Organizing pneumonia presenting after ulcerative colitis remission
Introduction
The inflammatory bowel diseases (IBDs), Crohn’s disease (CD) and ulcerative colitis (UC), are systemic illness with a constellation of extraintestinal manifestations (EIMs) that affect almost every organ and system (1,2). The incidence of EIM in IBD has been reported to range from 21% to 41%. Furthermore, its frequency increases with length of disease, and it is more frequent in CD. However, pulmonary involvement is far less common than the involvement of other organs, and organizing pneumonia (OP) involving the lung parenchyma is a rare EIM of IBD (2-6). We report a case of organizing pneumonia (OP) in a patient with UC in remission confirmed by endoscopic biopsy.
Case report
A 81-year-old female non-smoker with ulcerative colitis (UC) diagnosed 12 years previously, presented with a 10-day history of a non productive cough and dyspnea on exertion. Since had been initially diagnosed as having UC by endoscopic biopsy, and the disease had generally been well controlled with oral sulfasalazine, mesalazine, and/or prednisone for 8 years. Thereafter, mild disease activity was controlled with mesalazine rectal suspension alone, and she discontinued the mesalazine rectal suspension 5 months prior to this admission. She also had a 12-year history of hypertension, but had no history of lung disease, of EIMs, of significant occupational exposures, or of any recent travel.
On admission, her symptoms were a febrile sensation, general weakness, and decreased appetite. Physical examination revealed; respiratory rate of 22 beats/min, temperature 36.9 °C, pulse of 90 beats/min, blood pressure 130/80 mmHg, and room air oxygen saturation of 88%. She had inspiratory crackles in both lung bases, and there was no evidence of digital clubbing. The remainder of her examination was normal. Laboratory data included a white cell count of 12,130/mm3 (90.8% neutrophils, 0.5% eosinophils), an erythrocyte sedimentation rate of 86 mm/h (normal, 0-22 mm/h) and a C-reactive protein level of 13.18 mg/dL (normal, 0-0.3 mg/dL). Arterial blood gas values included a partial oxygen pressure of 74 mmHg, a partial carbon dioxide pressure of 26 mmHg, a pH of 7.49, and an oxygen saturation of 96% while resting on 2 L/min of oxygen. Chest radiography and computed tomography showed new diffuse, patchy densities with focal areas of nodules and reticular opacities involving the right lung and to a lesser extent the left lung (Figure 1A,B). Chest radiography obtained 4 months ago was normal. Colonoscopy and biopsy revealed no evidence of active inflammation or colitis.
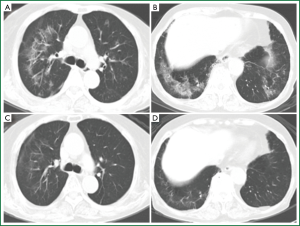
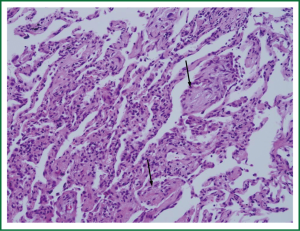
Serology for Mycoplasma pneumonia, Legionella pneumophilia, Chlamydia pneumonia, and Aspergillus were negative. Sputum stains for mycobacterial tuberculosis were negative. Despite intravenous antibiotics and supportive care for 10 days, her respiratory symptoms persisted. Pulmonary function testing revealed; forced vital capacity 2.28 L (117% of predicted), forced expiratory volume in one second 1.61 L (112% of predicted), total lung capacity 4.00 L (44% of predicted), and diffusing capacity 8.30 mL/min/mm Hg (48% of predicted). Bronchoscopy revealed hyperemic airways, but no other abnormality. Bronchoalveolar lavage fluid had a white blood cell differential count of 3% neutrophils, 33% lymphocytes, 22% monocytes, and 42% macrophages. Transbronchial biopsy demonstrated mild chronic inflammation with fibrous plugs in alveolar spaces (Figure 2). Methenamine silver stains failed to reveal fungi or Pneumocystis carinii, and cultures for organisms, including bacteria, fungi, mycobacteria, and virus, were negative. The findings in this case were consistent with an organizing pneumonia. Prednisolone was administered for 4 weeks at 1 mg/kg/day, and consequent subjective and radiographic improvements were dramatic (Figure 1C,D). The prednisolone was then tapered and discontinued at 12 weeks, and subsequently the patient continued to do well.
Discussion
EIMs involving various organs and systems, such as, joints, skin, liver, eye, mouth, and the coagulation system, either precede the onset of UC symptoms or appear and evolve in parallel with intestinal manifestations in 10% to 30% of patients (7). In contrast, pulmonary manifestations are described much less frequently than other EIMs, and may present several years after bowel disease onset (2-5).
Pulmonary manifestations in patients with IBD were first recognized by Kraft et al. (8), and since, sporadic cases and case series have expanded the number of patterns of pulmonary involvement that occur in IBD. Pulmonary manifestations vary from subclinical pulmonary findings to airway disorders, and obstructive and interstitial lung disease, which in some cases may result in extremely serious situations (2-6). In addition, it is important to appreciate that pulmonary manifestations can be caused by the drugs used to treat IBD, because in such cases, they usually improve after medication discontinuation, and in some cases respond to steroid therapy (4,9).
OP (formerly called bronchiolitis obliterans organizing pneumonia) involving the lung parenchyma, is considered a rare disease, and has been associated with many specific causes, including IBD (10). In patients with IBD, pulmonary diseases involving the lung parenchyma are relatively uncommon among all pulmonary manifestations (5). According to our review of the literature, OP has been described only in 2% (9/400) and 13% (21/155) of patients with pulmonary involvement in IBD, and more commonly in UC (4,5,11). However, the cumulative volume of published sporadic case reports on the pulmonary manifestations of IBD are more common than is generally appreciated (5). In many cases, a lung biopsy is required to establish an accurate diagnosis, and systemic steroid therapy is the norm (3), as in our case.
In general, UC remission is defined as complete symptom resolution, that is, a stool frequency of ≤3/day with no bleeding or urgency, and endoscopic mucosal healing (12). Although sporadic OP cases have been reported in inactive bowel disease (2,11,13), to the best of our knowledge, no case of OP in a patient with UC remission (confirmed histologically) has been previously reported in the English literature. Our patient had discontinued IBD medication prior to admission, and diagnosed to be in remission by endoscopic biopsy.
In summary, this is the first report of OP in an elderly patient after UC remission confirmed by histology. OP is considered a rare EIM in patients with IBD. However, this disorder is being increasingly recognized probably because of developments of in chest CT scan technology and the prolonged life span of patients. Therefore, a high degree of suspicion is necessary to detect pulmonary manifestations as they may present years after bowel disease. Nevertheless, early detection is important as the risk of morbidity and mortality in patients with IBD are almost certainly reduced by prompt appropriate treatment.
Acknowledgements
This work was supported by INHA UNIVERSITY HOSPITAL Research Grant.
Disclosure: The authors declare no conflict of interest.
References
- Kirsner JB, Shorter RG. Recent developments in “nonspecific” inflammatory bowel disease (first of two parts). N Engl J Med 1982;306:775-85.
- Camus P, Piard F, Ashcroft T, et al. The lung in inflammatory bowel disease. Medicine (Baltimore) 1993;72:151-83.
- Camus P, Colby TV. The lung in inflammatory bowel disease. Eur Respir J 2000;15:5-10.
- Storch I, Sachar D, Katz S. Pulmonary manifestations of inflammatory bowel disease. Inflamm Bowel Dis 2003;9:104-15.
- Black H, Mendoza M, Murin S. Thoracic manifestations of inflammatory bowel disease. Chest 2007;131:524-32.
- Casella G, Villanacci V, Di Bella C, et al. Pulmonary diseases associated with inflammatory bowel diseases. J Crohns Colitis 2010; 4:384-9.
- Danese S, Fiocchi C. Ulcerative colitis. N Engl J Med 2011;365:1713-25.
- Kraft SC, Earle RH, Roesler M, et al. Unexplained bronchopulmonary disease with inflammatory bowel disease. Arch Intern Med 1976;136:454-9.
- Foster RA, Zander DS, Mergo PJ, et al. Mesalamine-related lung disease: clinical, radiographic, and pathologic manifestations. Inflamm Bowel Dis 2003;9:308-15.
- Drakopanagiotakis F, Polychronopoulos V, Judson MA. Organizing pneumonia. Am J Med Sci 2008;335:34-9.
- Basseri B, Enayati P, Marchevsky A, et al. Pulmonary manifestations of inflammatory bowel disease: case presentations and review. J Crohns Colitis 2010;4:390-7.
- Stange EF, Travis SP, Vermeire S, et al. European evidence-based Consensus on the diagnosis and management of ulcerative colitis: Definitions and diagnosis. J Crohns Colitis 2008;2:1-23.
- Gil-Simón P, Barrio Andrés J, Atienza Sánchez R, et al. Bronchiolitis obliterans organizing pneumonia and Crohn's disease. Rev Esp Enferm Dig 2008;100:175-7.


