Endovascular stent graft repair of the ascending aorta—final frontier in the endovascular treatment of the aorta
Endovascular aortic/aneurysm repair (EVAR) of the abdominal aorta was performed first, and it was followed by thoracic endovascular aortic/aneurysm repair (TEVAR) for true aneurysm. Aortic arch aneurysms later came to be treated by TEVAR with various debranching techniques. The indications for TEVAR have recently been extended to the treatment of a majority of symptomatic type B aortic dissections with rupture or malperfusion. The indication for uncomplicated type B aortic dissections is controversy; however, large entry size, partially thrombosed false lumen, and larger aortic diameter in acute phase are regarded as risk factors for worse outcome (1-3). Therefore, TEVAR has been proposed as a means to prevent late complications by covering the primary entry tear and obtain the thrombosed remodeled false lumen. Although ascending TEVAR is currently limited to high surgical risk patients with aortic pathologies originating above the sinotubular junction and there is no consensus in regard to a standardized technique, the aortic root and ascending aorta are now the final frontiers for treatment by TEVAR.
Piffaretti et al. described eight patients with ascending aortic pseudoaneurysms and penetrating aortic ulcers of the ascending aorta who underwent total endovascular repair of the ascending aorta (4). Despite the fact that six of the cases were urgent interventions, primary clinical success was achieved in seven (87.5%) of the eight cases, and all patients were discharged home and independent after a median length of stay of 6 days (range, 5–24 days) without primary conversion, cerebrovascular accidents, valve impairment, or myocardial infarction. A low-flow type 3 endoleak in one patient remained asymptomatic and was managed conservatively. Because there was a significant reduction in diameter (≥5 mm) in 7 aortic lesions (87.5%) at the 1-year follow-up period, Piffaretti et al. concluded that ascending TEVAR was a feasible, safe, and effective means of treating ascending aortic pseudoaneurysms and penetrating aortic ulcers, and in a very selected subset of lesions favorable midterm results were obtained with both standard and custom-designed endografts.
Roselli et al. performed supracoronary ascending TEVAR in 22 patients with an acute type A dissection, intramural hematoma, pseudoaneurysm, chronic dissection, or aorto-cardiac fistula (5). The devices were delivered via a transfemoral, transapical, or axillary artery approach, and the proximal landing zone was at the sinotubular junction, mid- to distal ascending aorta, or graft from a previous ascending repair. There were three hospital deaths, including the death of a patient with partial occlusion of the left coronary artery that required open conversion, and there were three strokes and two myocardial infarctions. During a median follow-up period of 12 months, six patients developed a type 1 endoleak: two were treated endovascularly, one was treated by open repair, in one patient the endoleak resolved, one refused treatment, and one is being observed. In two of the patients, TEVAR was performed as a rescue, bridge treatment that was followed by open repair because of ruptured high-risk dissection. Actual survival at 30 days, 1 year, and 5 years was 86%, 80%, and 75% respectively. Roselli et al. concluded that ascending TEVAR is a feasible alternative to medical therapy for repair of acute and chronic ascending disease in high-risk patients.
Muetterties et al. reviewed a total of 52 articles published in the literature that focused on isolated ascending TEVAR. Sixteen different aortic stent grafts were used in 138 total patients (6). The most frequently treated aortic pathology was type A aortic dissection (80 cases), and it was followed by aortic pseudoaneurysms (38 cases), penetrating atherosclerotic ulcers (5 cases), intramural hematomas (4 cases), and ascending aortic aneurysms (4 cases). Femoral arterial access was used in 94 (68.1%) patients, and a transapical approach was used in 15 patients (10.9%), a carotid approach in 13 patients (9.4%), and axillary approach in 8 patients (5.8%). The type I endoleak was observed in 15 patients (10.9%), and 10 patients (7.2%) required open or endovascular repair. There were 3 (2.2%) open conversions and 3 (2.2%) cerebrovascular complications. All-cause mortality was 12 (8.7%). Aortic-related mortality was 2 (1.5%); the 30-day mortality was 9 (6.5%). The average follow-up period was 19.1 months. Muetterties et al. concluded that despite the absence of an approved ascending TEVAR technique, patients with a range of ascending aortic pathologies are currently being successfully treated by means of endovascular technologies, and aortic-related mortality in high-risk patients was comparable to aortic-related mortality in open surgery.
Ascending TEVAR is more challenging than TEVAR of the descending thoracic aorta or aortic arch because of the more complex pathology, hemodynamics, and anatomy. Although morbidity is significant, ascending TEVAR can be a lifesaving treatment in selected high-risk patients.
To obtain better and more reliable outcomes of ascending TEVAR, a better understanding of the pathology of ascending aortic dissection/aneurysms, and improvement of delivery systems and graft materials will be important.
Infection of the ascending aortic aneurysm
Piffaretti et al. used ascending TEVAR to treat one mycotic case of pseudoaneurysm (4). Diagnosing aortic infections is sometimes difficult, and aortic infection must be differentiated from penetrating atherosclerotic ulcer. Aortic infection and aortic graft infection are usually diagnosed on the basis of collaborate evidences such as blood cultures, the leukocyte count, serum C-reactive protein level, and clinical findings taken together. When the patient has already been treated with an antibiotic, the blood culture tends to be negative. Fluorodeoxyglucose-positron emission tomography/computed tomography (FDG-PET/CT) is helpful to diagnose infection. Once a diagnosis of infection is made, a synthetic graft is considered contraindicated. Open surgery using biomaterial or rifampicin-soaked synthetic graft replacement with or without omentopexy is usually recommended (7-9).
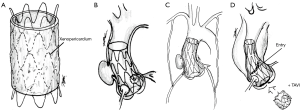
In the future, TEVAR using antibiotic drug eluting stent graft or stent graft made of biomaterial e.g., xenopericardium might be a choice to treat the infected aorta (Figure 1A).
Challenges in the future
Occasionally the entry in type A aortic dissection is close to the aortic root or at sinus of Valsalva sinus, and it frequently exists in combination with a preexisting ascending aneurysm and aortic valve insufficiency. In the future, it may be possible to treat root-ascending pathology by newly developed methods and devices e.g., root-ascending TEVAR with coronary ostia fenestrated stent graft (Figure 1B), root-ascending TEVAR with non-fenestrated stent graft in combination with off-pump coronary artery bypass graft using both internal thoracic arteries (Figure 1C). When aortic valve insufficiency co-exists, root-ascending TEVAR in combination with transcatheter aortic valve implantation (TAVI) might be considerable (Figure 1D).
When it is difficult to obtain an adequate distal landing zone due to the anatomy, brachiocephalic artery occlusion with axillo-axillary bypass may be a solution to prevent endoleak (Figure 2).

Undoubtedly, improvements to devices and techniques will enable more reliable, more proximal TEVAR.
Acknowledgements
None.
Footnote
Provenance: This is an invited Commentary commissioned by the Section Editor Lei Zhang (Department of Vascular Surgery, Changhai Hospital, Second Military Medical University, Shanghai, China).
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Marui A, Mochizuki T, Mitsui N, et al. Toward the best treatment for uncomplicated patients with type B acute aortic dissection: A consideration for sound surgical indication. Circulation 1999;100:II275-80. [Crossref] [PubMed]
- Evangelista A, Galuppo V, Gruosso D, et al. Role of entry tear size in type B aortic dissection. Ann Cardiothorac Surg 2014;3:403-5. [PubMed]
- Brunkwall J, Kasprzak P, Verhoeven E, et al. Endovascular repair of acute uncomplicated aortic type B dissection promotes aortic remodelling: 1 year results of the ADSORB trial. Eur J Vasc Endovasc Surg 2014;48:285-91. [Crossref] [PubMed]
- Piffaretti G, Galli M, Lomazzi C, et al. Endograft repair for pseudoaneurysms and penetrating ulcers of the ascending aorta. J Thorac Cardiovasc Surg 2016;151:1606-14. [Crossref] [PubMed]
- Roselli EE, Idrees J, Greenberg RK, et al. Endovascular stent grafting for ascending aorta repair in high-risk patients. J Thorac Cardiovasc Surg 2015;149:144-51. [Crossref] [PubMed]
- Muetterties C, Menon R, Wheatley G. Ascending TEVAR: A Systematic Review of Isolated Endovascular Repair of the Ascending Aorta. J Vasc Surg 2016;63 supple:152S-153S. [Crossref]
- Kubota H, Endo H, Noma M, et al. Xenopericardial roll graft replacement for infectious pseudoaneurysms and graft infections of the aorta. J Cardiothorac Surg 2015;10:133. [Crossref] [PubMed]
- Kubota H, Endo H, Noma M, et al. Equine pericardial roll graft replacement of infected pseudoaneurysm of the ascending aorta. J Cardiothorac Surg 2012;7:54. [Crossref] [PubMed]
- Kubota H, Endo H, Noma M, et al. Equine pericardial roll graft replacement of infected pseudoaneurysm of the aortic arch. J Cardiothorac Surg 2012;7:45. [Crossref] [PubMed]


