Psychological impact of revealing a diagnosis of lung cancer to patients in China
Introduction
The right of informed consent refers to that of a patient to make sane decisions regarding the treatment strategy and measures for his disease based on his full understanding of the complete information disclosed to him by his care giver (1). Modern medical ethics deems the patient’s right to know his or her diagnosis and the physician’s reciprocal duty of disclosure as key elements of the informed consent process (2). It is widely accepted in the Western societies that patients with malignant diseases should be fully informed of their diagnosis. While in the Oriental societies, such information is often concealed from the patients. Even in modern China, many healthcare providers and patients’ families still believe in the conventional philosophy that concealing the diagnosis of cancer is beneficial to the patients, at least emotionally. But this is in conflict with the modern notion of the patient’s right of being fully informed of their disease. Patients with lung cancer are more likely to develop various degrees of anxiety and depression due to physical discomfort and psychological factors the disease incurs (3). This prospective study was designed to investigate whether the awareness of diagnosis has a measurable impact on anxiety and depression in patients with surgically resectable lung cancer.
Methods
According to regulations in China, each patient and his/her family members were asked to sign a Letter of Proxy to assign one or more of the trusted members of his/her family to be informed of the conditions of the disease, to make decisions and sign documents on behalf of the patient. Such practice complied with the law and was in consideration of the tradition in China. We used the natural grouping method to divide the patients into two groups according to whether the diagnosis of cancer was disclosed or not. In this method, it was the consigned member of the family who decided which group the patient should be assigned to. Patients were grouped on admission. Patient’s family was fully aware of the diagnosis in our study. The diagnosis of lung cancer was made either before or during surgery. Patients with stage III or IV diseases, older than 80 years, and those who underwent bilateral surgeries were excluded. From February 2013 to March 2013, a total of 70 patients who underwent pulmonary resection for lung cancer in our hospital were collected in the study.
Each patient was asked to fill in a Form of Hospital Anxiety and Depression Scale (HAD Form) before discharge. The HAD Form (4) is composed of 14 items, 7 each for the assessment of anxiety and depression. The results are scored from 0 to 42 which indicate the severity of anxiety or depression. The form can be divided into two equal parts for the evaluation of anxiety and depression. A score between 0 and 7 from each of the semi-form denotes no symptom of anxiety or depression, a score between 8 and 21 denotes symptoms of anxiety or depression (4,5). The Chinese translation of the HAD Form we used in this study had been validated (6,7). The study was approved by the institutional review board at our hospital.
Data were analyzed using SPSS 16.0. Quantitative data were analyzed using Non-parameter Mann-Whitney and Wilcox on test, while patho clinical data, status of anxiety and depression were analyzed using Pearson Chi-square test. Risk factors of anxiety and depression were analyzed using Binary Logistic Regression. P<0.05 was regarded as being significant.
Results
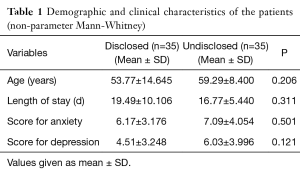
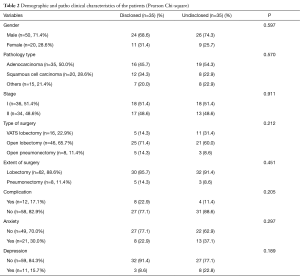
Seventy patients were included in the study, and 50 of them were male. The average age of the patients was 56.5±12.2 years (range, 17 to 76 years). The average length of hospital stay was 18.1±8.2 days (range, 8 to 57 days). Twelve (17.1%) patients had major postoperative complications which included reoperation for bleeding, bronchoscopic aspiration for atelectasis, prolonged air leak and chylothorax. The average anxiety scores were 6.63±3.64 (range, 0 to 18). Other demographic and patho clinical characteristics of the patients were summarized in Tables 1,2.
Full table
Full table
No difference was observed in demographic data between the disclosed and undisclosed groups (P>0.05) (Table 1). The anxiety and depression status and scores between the two groups were not significantly different either (P>0.05) (Table 2).
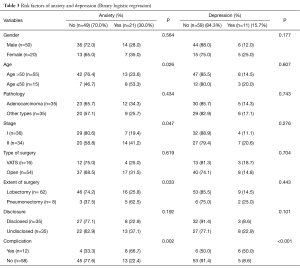
Binary Logistic Regression revealed that age ≤50, relatively more advanced stage, extent of surgery, postoperative complication were risk factors of anxiety (P=0.026, 0.047, 0.033, 0.002), while only postoperative complication was a risk factor of depression (P<0.001). Disclosure was not a risk factor of anxiety or depression (P>0.05) (Table 3).
Full table
Discussion
Modern medicine assumes that every patient has the fundamental right to know the diagnosis, treatment and prognosis of his/her disease (1,2). This is not only an ethical principle, but also a legal right. In the Western world, disclosure of diagnosis to a patient with malignant disease has become normal practice of health care providers. This is by no means an inherent privilege of the patients. In the middle of the 19th century, the American Medical Association (AMA) admonished the doctors not to tell the patient diagnosis of gloomy prognostications, but recommended revealing it to the relatives. The AMA believed that the patient’s spirit could be negatively affected by the health care provider’s words, so that diagnosis of life-threatening diseases should be kept secret from the patient. People at that time believed that “benevolent lies” to conceal cancer diagnosis were meant to protect the patients from emotional upheavals and, therefore, morally justified. In 1953, Fitts and Ravdin performed a questionnaire investigation in the Philadelphia area of the US. on doctor’s willingness to tell the truth to the patients. The results showed that 69% of the doctors usually concealed the diagnosis of cancer from the patient. The two most common reasons for their behavior were unfavorable emotional reaction of the patient and the relative’s request (8). As late as 1961, Oken conducted a study which showed that 90% of the doctors would lie to a patient with cancer, especially when that patient was in his last days (9). Although the doctors chose not to disclose the diagnosis of cancer, most patients would prefer to know (10). Within 20 years, the US. saw a complete reversal in the attitude toward truth-telling. In 1979, Novack and Oken used the same questionnaire they used in 1961 to investigate doctors’ opinion about disclosure of cancer diagnosis and came up with a reverse result. Ninety-seven percent of the doctors were willing to disclose a diagnosis of cancer to the patient (11). Now, few doctors doubt the policy of truth-telling to cancer patients in the US.
In spite of the triumph of doctor’s honesty and patient’s autonomy over medical paternalism in North America, Northern and Western Europe, people in Asia and some part of Europe still hold the old belief that “benevolent lies” are better than cruel facts to patients with end-stage diseases. Thomsen studied the variation in attitudes among European physicians toward truth telling in case of cancer. Unlike their colleagues in Northern Europe, physicians in Southern and Eastern Europe are more likely to reveal the diagnosis of cancer to the patient’s spouse rather than the patient (12). This discrepancy in belief of truth telling reflects not only the difference of doctor’s creed but also that of the population’s expectation between the Western and Eastern World. It’s deeply rooted in the Asian culture that benignly intended deception is meant for the patient’s interest and therefore morally justified. Montazeri and colleagues studied quality of life in patients with cancer in an Iranian population and found that those who did not know the diagnosis had a better physical, social and emotional quality of life than those who knew the diagnosis. They doubted the rationality of truth telling to cancer patient in the Asian World. They hypothesized that the principle of cancer disclosure might vary due to cultural differences (13). Similarly, studies conducted in India and Turkey showed that patients that received a cancer diagnosis had a significantly higher psychiatric morbidity than those left unaware of their diagnosis (14,15).
In fact, the East is not a monolithic block. In some parts of the Estern World, the notion that disclosure of diagnosis is detrimental to patients with cancer is changing. This is partly the result of education in the medical school (16). In Qatar, Rodriguez used Oken’s questionnaire to investigate a sample of 131 physicians, and found that nearly 90% of them claimed that they would inform patients of their cancer diagnosis (2). Another study from Turkey contradicted the excuse of cultural difference by not finding any difference in quality of life between patients who had their diagnosis of cancer revealed to themselves or not (17).
Our study did not find any relationship between disclosure of lung cancer diagnosis and patient’s depression or anxiety. We believe that there were two factors contributing to our results which were discordant from some studies carried out in Asia. Firstly, health care providers are no longer the only source of information for patients. When a patient develops symptoms related to cancer, he/she will search online for possible diagnosis. Furthermore, when a patient has access to his/her report of imaging examination, the diagnosis is often self-evident. So, even if the doctors would withhold the truth, the patient could see through their “white lies”. The patient and the doctor can sometimes reach a tacit agreement not to expose the lies. The patient feels that the doctor is concealing the diagnosis, but neither side would point it out. Secondly, as the medical conditions improve in China, more and more patients with lung cancer are diagnosed in early stage with a much better prognosis, patients are less likely to experience severe depression and anxiety and the doctors more willing to tell the truth.
Rises in the level of education and income are accompanied by aspirations for autonomy (18). In modern China, the patient’s desire to know the truth is stronger than ever. On the other hand, the instillation of ideas of modern medical science in medical school and frequent international communications have been changing notions of young medical staff. Although the traditional Chinese cultures prefer paternity in medical service, the new generation of doctors and nurses are more likely to consider truth telling a natural behavior.
The patient’s ability to cope with the disease is reinforced by the knowledge of their diagnosis and prognosis. Being diagnosed with cancer has been found to be a motivation for lifestyle changes, which include dietary changes, physical activities and smoking cessation. Therefore, patients with cancer can benefit from disclosure of diagnosis. Kostopoulou and colleagues conducted a study which showed that cancer patients who knew their diagnosis were 2.5 times as likely to change their eating habits as those who didn’t know their diagnosis, and newly diagnosed patients were more inclined to stop or reduce smoking (19). Furthermore, medical workers’ honesty toward patients helps to establish mutual trust and better communication between both sides, which will promote patients’ compliance to doctors’ instructions (20). Lack of knowledge of their diseases could be a major obstacle for the patients to manage their health problems.
The limitations of this study should be noted. This was not a randomized controlled study. All the subjects included in this study were those who were willing to authorize their family member to decide whether truth should be told to themselves. These subjects were different from those who would insist on being told the truth in the first place. Secondly, level of education and economic status of the subjects were not clear. Patients with a more advanced level of education might be more capable of communication with their health providers and therefore more likely to insist on hearing the truth. Economic status was another concern. Patients of poorer economic status were more sensitive to the effectiveness of the treatment, and more likely to give up treatment when they felt that their disease was incurable. Finally, all the subjects in this study were diagnosed with stage I and II lung cancers. These patients might have a brighter view of the prognosis of their disease. Their emotional status might differ from those with end-stage diseases. All the above-mentioned factors would have a bearing on patient’s willingness to participate in this study. Nevertheless, such biases in patient selection was unavoidable, as long as the principle of informed consent was complied with.
Conclusions
To conclude, the right to learn the truth of diagnosis and prognosis is a fundamental right of patients. It is not only wrong but also unnecessary to conceal cancer diagnosis to patients who are willing to know the truth. Patients in the Orient, like their equivalent in the West, can competently cope with the bad news. Telling the truth will not increase the incidence of depression or anxiety. It maybe the time to gradually abandon the old belief of protecting patients with cancers by concealing truth from and making decisions for them in this old country. Change can be made beginning with patients with early-stage cancers.
Acknowledgements
We would like to thank Kristin Eckland, ACNP-BC, MSN, RN, for her assistance in language correction.
Funding: This research was supported by “Shanghai young nursing talent training program”, No. QNHL2016; “Shanghai Health and Family Planning Commission Program”, No. 2014LP036A.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethics Statement: The study was approved by institutional ethics board of Shanghai Pulmonary Hospital (No. K16-282) and written informed consent was obtained from all patients.
References
- Hadfield P. Informed consent. Lancet 1993;341:1141. [Crossref] [PubMed]
- Rodriguez Del Pozo P, Fins JJ, Helmy I, et al. Truth-telling and cancer diagnoses: physician attitudes and practices in Qatar. Oncologist 2012;17:1469-74. [Crossref] [PubMed]
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361-70. [Crossref] [PubMed]
- Hopwood P, Stephens RJ. Depression in patients with lung cancer: prevalence and risk factors derived from quality-of-life data. J Clin Oncol 2000;18:893-903. [PubMed]
- Bjelland I, Dahl AA, Haug TT, et al. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res 2002;52:69-77. [Crossref] [PubMed]
- Zhang J, Wei J, Shi LL, et al. A multiple center study on depression and anxiety state in the department of neurology. Zhonghua Yi Xue Za Zhi 2007;87:889-93. [PubMed]
- Li S, Yang X, Huang P, et al. Correlation among cognitive function and activities of daily living, anxiety and depression in hospitalized older patients. J Nursing Science 2013;28:68-70.
- Fitts WT Jr, Ravdin IS. What Philadelphia physicians tell patients with cancer. J Am Med Assoc 1953;153:901-4. [Crossref] [PubMed]
- Oken D. What to tell cancer patients. A study of medical attitudes. JAMA 1961;175:1120-8. [Crossref] [PubMed]
- Kelly WD, Friesen SR. Do cancer patients want to be told? Surgery 1950;27:822-6. [PubMed]
- Novack DH, Plumer R, Smith RL, et al. Changes in physicians' attitudes toward telling the cancer patient. JAMA 1979;241:897-900. [Crossref] [PubMed]
- Thomsen OO, Wulff HR, Martin A, et al. What do gastroenterologists in Europe tell cancer patients? Lancet 1993;341:473-6. [Crossref] [PubMed]
- Montazeri A, Tavoli A, Mohagheghi MA, et al. Disclosure of cancer diagnosis and quality of life in cancer patients: should it be the same everywhere? BMC Cancer 2009;9:39. [Crossref] [PubMed]
- Alexander PJ, Dinesh N, Vidyasagar MS. Psychiatric morbidity among cancer patients and its relationship with awareness of illness and expectations about treatment outcome. Acta Oncol 1993;32:623-6. [Crossref] [PubMed]
- Atesci FC, Baltalarli B, Oguzhanoglu NK, et al. Psychiatric morbidity among cancer patients and awareness of illness. Support Care Cancer 2004;12:161-7. [Crossref] [PubMed]
- Hamadeh GN, Adib SM. Changes in attitudes regarding cancer disclosure among medical students at the American University of Beirut. J Med Ethics 2001;27:354. [Crossref] [PubMed]
- Bozcuk H, Erdoğan V, Eken C, et al. Does awareness of diagnosis make any difference to quality of life? Determinants of emotional functioning in a group of cancer patients in Turkey. Support Care Cancer 2002;10:51-7. [Crossref] [PubMed]
- Oksüzoğlu B, Abali H, Bakar M, et al. Disclosure of cancer diagnosis to patients and their relatives in Turkey: views of accompanying persons and influential factors in reaching those views. Tumori 2006;92:62-6. [PubMed]
- Kostopoulou V, Katsouyanni K. The truth-telling issue and changes in lifestyle in patients with cancer. J Med Ethics 2006;32:693-7. [Crossref] [PubMed]
- Dalla-Vorgia P, Katsouyanni K, Garanis TN, et al. Attitudes of a Mediterranean population to the truth-telling issue. J Med Ethics 1992;18:67-74. [Crossref] [PubMed]


