The APPS: an outcome score for the acute respiratory distress syndrome
Introduction
The acute respiratory distress syndrome (ARDS) is an acute and intense inflammatory process of the lungs that develops in response to pulmonary and systemic insults to the alveolar-capillary membrane, resulting in increased vascular permeability and development of interstitial and alveolar edema. Although ARDS is clinically characterized by acute hypoxemic respiratory failure refractory to oxygen therapy, over the years we have used several different diagnostic schemas, all based on a combination of clinical, oxygenation, radiographic, and hemodynamic abnormalities to identify these patients (1,2).
There is no typical ARDS patient. ARDS is a complex heterogeneous disease process that is not associated with or caused by any single etiology. This heterogeneity has made therapy challenging. ARDS cannot be diagnosed or described by any single laboratory test, treatment remains supportive, and we lack mechanistically or disease-specific pharmacotherapies to improve outcome.
It is estimated that about one million patients around the world develop ARDS each year; more than one third of them will not survive the syndrome (3). It has been demonstrated that lung injury severity 24 hours after ARDS onset is a major determinant of outcome (4). However, no simple and reliable index quantifying the clinical condition of ARDS patients predicts hospital outcome at 24 hours of usual care (including lung protective ventilation and hemodynamic stabilization) until the recent description and validation of an ARDS score by Villar et al. (5). Current definitions of ARDS are incapable of properly identifying or stratifying ARDS patients in terms of severity and prognosis (4). It is increasingly recognized that our understanding of the definition of ARDS and its outcome has been limited by the failure to accept that ARDS is a syndrome with different phenotypes that are independent of each other (1,4).
The need for an ARDS scoring system
The introduction of scoring systems such as the APACHE II score (6) or the injury severity score (7) in critically ill patients have illustrated the value of scoring systems that predict patient outcome. Unfortunately, those models can only be applied to general intensive care unit populations because they do not provide consistent and accurate estimates of the risk of death in patient populations with a specific disease process. A number of groups have attempted to characterize predictors of death in ARDS by developing a prognostic index (8,9), but their predictive power remains controversial, they are not easily calculated, and have not been replicated or validated. An arbitrary lung injury severity score was proposed in 1988 as an expanded definition of ARDS by taking into account four features of the syndrome: chest radiograph infiltration, PaO2/FiO2 ratio, applied positive end-expiratory pressure, and lung compliance (10). However, in our opinion, such scoring systems should be abandoned for three major reasons. First, they are not specific for ARDS: patients with a major component of cardiogenic pulmonary edema may be mislabeled as having ARDS, and a postoperative patient with moderate atelectasis and mild fluid overload may fit the lung injury score for ARDS. Second, they have not been validated: it is not clear whether patients with identical lung injury severity score have similar degrees of lung injury. Third, it has been shown in large cohorts that mean lung injury scores are not significantly different between ARDS survivors and non-survivors (4).
In 1953, Apgar introduced a 10-point scoring system for evaluation of newborn infants that transformed obstetrical care forever (11). The Apgar score is known universally, allowing clinicians to quickly rate the condition of newborns on five simple criteria (skin color or appearance, pulse rate, reflex irritability or grimace, activity or muscle tone, respiration) on a scale from 0 to 2, and then summing up the five values obtained. The score turned an intangible and impressionistic clinical evaluation into a number defining the patient’s status that is comparable across patients and populations. The Apgar score proved simple to use, effective at providing clinicians with graded feedback on a newborn’s condition, and predictive of hospital survival. It quickly became clear that a neonate with a bad Apgar score required resuscitation. As a result, neonatal intensive care units sprang into existence and the quality of care provided to neonates improved dramatically.
APPS: an Apgar score for ARDS
Regardless of how we view medicine as an art or as a science, every critically ill patient we treat deserves an Apgar-type score! Similar to obstetrics in 1953, most conditions requiring intensive care are without a routine and reliable gauge of overall patient status to guide clinical practice and predict outcome. Gawande et al. (12) recently reported that a simple surgical Apgar-type score based on three variables (the amount of blood loss, the lowest heart rate, and the lowest blood pressure that a patient experiences during an operation) could be used to rate patients condition and predict their outcome after general or vascular surgery. They described their model in 303 patients undergoing colectomy and validated the score in two independent cohorts of 102 and 767 surgical patients. Further reports by independent groups have confirmed the validity and generalization of this surgical Apgar-type score (13).
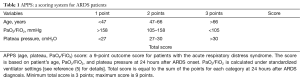
Villar et al. (5) deviated from prior studies in ARDS (14) by developing and validating a simple 9-point score in 600 patients with moderate and severe ARDS. This score, referred to as APPS, is based on the tertile distribution of individual values of patient’s age, PaO2/FiO2 ratio, and plateau pressure measured 24 h after ARDS diagnosis (Table 1). Tertiles allow expression of clinical values in ordinal range categories, akin to how clinicians routinely categorize patients into risk groups as highlighted by Santos et al. (15) and Repessé et al. (16) when discussing the value of the APPS in this issue of the journal. Tertile categorization detected useful information about the overall population that was not as evident when evaluating mean values of those variables. In general, outcome is worse with increasing age (17), patients with more severe lung injury tend to have lower PaO2/FiO2 (4), and there is a direct relationship between plateau pressure and mortality (18).
Full table
William Osler said that medicine is a science of uncertainty and an art of probability (19). Therefore, most of the time we are not dealing with facts, we are dealing with statistical probabilities. Although none of the prognostic models clinically in use today will ever precisely predict patient outcomes with 100% certainty, we believe that the APPS is more useful for decision making than any of the current ARDS scores for several reasons. First, clinicians can use the APPS to inform their own bedside predictions of a patient’s risk of death. The combination of model-based and physician-based estimates of mortality outperform either in isolation (20). Second, clinical trials with ARDS patients may utilize this score to stratify patients into each study arm to ensure that patients with similar risk of death are balanced between treatment and control groups. The APPS model is in line with recent recommendations stating that a better identification of patient populations is the key for appropriate characterization of patient status (21). Clearly, the APPS illustrates that ARDS cannot be viewed as a homogeneous disorder. On the contrary, when scoring patients after 24 hours of usual intensive care, we found that patients could be grouped more uniformly into three categories of increasing overall fatal outcome that were associated with increasing lung dysfunction. Third, since the APPS captures the severity of the disease process very early (immediately after 24 hours of standard intensive care), it could be used as a modifier of treatment effect in therapeutic clinical trials thought to have greater impact among sicker patients (22). If APPS is used as a modifier of treatment effect, it seems obvious that patients with a low risk of death are not going to benefit from the application of very aggressive therapies that may have a marked impact on sicker patients. By contrast, ARDS patients in the highest risk group (APPS >7 points) should be considered as a medical emergency. Forth, as it occurs with other accepted clinical scores, we can use the APPS in all observational, clinical and translational studies to better adjust for severity of illness when analyzing the association of confounding variables with mortality.
Our APPS model showed an excellence performance in a large cohort of consecutive patients with moderate and severe ARDS ventilated with a lung protective mechanical ventilation strategy. In addition to the simplicity of the calculation of the APPS, the stratification of ARDS patients based on their total score is linked to two measures of severity: one that specifically quantifies the severity of ARDS and another that quantifies the overall physiologic response along with patient’s age. We do not know whether the treatment-dependent variables (PaO2/FiO2 and plateau pressure) will influence the performance of the APPS under different practice patterns and circumstances, such as using: (I) non-protective mechanical ventilation; (II) a non-standardized ventilatory approach for measuring PaO2/FiO2; (III) novel pharmacologic therapies; (IV) different outcome end-points; (V) scoring at the time of ARDS diagnosis; or (VI) applying the score to mild ARDS. We believe that the APPS will provide the scientific basis to focus research on a more homogeneous set of ARDS patients.
It is also plausible that additional variables that influence the pathogenesis of ARDS and can increase APPS prediction power might be identified and added or substituted in a modified APPS. As commented by Santos et al. (15), the driving pressure (calculated as the difference between plateau pressure and positive end-expiratory pressure) has been suggested to be a better determinant of ARDS outcome than plateau pressure (23). However, that finding should be considered hypothesis-generating rather than definitive. Currently, there are no data that link a particular PaO2/FiO2 to predictable structural changes in the alveolar-capillary membrane, to the development of permeability edema, or to the amount of edema that accumulates as a result of increased vascular permeability (24). In this context, a measure or a biomarker of vascular permeability could be useful in the future to track the natural history of the diffuse alveolar damage that defines ARDS, although increased vascular permeability is itself a nonspecific marker of inflammatory damage to the alveolar-capillary membrane.
As pointed out by Repessé et al. (16), the current conceptual model of ARDS focuses almost entirely on lung mechanics and gas exchange, and excludes pulmonary hemodynamics. Paradoxically, the severity of lung injury during ARDS is related to the level of elevation of the pulmonary artery pressure (25). Pulmonary hypertension and right ventricular dysfunction are uniform features in all cases of moderate and severe ARDS of many etiologies, despite a normal cardiac output and the absence of systemic hypoxemia (25). Therefore, it is plausible that the degree of pulmonary hypertension or right ventricular afterload could be an additional variable for quantifying hemodynamic perturbations in ARDS, if it is shown that their addition to APPS improves the prediction power of APPS.
Conclusions
The current ARDS definition and the complex pathogenesis of ARDS will continue to complicate the task of identifying subgroups of ARDS patients who are at risk for poor outcome and who have the potential to benefit from approaches that target specific physiologic, biologic or genetic pathways. The use of APPS to guide risk stratification of patients with ARDS can be expected to be an important tool for guiding therapy, and for increasing the potential of success of future clinical trials. We do not exclude that in the future, incorporating markers of increased pulmonary vascular permeability and right ventricular dysfunction could improve the prognostic accuracy of the APPS.
Acknowledgements
This paper is dedicated to the memory of Dr. Alan Gilston [1928–2005] and Dr. Simon Bursztein [1934–1995], two of the pioneers of intensive and critical care medicine.
Funding: This work is supported in part by Instituto de Salud Carlos III, Spain (CB06/06/1088, PI13/0119), and Asociación Científica Pulmón y Ventilación Mecánica.
Footnote
Provenance: This is an invited Editorial commissioned by the Section Editor Zhongheng Zhang (Department of Critical Care Medicine, Jinhua Municipal Central Hospital, Jinhua Hospital of Zhejiang University, Jinhua, China).
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Villar J, Blanco J, Kacmarek RM. Acute respiratory distress syndrome definition: do we need a change? Curr Opin Crit Care 2011;17:13-7. [Crossref] [PubMed]
- Slutsky AS, Villar J, Pesenti A. Happy 50th birthday ARDS! Intensive Care Med 2016;42:637-9. [Crossref] [PubMed]
- Villar J, Blanco J, Kacmarek RM. Current incidence and outcome of the acute respiratory distress syndrome. Curr Opin Crit Care 2016;22:1-6. [Crossref] [PubMed]
- Villar J, Blanco J, del Campo R, et al. Assessment of PaO2/FiO2 for stratification of patients with moderate and severe acute respiratory distress syndrome. BMJ Open 2015;5:e006812. [Crossref] [PubMed]
- Villar J, Ambrós A, Soler JA, et al. Age, PaO2/FIO2, and Plateau Pressure Score: A Proposal for a Simple Outcome Score in Patients With the Acute Respiratory Distress Syndrome. Crit Care Med 2016;44:1361-9. [Crossref] [PubMed]
- Knaus WA, Draper EA, Wagner DP, et al. APACHE II: a severity of disease classification system. Crit Care Med 1985;13:818-29. [Crossref] [PubMed]
- Baker SP, O'Neill B, Haddon W Jr, et al. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma 1974;14:187-96. [Crossref] [PubMed]
- Heffner JE, Brown LK, Barbieri CA, et al. Prospective validation of an acute respiratory distress syndrome predictive score. Am J Respir Crit Care Med 1995;152:1518-26. [Crossref] [PubMed]
- Cooke CR, Shah CV, Gallop R, et al. A simple clinical predictive index for objective estimates of mortality in acute lung injury. Crit Care Med 2009;37:1913-20. [Crossref] [PubMed]
- Murray JF, Matthay MA, Luce JM, et al. An expanded definition of the adult respiratory distress syndrome. Am Rev Respir Dis 1988;138:720-3. [Crossref] [PubMed]
- Apgar V. A proposal for a new method of evaluation of the newborn infant. Curr Res Anesth Analg 1953;32:260-7. [Crossref] [PubMed]
- Gawande AA, Kwaan MR, Regenbogen SE, et al. An Apgar score for surgery. J Am Coll Surg 2007;204:201-8. [Crossref] [PubMed]
- Thorn CC, Chan M, Sinha N, et al. Utility of the Surgical Apgar Score in a district general hospital. World J Surg 2012;36:1066-73. [Crossref] [PubMed]
- Villar J, Pérez-Méndez L, Basaldúa S, et al. A risk tertiles model for predicting mortality in patients with acute respiratory distress syndrome: age, plateau pressure, and P(aO(2))/F(IO(2)) at ARDS onset can predict mortality. Respir Care 2011;56:420-8. [Crossref] [PubMed]
- Santos RS, Silva PL, Rocco JR, et al. A mortality score for acute respiratory distress syndrome: predicting the future without a crystal ball. J Thorac Dis 2016;8:1872-6. [Crossref] [PubMed]
- Repessé X, Aubry A, Vieillard-Baron A. On the complexity of scoring acute respiratory distress syndrome: do not forget hemodynamics! J Thorac Dis 2016;8:E758-64. [Crossref] [PubMed]
- Gee MH, Gottlieb JE, Albertine KH, et al. Physiology of aging related to outcome in the adult respiratory distress syndrome. J Appl Physiol (1985) 1990;69:822-9. [PubMed]
- Shiu KK, Rosen MJ. Is there a safe plateau pressure threshold for patients with acute lung injury and Acute Respiratory Distress Syndrome? Am J Respir Crit Care Med 2006;173:686; author reply 687. [Crossref] [PubMed]
- Rysavy M. Evidence-based medicine: a science of uncertainty and an art of probability. Virtual Mentor 2013;15:4-8. [Crossref] [PubMed]
- Rocker G, Cook D, Sjokvist P, et al. Clinician predictions of intensive care unit mortality. Crit Care Med 2004;32:1149-54. [Crossref] [PubMed]
- Vincent JL, Hall JB, Slutsky AS. Ten big mistakes in intensive care medicine. Intensive Care Med 2015;41:505-7. [Crossref] [PubMed]
- Cooke CR. The siren song of simple tools that predict mortality. Respir Care 2011;56:533-5. [Crossref] [PubMed]
- Amato MB, Meade MO, Slutsky AS, et al. Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med 2015;372:747-55. [Crossref] [PubMed]
- Schuster DP. What is acute lung injury? What is ARDS? Chest 1995;107:1721-6. [Crossref] [PubMed]
- Villar J, Blazquez MA, Lubillo S, et al. Pulmonary hypertension in acute respiratory failure. Crit Care Med 1989;17:523-6. [Crossref] [PubMed]


