FL than in patients in same stage after 2-FL (54% versus 34%), which were caused by the upstaging of TNM. In 3-FL group, almost of all the patients are truly in stage III because of the thorough lymph node dissection while in 2-FL group, some of the patients in stage III were stage IV actually, which lead a lower 5-year survival. Although Nishihira et al. (4) and Kato et al. (53) have conducted the randomized controlled trail in comparing the survival benefit between 3-FL and 2-FL, the drawbacks of both two trails make the outcome less convinced.
Although the 3-FL brings many benefits for patients with esophageal cancer, the high postoperative morbidity cannot be ignored. The morbidity after 3-FL is high, which is ranged from 46–80% (13,15-20), and it is not difficult to find the most frequently happened after 3-FL was pulmonary complications (13-16,18), comparing with the anastomotic leakage and recurrent nerve injury. The primary difference between 3-FL and 2-FL is the cervical and upper mediastinal lymph node dissection during 3-FL, which makes the higher risk of recurrent laryngeal nerve injury, which will impact the quality of patients’ long-term survival after operation. Therefore surgeons should be familiar with the cervical and upper mediastinal anatomy, and practice the surgical skills consistently, which will lead a lower postoperative morbidity.
The AJCC cancer staging manual 7th ed. (41) recommends resection of as many lymph nodes as possible and that more nodes should be dissected with increasing pT stage (C 10 for T1; C 20 for T2; and C 30 for T3 and T4) based on worldwide data. Many studies proved this result and the patients did get the survival benefits from the more dissection of the lymph node. However, the opposite voice come from several research that the more numbers of the removed lymph nodes brings the same postoperative survival rate as less numbers of the removed lymph nodes does, especially in early T stages (Tis–T1), even the more dissected lymph nodes lead to the worse postoperative survival from the report of the van der Schaaf et al. (58). Therefore, the 3-FL is not feasible for every patient, and the “selected” patients should be taken into consideration. So the way for selecting patients were variously reported, such as the two-step 3-FL, cervical US, EBUS combined with EUS and the SPIO-enhanced MRI, which improved the sensitivity and accuracy of authenticating the appearance of the cervical lymph node metastasis and provided the surgeons optimal operation decisions.
Not only are authentic techniques well-developed but also the operational techniques are largely turned into the area of minimally invasive techniques, including the thoracoscopic esophagectomy and robotic thoracoscopic esophagectomy, which make the lymphadenectomy more feasible, safe and accurate. The research of MIE combined with 3-FL are still in initial stage and it will take an important role in future treatment of esophageal cancer.
Conclusions
Three-field lymphadenectomy is gradually becoming the current way in treating esophageal cancer with cervical and/or upper mediastinal lymph nodes metastasis, and there’s no difference in OS, postoperative morbidity and mortality between 2-field and 3-filed lymphadenectomy regardless of the tumor’s histology and location. Many approaches based on the characteristics of esophageal cancer lymph node metastasis are taken to improve the accuracy of 3-filed lymphadenectomy and decrease the postoperative morbidity and mortality, while each approach needs further studies to demonstrate its feasibility.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Nakagawa S, Kanda T, Kosugi S, et al. Recurrence pattern of squamous cell carcinoma of the thoracic esophagus after extended radical esophagectomy with three-field lymphadenectomy. J Am Coll Surg 2004;198:205-11. [Crossref] [PubMed]
- Daly JM, Fry WA, Little AG, et al. Esophageal cancer: results of an American College of Surgeons Patient Care Evaluation Study. J Am Coll Surg 2000;190:562-72; discussion 572-3. [Crossref] [PubMed]
- Orringer MB, Marshall B, Iannettoni MD. Transhiatal esophagectomy: clinical experience and refinements. Ann Surg 1999;230:392-400; discussion 400-3. [Crossref] [PubMed]
- Nishihira T, Hirayama K, Mori S. A prospective randomized trial of extended cervical and superior mediastinal lymphadenectomy for carcinoma of the thoracic esophagus. Am J Surg 1998;175:47-51. [Crossref] [PubMed]
- Logan A. The surgical treatment of carcinoma of the esophagus and cardia. J Thorac Cardiovasc Surg 1963;46:150-61. [PubMed]
- Skinner DB. En bloc resection for neoplasms of the esophagus and cardia. J Thorac Cardiovasc Surg 1983;85:59-71. [PubMed]
- Lerut T, De Leyn P, Coosemans W, et al. Surgical strategies in esophageal carcinoma with emphasis on radical lymphadenectomy. Ann Surg 1992;216:583-90. [Crossref] [PubMed]
- Dresner SM, Griffin SM. Pattern of recurrence following radical oesophagectomy with two-field lymphadenectomy. Br J Surg 2000;87:1426-33. [Crossref] [PubMed]
- Altorki N, Skinner D. Should en bloc esophagectomy be the standard of care for esophageal carcinoma? Ann Surg 2001;234:581-7. [Crossref] [PubMed]
- Siewert JR, Stein HJ, Feith M, et al. Histologic tumor type is an independent prognostic parameter in esophageal cancer: lessons from more than 1,000 consecutive resections at a single center in the Western world. Ann Surg 2001;234:360-7; discussion 368-9. [Crossref] [PubMed]
- Collard JM, Otte JB, Fiasse R, et al. Skeletonizing en bloc esophagectomy for cancer. Ann Surg 2001;234:25-32. [Crossref] [PubMed]
- Ferahköşe Z, Anadol AZ, Gökbayir H, et al. Three-field lymph node dissection in the treatment of thoracic esophageal carcinoma: the Turkish experience. Dis Esophagus 2006;19:232-7. [Crossref] [PubMed]
- Tachibana M, Kinugasa S, Yoshimura H, et al. Clinical outcomes of extended esophagectomy with three-field lymph node dissection for esophageal squamous cell carcinoma. Am J Surg 2005;189:98-109. [Crossref] [PubMed]
- Noguchi T, Wada S, Takeno S, et al. Two-step three-field lymph node dissection is beneficial for thoracic esophageal carcinoma. Dis Esophagus 2004;17:27-31. [Crossref] [PubMed]
- Lerut T, Nafteux P, Moons J, et al. Three-field lymphadenectomy for carcinoma of the esophagus and gastroesophageal junction in 174 R0 resections: impact on staging, disease-free survival, and outcome: a plea for adaptation of TNM classification in upper-half esophageal carcinoma. Ann Surg 2004;240:962-72; discussion 972-4. [Crossref] [PubMed]
- Igaki H, Tachimori Y, Kato H. Improved survival for patients with upper and/or middle mediastinal lymph node metastasis of squamous cell carcinoma of the lower thoracic esophagus treated with 3-field dissection. Ann Surg 2004;239:483-90. [Crossref] [PubMed]
- Igaki H, Kato H, Tachimori Y, et al. Prognostic evaluation of patients with clinical T1 and T2 squamous cell carcinomas of the thoracic esophagus after 3-field lymph node dissection. Surgery 2003;133:368-74. [Crossref] [PubMed]
- Altorki N, Kent M, Ferrara C, et al. Three-field lymph node dissection for squamous cell and adenocarcinoma of the esophagus. Ann Surg 2002;236:177-83. [Crossref] [PubMed]
- Igaki H, Kato H, Tachimori Y, et al. Prognostic evaluation for squamous cell carcinomas of the lower thoracic esophagus treated with three-field lymph node dissection. Eur J Cardiothorac Surg 2001;19:887-93. [Crossref] [PubMed]
- Fang W, Igaki H, Tachimori Y, et al. Three-field lymph node dissection for esophageal cancer in elderly patients over 70 years of age. Ann Thorac Surg 2001;72:867-71. [Crossref] [PubMed]
- Kato H, Tachimori Y, Mizobuchi S, et al. Cervical, mediastinal, and abdominal lymph node dissection (three-field dissection) for superficial carcinoma of the thoracic esophagus. Cancer 1993;72:2879-82. [Crossref] [PubMed]
- Shim YM, Kim HK, Kim K. Comparison of survival and recurrence pattern between two-field and three-field lymph node dissections for upper thoracic esophageal squamous cell carcinoma. J Thorac Oncol 2010;5:707-12. [Crossref] [PubMed]
- Fujita H, Sueyoshi S, Tanaka T, et al. Optimal lymphadenectomy for squamous cell carcinoma in the thoracic esophagus: comparing the short- and long-term outcome among the four types of lymphadenectomy. World J Surg 2003;27:571-9. [Crossref] [PubMed]
- Kato H. Lymph node dissection for thoracic esophageal carcinoma. Two- and 3-field lymph node dissection. Ann Chir Gynaecol 1995;84:193-9. [PubMed]
- Fujita H, Kakegawa T, Yamana H, et al. Cervico-thoraco-abdominal (3-field) lymph node dissection for carcinoma in the thoracic esophagus. Kurume Med J 1992;39:167-74. [Crossref] [PubMed]
- Chen J, Wu S, Zheng X, et al. Cervical lymph node metastasis classified as regional nodal staging in thoracic esophageal squamous cell carcinoma after radical esophagectomy and three-field lymph node dissection. BMC Surg 2014;14:110. [Crossref] [PubMed]
- Fang WT, Chen WH, Chen Y, et al. Selective three-field lymphadenectomy for thoracic esophageal squamous carcinoma. Dis Esophagus 2007;20:206-11. [Crossref] [PubMed]
- Fujita H, Kakegawa T, Yamana H, et al. Lymph node metastasis and recurrence in patients with a carcinoma of the thoracic esophagus who underwent three-field dissection. World J Surg 1994;18:266-72. [Crossref] [PubMed]
- Galvani CA, Gorodner MV, Moser F, et al. Robotically assisted laparoscopic transhiatal esophagectomy. Surg Endosc 2008;22:188-95. [Crossref] [PubMed]
- Kim DJ, Hyung WJ, Lee CY, et al. Thoracoscopic esophagectomy for esophageal cancer: feasibility and safety of robotic assistance in the prone position. J Thorac Cardiovasc Surg 2010;139:53-59.e1. [Crossref] [PubMed]
- Dunn DH, Johnson EM, Morphew JA, et al. Robot-assisted transhiatal esophagectomy: a 3-year single-center experience. Dis Esophagus 2013;26:159-66. [Crossref] [PubMed]
- Mori K, Yamagata Y, Aikou S, et al. Short-term outcomes of robotic radical esophagectomy for esophageal cancer by a nontransthoracic approach compared with conventional transthoracic surgery. Dis Esophagus 2016;29:429-34. [Crossref] [PubMed]
- Park SY, Kim DJ, Yu WS, et al. Robot-assisted thoracoscopic esophagectomy with extensive mediastinal lymphadenectomy: experience with 114 consecutive patients with intrathoracic esophageal cancer. Dis Esophagus 2016;29:326-32. [Crossref] [PubMed]
- Puntambekar S, Kenawadekar R, Kumar S, et al. Robotic transthoracic esophagectomy. BMC Surg 2015;15:47. [Crossref] [PubMed]
- Saito H, Sato T, Miyazaki M. Extramural lymphatic drainage from the thoracic esophagus based on minute cadaveric dissections: fundamentals for the sentinel node navigation surgery for the thoracic esophageal cancers. Surg Radiol Anat 2007;29:531-42. [Crossref] [PubMed]
- Lee DH, Kim HR, Kim DK, et al. Outcomes of cervical lymph node recurrence in patients with esophageal squamous cell carcinoma after esophagectomy with 2-field lymph node dissection. J Thorac Cardiovasc Surg 2013;146:365-71. [Crossref] [PubMed]
- Nakayama K. Carcinoma of the esophagus and the cardia. Experience in approximately 3,000 cases. J Int Coll Surg 1961;35:143-53. [PubMed]
- Sannohe Y, Hiratsuka R, Doki K. Lymph node metastases in cancer of the thoracic esophagus. Am J Surg 1981;141:216-8. [Crossref] [PubMed]
- Bumm R, Wong J. More of less surgery for esophageal cancer: extent of lymphadenectomy in esophagectomy for squamous cell esophageal carcinoma: how much is necessary? Dis Esoph 1994;7:151-5.
- Japanese Society for Esophageal Diseases. Guide lines for the clinical and pathologic studies for carcinoma of the esophagus. Jpn J Surg 1976;6:79-86. [Crossref] [PubMed]
- Esophagus and esophagogastric junction. In: Edge SB, Byrd DR, Compton CC. editors. AJCC cancer staging manual. 7th ed. New York, NY: Springer, 2009:103-16.
- Hsu WH, Hsu PK, Hsieh CC, et al. The metastatic lymph node number and ratio are independent prognostic factors in esophageal cancer. J Gastrointest Surg 2009;13:1913-20. [Crossref] [PubMed]
- Ye K, Xu JH, Sun YF, et al. Characteristics and clinical significance of lymph node metastases near the recurrent laryngeal nerve from thoracic esophageal carcinoma. Genet Mol Res 2014;13:6411-9. [Crossref] [PubMed]
- Yoshioka S, Fujiwara Y, Sugita Y, et al. Real-time rapid reverse transcriptase-polymerase chain reaction for intraoperative diagnosis of lymph node micrometastasis: clinical application for cervical lymph node dissection in esophageal cancers. Surgery 2002;132:34-40. [Crossref] [PubMed]
- Malassagne B, Tiret E, Duprez D, et al. Prognostic value of thoracic recurrent nerve nodal involvement in esophageal squamous cell carcinoma. J Am Coll Surg 1997;185:244-9. [Crossref] [PubMed]
- Ide H, Eguchi R, Nakamura T, et al. Evaluation of lymph node dissection for thoracic esophageal cancer based on preoperative staging. In: Peracchia A. editor. Recent advances in diseases of the esophagus. Selected papers of the 6th World Congress of the ISDE. Bologna: Monduzzi Editore, 1995:377-83.
- Watanabe H, Kato H, Tachimori Y. Significance of extended systemic lymph node dissection for thoracic esophageal carcinoma in Japan. Recent Results Cancer Res 2000;155:123-33. [Crossref] [PubMed]
- D'Journo XB, Doddoli C, Michelet P, et al. Transthoracic esophagectomy for adenocarcinoma of the oesophagus: standard versus extended two-field mediastinal lymphadenectomy? Eur J Cardiothorac Surg 2005;27:697-704. [Crossref] [PubMed]
- Siewert JR, Stein HJ. Lymph-node dissection in squamous cell esophageal cancer -- who benefits? Langenbecks Arch Surg 1999;384:141-8. [Crossref] [PubMed]
- Hulscher JB, van Sandick JW, de Boer AG, et al. Extended transthoracic resection compared with limited transhiatal resection for adenocarcinoma of the esophagus. N Engl J Med 2002;347:1662-9. [Crossref] [PubMed]
- Tachibana M, Kinugasa S, Yoshimura H, et al. Extended esophagectomy with 3-field lymph node dissection for esophageal cancer. Arch Surg 2003;138:1383-9; discussion 1390. [Crossref] [PubMed]
- Akiyama H, Tsurumaru M, Udagawa H, et al. Radical lymph node dissection for cancer of the thoracic esophagus. Ann Surg 1994;220:364-72; discussion 372-3. [Crossref] [PubMed]
- Kato H, Watanabe H, Tachimori Y, et al. Evaluation of neck lymph node dissection for thoracic esophageal carcinoma. Ann Thorac Surg 1991;51:931-5. [Crossref] [PubMed]
- Fang WT, Chen WH, Chen Y, et al. Selective three-field lymphadenectomy for thoracic esophageal squamous carcinoma. Zhonghua Wei Chang Wai Ke Za Zhi 2006;9:388-91. [PubMed]
- Fujita H, Kakegawa T, Yamana H, et al. Mortality and morbidity rates, postoperative course, quality of life, and prognosis after extended radical lymphadenectomy for esophageal cancer. Comparison of three-field lymphadenectomy with two-field lymphadenectomy. Ann Surg 1995;222:654-62. [Crossref] [PubMed]
- Peyre CG, Hagen JA, DeMeester SR, et al. The number of lymph nodes removed predicts survival in esophageal cancer: an international study on the impact of extent of surgical resection. Ann Surg 2008;248:549-56. [PubMed]
- Lagergren J, Mattsson F, Zylstra J, et al. Extent of Lymphadenectomy and Prognosis After Esophageal Cancer Surgery. JAMA Surg 2016;151:32-9. [Crossref] [PubMed]
- van der Schaaf M, Johar A, Wijnhoven B, et al. Extent of lymph node removal during esophageal cancer surgery and survival. J Natl Cancer Inst 2015.107. [PubMed]
- Natsugoe S, Matsumoto M, Okumura H, et al. Clinical course and outcome after esophagectomy with three-field lymphadenectomy in esophageal cancer. Langenbecks Arch Surg 2010;395:341-6. [Crossref] [PubMed]
- Li CL, Zhang FL, Wang YD, et al. Characteristics of recurrence after radical esophagectomy with two-field lymph node dissection for thoracic esophageal cancer. Oncol Lett 2013;5:355-9. [PubMed]
- Mariette C, Balon JM, Piessen G, et al. Pattern of recurrence following complete resection of esophageal carcinoma and factors predictive of recurrent disease. Cancer 2003;97:1616-23. [Crossref] [PubMed]
- Yano M, Takachi K, Doki Y, et al. Prognosis of patients who develop cervical lymph node recurrence following curative resection for thoracic esophageal cancer. Dis Esophagus 2006;19:73-7. [Crossref] [PubMed]
- Kato H, Tachimori Y, Watanabe H, et al. Recurrent esophageal carcinoma after esophagectomy with three-field lymph node dissection. J Surg Oncol 1996;61:267-72. [Crossref] [PubMed]
- Stiles BM, Mirza F, Port JL, et al. Predictors of cervical and recurrent laryngeal lymph node metastases from esophageal cancer. Ann Thorac Surg 2010;90:1805-11; discussion 1811.
- Jang HJ, Lee HS, Kim MS, et al. Patterns of lymph node metastasis and survival for upper esophageal squamous cell carcinoma. Ann Thorac Surg 2011;92:1091-7. [Crossref] [PubMed]
- Natsugoe S, Yoshinaka H, Shimada M, et al. Assessment of cervical lymph node metastasis in esophageal carcinoma using ultrasonography. Ann Surg 1999;229:62-6. [Crossref] [PubMed]
- Shan HB, Zhang R, Li Y, et al. Application of Endobronchial Ultrasonography for the Preoperative Detecting Recurrent Laryngeal Nerve Lymph Node Metastasis of Esophageal Cancer. PLoS One 2015;10:e0137400. [Crossref] [PubMed]
- Motoyama S, Ishiyama K, Maruyama K, et al. Estimating the need for neck lymphadenectomy in submucosal esophageal cancer using superparamagnetic iron oxide-enhanced magnetic resonance imaging: clinical validation study. World J Surg 2012;36:83-9. [Crossref] [PubMed]
- Saito T, Kuwahara A, Hirao E, et al. Two stages three fields lymph node dissection in esophageal cancer. Nihon Kyobu Geka Gakkai Zasshi 1990;38:1402-9. [PubMed]
- Shen Y, Zhang Y, Tan L, et al. Extensive mediastinal lymphadenectomy during minimally invasive esophagectomy: optimal results from a single center. J Gastrointest Surg 2012;16:715-21. [Crossref] [PubMed]
- Xiao W, Ma K, Peng L, et al. Comparison of thoracoscopic esophagectomy and traditional esophagectomy in radical mediastinal lymphadenectomy for esophageal cancer. Zhonghua Wei Chang Wai Ke Za Zhi 2014;17:911-4. [PubMed]
- Zhang Z, Song Y, Gao Y, et al. Clinical value of thoracoscopic extensive mediastinal lymphadenectomy in the surgical treatment of esophageal carcinoma. Zhonghua Wei Chang Wai Ke Za Zhi 2014;17:902-6. [PubMed]
- Singh RK, Pham TH, Diggs BS, et al. Minimally invasive esophagectomy provides equivalent oncologic outcomes to open esophagectomy for locally advanced (stage II or III) esophageal carcinoma. Arch Surg 2011;146:711-4. [Crossref] [PubMed]
- Biere SS, van Berge Henegouwen MI, Maas KW, et al. Minimally invasive versus open oesophagectomy for patients with oesophageal cancer: a multicentre, open-label, randomised controlled trial. Lancet 2012;379:1887-92. [Crossref] [PubMed]
- Horgan S, Berger RA, Elli EF, et al. Robotic-assisted minimally invasive transhiatal esophagectomy. Am Surg 2003;69:624-6. [PubMed]
- van der Sluis PC, Ruurda JP, van der Horst S, et al. Robot-assisted minimally invasive thoraco-laparoscopic esophagectomy versus open transthoracic esophagectomy for resectable esophageal cancer, a randomized controlled trial (ROBOT trial). Trials 2012;13:230. [Crossref] [PubMed]
- Altorki N. En-bloc esophagectomy--the three-field dissection. Surg Clin North Am 2005;85:611-9. xi. [Crossref] [PubMed]
- Hagen JA, DeMeester SR, Peters JH, et al. Curative resection for esophageal adenocarcinoma: analysis of 100 en bloc esophagectomies. Ann Surg 2001;234:520-30; discussion 530-1. [Crossref] [PubMed]