Small cervical incision facilitates minimally invasive resection of non-invasive thoracic inlet tumor
Introduction
Nowadays, the thoracic inlet tumors still impose great challenges to thoracic surgeons due to their unique anatomic location in the thoracic inlet, where they were hidden behind the clavicle and first rib, and were close to important subclavicular vessels and brachial plexus (1). In order to obtain an excellent exposure, open approaches were conventionally applied either via a semi-clamshell incision or via thoracotomy in combination with sternotomy (2). However, these open approaches were associated with incisional trauma, significantly intensifying postoperative pain, increasing morbidity and yielding longer hospital stays (3). With the development of minimally invasive techniques, several studies (2-5) have focused on video-assisted thoracoscopic surgery (VATS) for the treatment of thoracic inlet tumor. Although VATS minimizes incisional trauma, it was found to markedly increase the incidence of brachial plexus injury as compared with open approaches (5). Therefore, only a few skillful thoracic surgeons (2) are capable of accomplishing totally thoracoscopic resection of thoracic inlet tumors. As a result, whether the minimally invasive surgical techniques can be used in resecting the thoracic inlet tumor in a safer and easier way and how to do it are major clinical concerns.
Methods
Here we report that a small anterior sternocleidomastoid muscle incision in the neck can facilitate minimally invasive resection of the non-invasive thoracic inlet tumors. In this surgical approach, VATS was applied for resection of the intra-thoracic part of thoracic inlet tumors, while for the cervical and subclavicular parts, which is the blind area of thoracoscope, the small cervical incision was used to facilitate the exposure. Therefore, the feeling of the surgeons’ fingers and direct visualization of the cervical part can excellently compensate the blind area of thoracoscope, making the resection of thoracic inlet tumors safely and effectively. The followings were two cases undergoing this surgical approach for a complete resection of thoracic inlet tumors, and inform consent was obtain from both patients. This work was also approved by the Ethics Review Committee of West China hospital.
Results
Case 1
A 70-year-old female was admitted into our department complaining of coughing and chest distress. Her computed tomography (CT) scan showed a regular-shaped and low-dense mass with a size of 5.6 cm × 4.1 cm in the right posterior mediastinum, occupying posterior thoracic inlet (Figure 1A) and extending to adjacent structures. Her magnetic resonance image (MRI) showed the round-shaped mass as relatively high intensity on T1W1, and high intensity on T2W1 (Figure 1B).
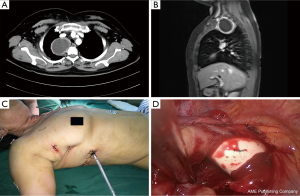
Operation was carried out under general anesthesia with a double lumen intubation. As most part of the tumor was located in the posterior thoracic inlet, a small cervical incision about 4 cm along the anterior margin of left sternocleidomastoid muscle was initially made when the patient was placed in the supine decubitus position. After the transection of omohyoid muscle, a blunt dissection was carried out deep into the cervical esophageal bed. A further exploration was made into the thoracic inlet along the esophageal bed. Then the cervical incision was covered with clean gauze, and, the patient was then re-placed in the full left decubitus position. After resterilization of the neck and chest wall, three conventional VATS ports were made: one in the fourth intercostal space along the right posterior axillary line, one in the sixth intercostal space along the middle axillary line, and another in the ninth intercostal space along right posterior axillary line (Figure 1C). VATS was applied in the thorax for dissecting the inferior aspect of the mass, and through the cervical incision blunt dissection of adjacent blood vessels and nerves as well as the superior aspect of the mass was achieved. And at the meantime, we could also use our fingers to separate the adjacent blood vessels and nerves from the mass. The sensation of our fingers as well as the direct view from the cervical incision could compensate the blind area of the thoracoscope in the thorax, and could help us to obtain a whole sensation of the mass and successfully avoid injuries to adjacent important structures going through the thoracic inlet (Figure 1D). The mass was gently pulled out from the VATS port. Rightly after the operation, local injection of ropivacaine to the incision as well as a self-controlled analgesia pump was applied for pain control. The total operation time was about 60 minutes, and the total blood loss was about 50 mL. Postoperatively, the mass was pathologically diagnosed as neurogenic tumor. No postoperative complications were observed, and the patient was also discharged from the hospital on postoperative day 3.
Case 2
A 40-year-old female was presented to our department during a general checkup with a CT scan showing a regular-shaped mass with a size of 4.1 cm × 3.2 cm in the left posterior mediastinum, occupying anterior thoracic inlet (Figure 2A) and being closely adjacent to left subclavicular artery. The subsequent MRI showed the mass as high intensity on T1W1, and high intensity on T2W1 (Figure 2B).
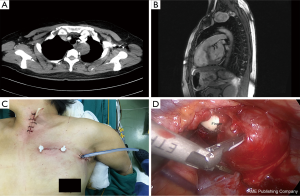
Operation was carried out under general anesthesia with double lumen intubation. This patient was placed in the supine decubitus position. A small cervical incision about 4 cm was first made along the anterior margin of left sternocleidomastoid muscle. After transection of the omohyoid muscle, the common carotid artery sheath was identified and retracted laterally. A blunt dissection was carried out deep into the cervical esophageal bed, and a further exploration was made into the thoracic inlet along the esophageal bed. Then two VATS ports were made: one in the second intercostal space along the left midclavicle line and another in the third intercostal space along the left anterior axillary line. Based upon the convenience of visualization and dissection of the inferior aspect of the mass, the thoracoscope and the surgical instruments can be alternatively induced into the thoracic cavity through either one of the two ports. Through the cervical incision, we could use our fingers to separate the adjacent blood vessels and nerves from the mass, so the blind area of the thoracoscope was compensated by the sensation of our fingers from the cervical incision (Figure 2C). We could even acquire a direct view of the cervical part of the mass, and launch a dissection there easily. This combined approach helped us to obtain a whole sensation of the mass without any blind area and successfully avoid injuries to adjacent important structures including the blood vessels and brachial plexus (Figure 2D). The mass was completely resected and gently pulled out from the thoracic port. Rightly after the operation, local injection of ropivacaine to the incision as well as a self-controlled analgesia pump was applied for pain control. The total blood loss was about 50 mL, and total operation time was about 45 minutes. Postoperatively, the mass was pathologically diagnosed as neurogenic tumor. No postoperative complications were observed, and she was discharged from the hospital on postoperative day 2.
Discussion
The thoracic inlet is an incapacious structure through which the subclavicular blood vessels and the brachial plexus are going. Therefore, tumors locating in thoracic inlet impose great challenge for thoracic surgeons. Traditionally, an anterior transcervical-thoracic approach (6) or transmanubrial osteomuscular sparing approach (7) was applied for complete resection of thoracic inlet tumors. Later, an anterior cervical-transsternal approach was introduced (8). Although these open approaches can yield excellent exposure, they are all associated with prominent incisional trauma, which does not fit in with the widely accepted concept of minimal invasive surgery. With the development of minimal invasive techniques, VATS was applied in a combination with a supraclavicular or transclavicular approach in resection of thoracic inlet tumors (4,9). This combination showed an excellent extirpation of the tumor and significantly decreased the incisional trauma (9,10). However, this approach had to resect sternocleidomastoid, omohyoid, and anterior scalene muscles, and sometimes even the clavicle. On the other hand, the supraclavicular region is not a usual operative field to all thoracic surgeons. Recently, Tanaka et al. (2) reported a totally thoracoscopic resection of a thoracic inlet tumor. But the size of the tumor they resected was relatively small (about 2–3 cm), so the vital blood vessels and brachial plexus may not be closely related to the tumor. As we all know, the larger the thoracic inlet tumor size the closer it locates to the surrounding blood vessels and the brachial plexus. Therefore, the thoracoscopic resection of the thoracic inlet tumor still remains challenge to the thoracic surgeons. And it still becomes more dangerous when tumor size is large. Here, we presented our preliminary experience of combining VATS with a small cervical incision to significantly reduce the difficulty of thoracoscopic tumor resection as well as incisional trauma. As we all know, thoracic inlet could be divided into three compartments (anterior, middle, and posterior compartments) on the basis of anterior, middle, and posterior scalene muscles (11). When the tumor locates in different compartments, the patient positioning as well as the setting of the ports should be carefully designed. Take case 1 for example, the tumor was located posterior compartment, and the patient was first placed in a lateral decubitus position and then a regularly commonly used three ports of VATS was applied to obtain an excellent visualization of the tumors as well as enough operation space after pulling the deflated lung anteriorly. However, in case 2, the tumor was located in anterior compartment, and the patient was first placed in a supine decubitus position and then an anterior port for VATS was applied for easy operation, as the deflated lung occupied the posterior part of the thorax. Therefore, our current combined approach of VATS with a small cervical incision was feasible, safe, and more importantly, easy to be mastered by general thoracic surgeons.
Our combined approach of VATS with a small cervical incision owns several advantages. It is less invasive as compared with previously reported open approaches (4,9), for the fact that the cervical incision was small (about 4 cm) and only needs to cut off a tiny muscle in the neck (the omohyoid muscle). Therefore our two patients showed little blood loss and achieved rapid postoperative rehabilitation. This small cervical incision provides an access to the superior end of the tumor, so that the thoracic surgeon can use his fingers to dissect and free the adjacent blood vessels and nerves from the tumors. Gentle blunt dissection is a key point to avoid adverse injury because bigger solid tumors (for example: greater than 6 cm) in the thoracic inlet may inherently have larger pedicle and vascular feeding from adjacent structures. In this circumstance, gentle blunt dissection by fingers through the cervical incision can help to feel the pedicle of the tumor, and isolate it from surrounding structures. The diameter of the pedicle can also be estimated by the fingers. If its diameter is less than 5 mm, such as in our reported two cases, ultrasonic scalpel can be used to directly cut it off, otherwise, forceps can be directed by the fingers to clamp the pedicle and then perform the subsequential cut off. Our initial two cases proved that this combined approach was fit for larger tumors located in the thoracic inlet (in our cases, the size of the tumors was about 5 cm), because general thoracic surgeon are more familiar with the anatomy of cervicle than that of the subclavicular region. Our reported approach was not only proved to be feasible in our current benign tumors, but also in malignant tumor as reported by Asaka et al. (3).
Conclusions
This combined approach can significantly reduce incisional trauma and permit a safe and radical resection of the tumor in a complex and delicate area of the thoracic inlet.
Acknowledgements
Funding: This project was supported by Natural Science Foundation of China (No. 31071210; No. 30400440).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by Ethics Review Committee of West China hospital of No. 20160501 and written informed consent was obtained from all patients.
References
- Honguero Martínez AF, Rombolá CA, et al. Technical aspects of the anterior transmanubrial approach in thoracic inlet tumor surgery. Arch Bronconeumol 2012;48:419-22. [Crossref] [PubMed]
- Tanaka T, Ueda K, Hayashi M, et al. Totally thoracoscopic resection of a superior mediastinal tumor extending above the thoracic inlet. J Thorac Cardiovasc Surg 2011;141:1323-5. [Crossref] [PubMed]
- Asaka S, Yoshida K, Hashizume M, et al. A mediastinal liposarcoma resected using a double approach with a thoracoscope. Thorac Cardiovasc Surg Rep 2013;2:46-9. [Crossref] [PubMed]
- Yan S, Sun Y, Sun Y, et al. Thoracoscopic transclavicular approach for a large thoracic inlet tumor. Ann Thorac Surg 2014;98:e91-3. [Crossref] [PubMed]
- Yang C, Zhao D, Zhou X, et al. A comparative study of video-assisted thoracoscopic resection versus thoracotomy for neurogenic tumours arising at the thoracic apex. Interact Cardiovasc Thorac Surg 2015;20:35-9. [Crossref] [PubMed]
- Dartevelle PG, Chapelier AR, Macchiarini P, et al. Anterior transcervical-thoracic approach for radical resection of lung tumors invading the thoracic inlet. J Thorac Cardiovasc Surg 1993;105:1025-34. [PubMed]
- Grunenwald D, Spaggiari L. Transmanubrial osteomuscular sparing approach for apical chest tumors. Ann Thorac Surg 1997;63:563-6. [Crossref] [PubMed]
- Ladas G, Rhys-Evans PH, Goldstraw P. Anterior cervical-transsternal approach for resection of benign tumors at the thoracic inlet. Ann Thorac Surg 1999;67:785-9. [Crossref] [PubMed]
- Akashi A, Ohashi S, Yoden Y, et al. Thoracoscopic surgery combined with a supraclavicular approach for removing superior mediastinal tumor. Surg Endosc 1997;11:74-6. [Crossref] [PubMed]
- Givigliano F, La Rocca A, La Manna C, et al. Minimally invasive combined approach for an hourglass-shaped mass at the thoracic inlet. J Thorac Cardiovasc Surg 2007;134:528-9. [Crossref] [PubMed]
- Rusch VW. Management of Pancoast tumours. Lancet Oncol 2006;7:997-1005. [Crossref] [PubMed]


