ASCENDing the anaplastic lymphoma kinase ladder: a tale of two C-nibs
Targeting driver mutations in oncogene addicted advanced non-small cell lung cancer (NSCLC) has revealed the Achilles heel and revolutionized its management in the last one decade (1). At present, approximately 2/3rd of lung adenocarcinomas can be classified based on the driver genomic alteration (2). Anaplastic lymphoma kinase (ALK) gene rearrangement, particularly EML4-ALK fusion is seen in 3−7% patients of NSCLC, more so in younger patients and non-smokers (3-5). Crizotinb, a dual MET and ALK inhibitor, is the first approved drug for patients with metastatic NSCLC harboring ALK gene rearrangements, based on its superiority in terms of objective response rates (ORRs) and progression free survival (PFS) over standard single agent and platinum based doublet chemotherapy in second and first line settings respectively (6,7). Despite initial encouraging response, majority of the patients progress after median of 8–14 months. Acquired resistance to crizotinib emerges because of second site mutations affecting the binding of the drug in the kinase domain or by means of activation of pathways that bypass the original oncogenic kinase signal (8).
Ceritinib is another tyrosine kinase inhibitor of ALK with 20 times higher potency than crizotinib as has been demonstrated in enzymatic assays. Preclinical models of acquired resistance to crizotinib, revealed that ceritinib potently overcomes crizotinib-resistant mutations in particular, L1196M, G1269A, I1171T, and S1206Y (9). In a recent phase I trial (ASCEND 1), ceritinib has shown a robust clinical activity, both intracrainial and extracranial, in previously treated advanced ALK rearranged NSCLC. ORRs of 72% in ALK inhibitor naive and 56% in crizotinib treated patients were observed. In 94 patients with brain metastasis, 79% of ALK inhibitor naïve and 65% of crizotinib treated patients achieved intracranial disease control (10).
In the presently commented phase 2 trial (ASCEND 2), Crinò et al. (11) have reported the efficacy and safety of ceritinib in patients with ALK rearranged advanced NSCLC who had received at least one platinum based doublet chemotherapy and had disease progression on crizotinib as their last treatment. A total of 140 eligible patients were treated with ceritinib 750 mg daily till disease progression or unacceptable toxicity. The primary objective of the study was investigator’s assessed ORRs and secondary objectives were blinded independent review committee (BIRC) assessed overall survival (OS), safety, and patient-reported outcomes (PROs).
The investigator’s assessed ORR was 38.6% (95% CI, 30.5–47.2%) and the disease control rate (DCR) was 77.1% (95% CI, 69.3–83.8%). The responses were early (median time to response 1.8 months) and durable (median duration of response 9.7 months). The median PFS was 5.7 months (95% CI, 5.4–7.6). There were 100 patients with brain metastasis, 72 of which had received brain radiotherapy. The whole body ORR in these patients was 33% and DCR was 74%. The median PFS of these patients was 5.4 months. Intracranial response was evaluated in 20 patients who had active target lesions at study entry. Objective intracranial response was observed in 45% and intracranial disease control was seen in 80% patients. Grade 3–4 toxicities were reported in 71.4% patients, the most common being elevated ALT and gamma-glutamyltransferase, which occurred in 15.7% and 9.3%, respectively. Treatment discontinuation due to toxicities was reported in 7.9% patients. More than 75% patients reported drug related nausea, vomiting and diarrhea however majority were grade 1–2. In patient reported outcomes, health-related quality of life (QOL) was maintained during treatment, and no significant change from baseline was observed in the QLQ-C30 global QOL or functional scale score.
The reported ORR was lower in ASCEND 2 as compared to ASCEND 1 (38.6% vs. 56% in ALK inhibitor treated patients). However, DCRs and median PFS were comparable. This may have been due to presence of more heavily pretreated patients in ASCEND 2 as compared to ASCEND 1. Putting both these studies together, ceritinib shows encouraging activity for both intracranial and extracranial disease in crizotinib pretreated patients. ALK dependent crizotinib resistance generally occurs either due to amplification of ALK gene or various tyrosine kinase domain mutations. Ceritinib activity in both these trials was independent of the type of mutation.
Alectinib is another potent and highly selective ALK inhibitor that has received US-FDA approval for ALK positive advanced NSCLC after failure of crizotinib. It has shown impressive ORR of 50% and 48% and median PFS of 8.9 and 8.1 months in two recent phase 2 trials (12,13). Alectinib has shown significant CNS activity as the intracranial DCRs were 83 and 100% respectively. Gadgeel et al. have recently reported the pooled analysis of CNS response of alectinib in these two trials (14). In patients with baseline measurable disease the CNS ORR was 64% and CNS DCR was 90%. Similarly in patients with measurable and non-measurable disease CNS ORR was 42.6% and CNS DCR was 85.3%. Responses were better in patients who had not received prior cranial radiotherapy (35.8% vs. 58.5%). In both these trials, alectinib has shown good safety profile. Majority of the adverse effects were grade 1–2. Grade 3–4 adverse events were seen in 34% and 24% patients only. Table 1 summarizes the inter-trial comparison of whole body and intracranial efficacy of three ALK inhibitors (crizotinib, ceritinib and alectinib).
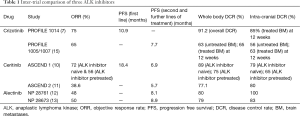
Full table
With development of next generation of ALK inhibitors, we have now multiple options in any given patient who has relapsed on crizotinib. But the million-dollar question is which next-generation ALK inhibitor should be prescribed? So far there is no published head to head randomized trial answering the question of choice of ALK inhibitors or even the optimum sequence of ALK inhibitors.
Based on the available single-arm studies of alectinib and ceritinib in crizotinib-resistant disease, the systemic efficacy of these drugs may be comparable. There are potential advantages of alectinib over ceritinib, including alectinib’s documented intracranial activity and its favorable safety profile, but, ultimately, the choice of next-generation ALK inhibitor will need to be individualized for each patient.
Another important question is the optimum sequence of new generation of ALK inhibitors. In the literature, there are reports supporting the sequential use of alectinib after ceritinib, or vice versa. Alectinib was found to be active in progressive CNS disease or in patients who have developed the ceritinib resistance mutation F1174V (16). Similarly, ceritinib may be active after alectinib in patients who become resistant due to the alectinib resistance mutation I1171 (17). Hence, the type of resistance mutation might help in selecting the optimum ALK inhibitor after crizotinib failure, necessitating tumor biopsy at the time of disease progression.
Although significant advancements have occurred in the treatment of advanced ALK positive NSCLC with multiple new generations ALK inhibitors, resistance to these drugs is also inevitable. More pragmatic trials are needed to find out the right choice of TKI based on efficacy, tolerability and resistance mechanisms and to guide the optimum sequence.
Acknowledgements
None.
Footnote
Provenance: This is an invited Commentary commissioned by the Section Editor Long Jiang (Second Affiliated Hospital, Institute of Respiratory Diseases, Zhejiang University School of Medicine, Hangzhou, China).
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Pao W, Girard N. New driver mutations in non-small-cell lung cancer. Lancet Oncol 2011;12:175-80. [Crossref] [PubMed]
- Oxnard GR, Binder A, Jänne PA. New targetable oncogenes in non-small-cell lung cancer. J Clin Oncol 2013;31:1097-104. [Crossref] [PubMed]
- Gainor JF, Varghese AM, Ou SH, et al. ALK rearrangements are mutually exclusive with mutations in EGFR or KRAS: an analysis of 1,683 patients with non-small cell lung cancer. Clin Cancer Res 2013;19:4273-81. [Crossref] [PubMed]
- Doval D, Prabhash K, Patil S, et al. Clinical and epidemiological study of EGFR mutations and EML4-ALK fusion genes among Indian patients with adenocarcinoma of the lung. Onco Targets Ther 2015;8:117-23. [PubMed]
- Bal A, Singh N, Agarwal P, et al. ALK gene rearranged lung adenocarcinomas: molecular genetics and morphology in cohort of patients from North India. APMIS 2016;124:832-8. [Crossref] [PubMed]
- Shaw AT, Kim DW, Nakagawa K, et al. Crizotinib versus chemotherapy in advanced ALK-positive lung cancer. N Engl J Med 2013;368:2385-94. [Crossref] [PubMed]
- Solomon BJ, Mok T, Kim DW, et al. First-line crizotinib versus chemotherapy in ALK-positive lung cancer. N Engl J Med 2014;371:2167-77. [Crossref] [PubMed]
- Katayama R, Shaw AT, Khan TM, et al. Mechanisms of acquired crizotinib resistance in ALK-rearranged lung Cancers. Sci Transl Med 2012;4:120ra17. [Crossref] [PubMed]
- Friboulet L, Li N, Katayama R, et al. The ALK inhibitor ceritinib overcomes crizotinib resistance in non-small cell lung cancer. Cancer Discov 2014;4:662-73. [Crossref] [PubMed]
- Kim DW, Mehra R, Tan DS, et al. Activity and safety of ceritinib in patients with ALK-rearranged non-small-cell lung cancer (ASCEND-1): updated results from the multicentre, open-label, phase 1 trial. Lancet Oncol 2016;17:452-63. [Crossref] [PubMed]
- Crinò L, Ahn MJ, De Marinis F, et al. Multicenter Phase II Study of Whole-Body and Intracranial Activity With Ceritinib in Patients With ALK-Rearranged Non-Small-Cell Lung Cancer Previously Treated With Chemotherapy and Crizotinib: Results From ASCEND-2. J Clin Oncol 2016;34:2866-73. [Crossref] [PubMed]
- Shaw AT, Gandhi L, Gadgeel S, et al. Alectinib in ALK-positive, crizotinib-resistant, non-small-cell lung cancer: a single-group, multicentre, phase 2 trial. Lancet Oncol 2016;17:234-42. [Crossref] [PubMed]
- Ou SH, Ahn JS, De Petris L, et al. Alectinib in Crizotinib-Refractory ALK-Rearranged Non-Small-Cell Lung Cancer: A Phase II Global Study. J Clin Oncol 2016;34:661-8. [Crossref] [PubMed]
- Gadgeel SM, Shaw AT, Govindan R, et al. Pooled Analysis of CNS Response to Alectinib in Two Studies of Pretreated Patients With ALK-Positive Non-Small-Cell Lung Cancer. J Clin Oncol 2016;34:4079-4085. [PubMed]
- Costa DB, Shaw AT, Ou SH, et al. Clinical Experience With Crizotinib in Patients With Advanced ALK-Rearranged Non-Small-Cell Lung Cancer and Brain Metastases. J Clin Oncol 2015;33:1881-8. [Crossref] [PubMed]
- Ou SH, Milliken JC, Azada MC, et al. ALK F1174V mutation confers sensitivity while ALK I1171 mutation confers resistance to alectinib. The importance of serial biopsy post progression. Lung Cancer 2016;91:70-2. [Crossref] [PubMed]
- Katayama R, Friboulet L, Koike S, et al. Two novel ALK mutations mediate acquired resistance to the next-generation ALK inhibitor alectinib. Clin Cancer Res 2014;20:5686-96. [Crossref] [PubMed]


