The fractional flow reserve gray zone has never been so narrow
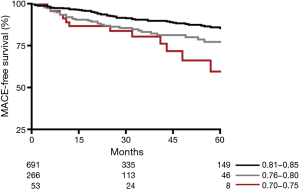
Fractional flow reserve (FFR) is the gold standard in the invasive hemodynamic assessment of epicardial coronary artery stenoses. FFR is defined as the ratio of maximal flow achievable in the stenotic coronary artery to the maximal flow achievable in the same coronary artery if it was normal. In other words, FFR informs the clinician to what extent blood flow is reduced and can be improved after revascularization: e.g., a FFR of 0.60 means that coronary blood flow is 60% of what should be in the absence of the epicardial stenosis, and it could improve by 40% after percutaneous coronary intervention. FFR is highly reproducible, has an unequaled spatial resolution and it is easy to measure during diagnostic coronary angiography. A FFR ≤0.75 has 100% positive predictive value, whereas FFR >0.80 has more than 95% negative predictive value for reversible myocardial ischemia at non-invasive functional testing (1). The DEFER trial, conducted in the era of bare metal stents, has demonstrated that it is safe to defer to medical therapy coronary stenoses with FFR above 0.75 in stable patients with single vessel disease (2). In the era of drug eluting stents, the threshold of 0.80 was adopted in the FAME 1 and 2 trials to guide clinical decision-making, because in a minority of patients an FFR value between 0.75 and 0.80 was found to be associated with typical exercise-induced angina and reversible flow maldistributions (3). Performing revascularization of coronary stenosis with FFR ≤0.80 has been consistently associated with improved clinical outcome in randomized trials as well as in routine clinical practice (4,5). Nevertheless, none of these studies have specifically investigated the clinical impact of coronary stenoses with FFR within the so-called gray zone of values comprised between 0.75 and 0.80. Johnson et al. demonstrated a risk continuum between FFR and clinical outcome (6), i.e., the lower the FFR values the higher the risk of cardiovascular events if these patients are treated with conservative therapy. Conversely, the benefits potentially deriving from revascularization progressively increase with decreasing FFR values. Interestingly, the balance between risks and benefits of revascularization tilts over to optimal medical therapy just in correspondence of the FFR gray zone. In fact, with FFR values above 0.80 no additional clinical benefits are to be expected from revascularization as compared with medical therapy, but rather an inappropriate increased iatrogenic risk of events related to the procedure or to the associated antiplatelet therapy. This risk continuum has been recently confirmed also in the narrow range of FFR values comprised between 0.70 and 0.85 (7). In fact, a progressive decrease in major adverse cardiovascular event (MACE)-free survival has been observed in patients with single vessel single stenosis but with FFR values going from 0.85 to 0.70 (Figure 1). This gradient of MACE rate was particularly evident with lesions located in proximal coronary segments, underscoring the importance to warrant revascularization to these stenoses even with FFR values within the gray zone of 0.75–0.80.
Dr. Tanaka et al. recently highlighted the challenges and opportunities of non-invasive diagnostic imaging in detecting coronary stenoses with abnormal FFR values (i.e., ≤0.80), raising the question if invasive FFR assessment is indeed necessary in all patients with stable coronary artery disease (8). In patients with single vessel disease and clear-cut positive non-invasive functional evaluation, clinicians might refrain from performing additional tests and undertake the appropriate decision-making based on the coronary angiography. Yet, FFR in this setting might still confirm the relative contribution of the epicardial disease to the ischemic burden and suggest the expected improvement achievable in the coronary flow after revascularization. In patients with multivessel disease, the role of invasive FFR is paramount due to the limited spatial resolution of traditional non-invasive functional assessment. In these patients, the interventional cardiologists are aware of the presence of an ischemic substrate though are left with dilemmas as to which coronary segment is indeed responsible and deserves revascularization. Nevertheless, novel techniques like the FFR-derived from coronary computed tomography angiography (FFR-CT), the CT perfusion (CTP), the Transluminal Attenuation Gradient by 320-detector row computed tomography (TAG320) or the combined myocardial perfusion scintigraphy with CT (MPS-CT) are raising increasing interest for their ability to provide non-invasively both anatomic and hemodynamic information of coronary artery. Initial studies have, in fact, confirmed improved specificity, and superior diagnostic accuracy as compared with the traditional techniques to predict abnormal invasive FFR values (9). In addition, these techniques might significantly impact the management strategies by reducing the rate of patients with non-obstructive coronary artery disease referred to invasive angiography (10). Remaining potential challenges associated with some of these techniques like the dose of radiations and volume of contrast medium might still hamper their widespread application.
Acknowledgements
None.
Footnote
Provenance: This is an invited article commissioned by the Section Editor Yue Liu (Associate professor, Department of Cardiology, The First Affiliated Hospital of Harbin Medical University, Harbin, China).
Conflicts of Interest: The authors have no conflicts of interest to declare.
Response to:Tanaka H, Okada T, Kihara Y. Shedding light on the gray zone. J Thorac Dis 2016;8:1421-4.
References
- Pijls NH, De Bruyne B, Peels K, et al. Measurement of fractional flow reserve to assess the functional severity of coronary-artery stenoses. N Engl J Med 1996;334:1703-8. [Crossref] [PubMed]
- Zimmermann FM, Ferrara A, Johnson NP, et al. Deferral vs. performance of percutaneous coronary intervention of functionally non-significant coronary stenosis: 15-year follow-up of the DEFER trial. Eur Heart J 2015;36:3182-8. [Crossref] [PubMed]
- De Bruyne B, Pijls NH, Bartunek J, et al. Fractional flow reserve in patients with prior myocardial infarction. Circulation 2001;104:157-62. [Crossref] [PubMed]
- van Nunen LX, Zimmermann FM, Tonino PA, et al. Fractional flow reserve versus angiography for guidance of PCI in patients with multivessel coronary artery disease (FAME): 5-year follow-up of a randomised controlled trial. Lancet 2015;386:1853-60. [Crossref] [PubMed]
- De Bruyne B, Fearon WF, Pijls NH, et al. Fractional flow reserve-guided PCI for stable coronary artery disease. N Engl J Med 2014;371:1208-17. [Crossref] [PubMed]
- Johnson NP, Tóth GG, Lai D, et al. Prognostic value of fractional flow reserve: linking physiologic severity to clinical outcomes. J Am Coll Cardiol 2014;64:1641-54. [Crossref] [PubMed]
- Adjedj J, De Bruyne B, Floré V, et al. Significance of Intermediate Values of Fractional Flow Reserve in Patients With Coronary Artery Disease. Circulation 2016;133:502-8. [Crossref] [PubMed]
- Tanaka H, Okada T, Kihara Y. Shedding light on the gray zone. J Thorac Dis 2016;8:1421-4. [Crossref] [PubMed]
- Nørgaard BL, Leipsic J, Gaur S, et al. Diagnostic performance of noninvasive fractional flow reserve derived from coronary computed tomography angiography in suspected coronary artery disease: the NXT trial (Analysis of Coronary Blood Flow Using CT Angiography: Next Steps). J Am Coll Cardiol 2014;63:1145-55. [Crossref] [PubMed]
- Douglas PS, Pontone G, Hlatky MA, et al. Clinical outcomes of fractional flow reserve by computed tomographic angiography-guided diagnostic strategies vs. usual care in patients with suspected coronary artery disease: the prospective longitudinal trial of FFR(CT): outcome and resource impacts study. Eur Heart J 2015;36:3359-67. [Crossref] [PubMed]


