Non-grasping en bloc mediastinal lymph node dissection through uniportal video-assisted thoracic surgery for lung cancer surgery
Introduction
Since introduced by Gonzalez in 2011 (1), uniportal video-assisted thoracic surgery (VATS) has been demonstrated to be feasible, safe, and effective for lung cancer surgery compared with traditional multi-portal VATS (2,3). Although, diversified techniques have been attempted, complete mediastinal lymph node dissection (MLND) through uniportal VATS is still a difficult work due to more limited access (3-5). It’s not unique that most thoracic surgeons use strategies of grasping, accompanied with which are complicated instrumentation and mutual interference among them, to facilitate exposure and dissection. To simplify the instrumentation and make MLND more comfortable, we designed the method of “non-grasping en bloc MLND” during the practice of tri-portal VATS lung cancer surgery (6). Then we transferred this method into uniportal VATS lung cancer surgery and found it fit well. This paper aims to depict our technical tricks and share our experience.
Surgical technique
Informed consent was obtained from every patient before the operation. The strategies of incision and instrumentation are illustrated in Figure 1A. Anatomic lung resection (lobectomy or segmentectomy) is firstly performed followed by MLND. Except for a ring forceps used for lung traction, only two instruments (suction and energy devices) are needed during MLND. A curved metal endoscopic suction (MES) with side holes on the tip participates in the whole process of MLND. Due to its characteristic of “stick” and capacity of suction, the MES is explored with diversified use, such as manipulation of the target block, blunt dissection, and suction. An electrocoagulation hook (EH) is used for precise excision and hemostasis. An ultrasonic scalpel (US) plays roles as blunt dissector, sealer, and clamper. Efficient coordination of the MES and energy device (EH or US) is effective enough for dissection while maintaining a clear operating field. During dissection we manipulate the nodal block with the noninvasive MES other than grasping the target LNs directly using additional instruments (Figure 1B). Modular dissection is carried out following specific 3-dimensional orders according to different anatomic features of each station. At last, en bloc dissection of each nodal block and skeletonization are achieved (Figure 1C,D).
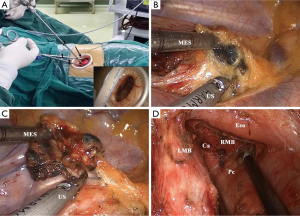
The technical aspects for each station are (Figures 2,3):
- 2R and 4R: dissection of the block is initiated right beneath the arch of azygos vein. The lower part of the block is firstly dissected and flipped over the arch of azygos vein. Then en bloc dissection of the block is performed by coordination of the MES and energy device from caudal to cranial and from anterior to posterior;
- 7R or 7L: the block is firstly dissected off the esophagus until the contralateral main bronchus is identified. Then the block is dissected off the pericardium, the ipsilateral main bronchus, and the carina sequentially. There is no need to retract the esophagus or the aorta using extra instruments even in left subcarinal lymphadenectomy;
- 5 and 6: dissection of stations 5 and 6 is performed anterior to the vagus nerve and posterior to the ascending aorta leaving the phrenic nerve hung free;
- 4L: the block is dissected off the aortic arch, the left main pulmonary artery, and along the left main-stem bronchus (LMB) to the trachea sequentially. The left recurrent laryngeal nerve should be protected from mechanical or thermal injuries.
Between Jan 2014 and Sep 2015, 34 patients with lung cancer underwent successful MLND using this technique, the median number of the dissected mediastinal LNs was 8 (range from 5 to 19). There was seldom cutting of lymph node. There was no severe intraoperative accident and no conversion either to multiportal VATS or thoracotomy. No perioperative morbidity and mortality were identified in this small cohort.
Discussion
The advantage of uniportal VATS lies in the sagittal, caudo-cranial approach, which enables the surgeon a similar angle of view as for open surgery. However, the limited access makes it more difficult to coordinate instrumentation. Surgeons are always trapped by bothersome alternating introduction and removal of diverse instruments. In addition, direct grip of the target LNs may lead to cutting or crushing of them, which may cause bothersome bleeding and potential dissemination of cancer cells if the node is involved. The method of “non-grasping en bloc MLND” incorporates several important features. Firstly, efficient coordination of the MES and energy device (EH or US) makes sure of non-grasping dissection while saving troubles of alternating instrumentation and providing a clear operating field. This technique enables the surgeon to perform MLND with simplest instrumentation. Secondly, the non-grasping strategy meets the oncological principles while avoiding damages to LNs. At last, skeletonization of the anatomic landmarks makes sure of en bloc dissection of each station with no LN missed. As regard to the effectiveness, the median number of the dissected mediastinal LNs was similar to that in triportal VATS (9.5±4.0) (6). There must be some difficulties when dealing with difficult situations such as bulky and invaded nodes using this method. However, this method works well for most kinds of situations. There are some special tricks to deal with invaded lymph nodes. And of course, no one can make sure that there would be no injury to the capsular no matter the nodes are affected or not. Our purpose was to reduce the morbidity as possible other than stop it. This cohort was small, more cases are needed to further validate the effectiveness and advantages of this technique.
In conclusion, the method of “non-grasping en bloc MLND” enables en bloc MLND while saving troubles of excessive interference among instruments and potential damage to the target LN in uniportal VATS for lung cancer surgery. Considering the limited access, this technique truly interprets the concept of “less is more” during uniportal VATS MLND.
Acknowledgements
We thank Ninghui Xu and her nurse staff (Department of Operating Room, West China Hospital, Sichuan University) for their great efforts to participate in the surgical procedures.
Funding: This paper was supported by the Key Science and Technology Program of Sichuan Province, China (No. 2013SZ0005 and No. 2014SZ0148, both to Dr. L Liu).
Footnote
Conflicts of Interest: This paper was presented (poster presentation) at the 24th Annual Meeting of Asian Society for Cardiovascular and Thoracic Surgery (ASCVTS), Taipei, April 4th–10th, 2016.
References
- Gonzalez D, Paradela M, Garcia J, et al. Single-port video-assisted thoracoscopic lobectomy. Interact Cardiovasc Thorac Surg 2011;12:514-5. [Crossref] [PubMed]
- Ng CS, Rocco G, Wong RH, et al. Uniportal and single-incision video-assisted thoracic surgery: the state of the art. Interact Cardiovasc Thorac Surg 2014;19:661-6. [Crossref] [PubMed]
- Wang BY, Liu CY, Hsu PK, et al. Single-incision versus multiple-incision thoracoscopic lobectomy and segmentectomy: a propensity-matched analysis. Ann Surg 2015;261:793-9. [Crossref] [PubMed]
- Jeon HW, Kim YD, Moon YK, et al. Single incision thoracoscopic right upper lobectomy with systematic lymph node dissection. J Cardiothorac Surg 2014;9:66. [Crossref] [PubMed]
- Delgado Roel M, Fieira Costa EM, González-Rivas D, et al. Uniportal video-assisted thoracoscopic lymph node dissection. J Thorac Dis 2014;6:S665-8. [PubMed]
- Liu C, Pu Q, Guo C, et al. Non-grasping en bloc mediastinal lymph node dissection for video-assisted thoracoscopic lung cancer surgery. BMC Surg 2015;15:38. [Crossref] [PubMed]
- Liu C, Ma L, Guo C, et al. Uniportal VATS mediastinal lymphadenectomy (right side). Asvide 2016;3:414. Available online: http://www.asvide.com/articles/1186
- Liu C, Ma L, Guo C, et al. Uniportal VATS mediastinal lymphadenectomy (left side). Asvide 2016;3:415. Available online: http://www.asvide.com/articles/1187


