Esmolol in septic shock: old pathophysiological concepts, an old drug, perhaps a new hemodynamic strategy in the right patient
During sepsis, sympathetic activation plays a pivotal role in optimizing cardiac output and blood pressure by acting on the interplays between heart rate (HR), contractility and vascular tone. The integrity of baroreflex function is fundamental for the maintenance of hemodynamic homeostasis. Accordingly, in the early phases of sepsis, tachycardia becomes a crucial mechanism for compensating the decrease in stroke volume (SV) and indicates the efficacy of baroreflex activity (1). Given the compensatory origin of such tachycardia, adequate volume resuscitation often results in a concomitant decrease in HR. In septic shock an impaired baroreflex response is often associated to the hyper-adrenergic state induced by elevated endogenous and exogenous catecholamine concentrations (2). As a consequence, a significant number of septic shock patients develop persistent tachycardia even after adequate volume expansion, and such non-compensatory tachycardia can be considered the clinical hallmark of sympathetic overstimulation (2). More importantly, such persistent elevated HR reflects a chronotropic myocardial dysfunction that may precede the decrease in contractility. To date, it is still difficult to estimate the percentage of septic shock patients remaining tachycardic after the first 24 hours, once the conventional resuscitation endpoints are achieved. Such percentage cannot be extrapolated by clinical studies as they may differ from daily clinical practice. For instance, in the ALBIOS trial—the largest trial ever performed in Italy on severe sepsis and septic shock—the mean HR after achieving hemodynamic optimization in the patients with septic shock were 104±21 and 107±21 in the two groups (albumin and crystalloids vs. crystalloids only) (3). More importantly, in the daily clinical practice patients much more often become tachycardic after 24 hours. This condition is related to the severity/progression of the underlying disease, especially in presence of increasing norepinephrine requirements. Retrospective analyses of medical records of consecutive septic shock patients can provide the exact dimensions of such subgroup of septic shock patients remaining persistently tachycardic despite resuscitation. In this regards, several research groups are now focusing their attention to this specific subgroup of patients and more data will hopefully be available in the near future.
In a proof of concept study, we showed that in presence of non-compensatory tachycardia, esmolol-induced decrease in HR was associated with improved hemodynamics (increased SV) and reductions in norepinephrine requirements (4). It is out of doubt that this improvement was related, at least in part, to enhanced diastolic function. Nevertheless, whether our findings were only the consequence of improved diastole after HR reduction remains an unsolved question. As it has been demonstrated that beta-blockers may improve ventricular-arterial coupling by decreasing arterial elastance (Ea) (mainly through a reduction in HR), we hypothesized that an improved ventricular-arterial coupling contributed to the observed increase in SV. Our more recent study (5) was therefore designed to investigate whether HR reduction with esmolol may improve myocardial performance by positively affecting the tone of arterial vessels and more importantly, their responsiveness to HR-related changes in SV.
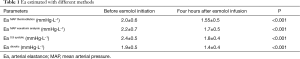
Cholley and Le Gall (6) and Mathieu et al. (7) as well as Kimmoun et al. (8) elegantly described the concept of ventriculo-arterial coupling, its pathophysiological implications and the importance of Ea as component of ventricular-arterial coupling. More importantly, they underline that Ea expresses the true afterload imposed to the left ventricle (LV) as the result of the interplays between wall stiffness, compliance and outflow resistance. Based on this assumption, Ea has therefore to be considered as a reliable estimate of arterial load. In practice, Ea quantifies the capability of the arterial vessels to increase blood pressure when SV rises. Ea is expressed by the ratio of LV end-systolic pressure (LVESP) to the SV. Nevertheless, it is difficult to obtain at the bedside a reliable value of LVESP as it requires highly invasive technique (intraventricular conductance catheter). To facilitate the assessment of Ea, mean aortic pressure (MAP) (9-11), dicrotic pressure (12-14), with systolic aortic pressures (SAP) and diastolic aortic pressures (DAP) and 0.9 • SAP formulas (15-17) have been proposed as a surrogate of LVESP. Since the superiority of one method over another in estimating LVESP has not been demonstrated both under dynamic conditions and after pharmacological interventions, in our study we decided to use MAP for calculating Ea. In this regard, it is important to highlight that the pressure recording analytic method (PRAM) measures SV, on a beat-to-beat analysis, through recognition of the resonance points, which are the result of the interactions between incident and reflected waves. Therefore, PRAM method allows to obtain SV and its relative MAP value at each single beat (MAP value generated by that single SV) and this is exactly what is needed for obtaining Ea (9-11). In fact, even by applying other pressures or formula, the consistency of response to esmolol is similar (see Table 1). We agree with Kimmoun et al. (8) and other authors (6,7) that we did not investigate ventricular elastance, the other determinant of V-A coupling (although this limitation is largely acknowledged in the manuscript). However, one should not forget that accurate measurement of ventricular elastance is extremely difficult to perform in severely critically ill patients, because of the invasiveness and the risks related to the technique (LV catheterization with high-fidelity catheters) and the need of transferring the patients in the cath-lab. Given the observational nature of our study, such invasiveness was not justified. In addition, Kimmoun et al. (8) criticized our study design. However, the study was designed as observational because our ICU guidelines now requires administration of esmolol to control the HR in such subgroup of patients, particularly as we had demonstrated previous outcome benefit. Interestingly, Kimmoun et al. (8) proposed alternate sequences of “on and off” esmolol administration. We are very surprised from this suggestion. Indeed, the severity of the clinical conditions of septic shock patients and the hemodynamic impact of alternate sequences of esmolol administration, do not warrant such approach and such design can be extremely harmful for the patients and it can be eventually applied only to experimental models. Due to the short observational period, the authors also argued that it was unlikely that anti-inflammatory activity of esmolol has contributed to decreased Ea. However, it has been shown that ultrashort acting beta-blockers may reach the peak of anti-inflammatory effects even after 3 hours (18). Of note, acute increases in HR directly affect arterial distensibility. In acute pacing study in humans, increasing HR from 63 to 110 beats/min was associated to systodiastolic diameter change and reduced radial arterial distensibility by 45% (19).
Full table
Kimmoun et al. (8) correctly analyzed the relationships between MAP, reduction in norepinephrine requirement, SV and Ea. During pharmacologically induced HR reduction, preload, ventricular filling, myocardial contractility and their relationships change accordingly. Such modifications require time before reaching a new stable hemodynamic condition. In our previous study the maximum time allowed to achieve control HR was 12 hours, and the first time-point for data collection was 24 hours after commencing esmolol (4). By contrast, in the present study we performed a fast dose titration of esmolol (5). Such study design carries the risk of worsening hemodynamic instability, leading to increased norepinephrine requirements as consequence of negative chronotropic effect and reduced myocardial contractility (high doses over a short time period). However, MAP decreased in parallel with norepinephrine dose after the reduction of HR. The MAP values and norepinephrine requirements should be analyzed in the context of the increased SV and decreased Ea seen after HR reduction. In our study, the decrease in MAP was the consequence of the achievement of a new equilibrium between contractility and arterial load, allowing the LV to generate a higher SV with less contractility. This assumption is reinforced by the fact that arterial dP/dtmax (a surrogate of LV dP/dtmax), decreased on reducing HR, while SV increased and norepinephrine requirements were reduced. The improved myocardial performance is even better described by the changes in MAP—Pdicrotic which accurately expresses the interaction between LV contractility and a given afterload. In fact, MAP—Pdicrotic decreased, indicating a more physiological cardiovascular interaction. It should be noted that MAP and Pdicrotic are directly measured variables and are not affected by confounding factors such as very precise synchronization of arterial signal and echocardiography. Therefore, how can we explain that a drug reducing contractility was associated with increased SV after decreasing the HR? In addition to improved LV filling, our results clearly indicate that a better ventricular-arterial coupling played a crucial role, as one of its component improved. The findings of our study demonstrate that HR reduction with esmolol unloads the LV, thereby improving myocardial performance. What is probably even more important is that the increase in SV after HR reduction contributed to the maintenance of cardiac output. This new hemodynamic profile after administration of esmolol should be considered as an economization of myocardial workload and oxygen consumption, which in turn may contribute to preserve myocardial performance during the course of the septic disease. There are sufficient preclinical and clinical data to suggest that beta-blockade is safe in septic shock though, obviously, it must be used carefully and once the patient has been stabilized.
What is the clinical relevance of such hemodynamic changes? Elevated HR is a risk factor for an increased mortality even in septic shock patients. Nowadays, the majority of the patients suffering from septic shock die late during the stay in the intensive care units (ICUs) (20). This delayed mortality is probably the result of a more sophisticated ICU care that keeps both elderly patients and patients with significant comorbidities alive longer. It is out of doubt that early and aggressive resuscitation according to Surviving Sepsis Campaign reduces the number of early deaths. As suggested by Daviaud et al., it is this reduction of early deaths that mainly contributes to the overall improved outcome of patients with septic shock (20). Nevertheless, in established septic shock (following hemodynamic resuscitation) esmolol administration and other therapies aiming at economizing cardiac work, decreasing cardiac energetic costs, and preserving ventricular-arterial coupling may not only improve cardiovascular efficiency but also preserve long-term myocardial performance. It is possible that such therapeutic strategies may contribute to decrease even the number of late deaths, thereby further improving patient’s outcome—a hypothesis that needs to be tested in future studies.
Acknowledgements
None.
Footnote
Provenance: This is an invited Editorial commissioned by the Section Editor Zhongheng Zhang (Department of Emergency Medicine, Sir Run-Run Shaw Hospital, Zhejiang University School of Medicine, Hangzhou, China).
Conflicts of Interest: Salvatore Mario Romano has a patent “Method and apparatus for measuring cardiac flow output” (USA Patent Number 6758822). The authors have no conflicts of interest to declare.
Comment on: Mathieu C, Zieleskiewicz L, Leone M. Betablockers in septic shock: a magnifying glass on the relation heart vessel. J Thorac Dis 2016;8:E802-E4.
Kimmoun A, Wei C, Levy B, et al. Heart rate reduction may be a major determinant of vascular tone in esmololtreated septic shock patients–although still remains to be confirmed! J Thorac Dis 2016;8:E829-32.
Cholley B, Le Gall A. Ventriculo-arterial coupling: the comeback? J Thorac Dis 2016;8:2287-9. Kim WY, Hong SB. Beta-blockers in patients with septic shock: plenty of promise, but no hard evidence yet. J Thorac Dis 2016;8:E1041-3.
References
- Lanspa MJ, Brown SM, Hirshberg EL, et al. Central venous pressure and shock index predict lack of hemodynamic response to volume expansion in septic shock: a prospective, observational study. J Crit Care 2012;27:609-15. [Crossref] [PubMed]
- Dünser MW, Hasibeder WR. Sympathetic overstimulation during critical illness: adverse effects of adrenergic stress. J Intensive Care Med 2009;24:293-316. [Crossref] [PubMed]
- Masson S, Caironi P, Fanizza C, et al. Sequential N-Terminal Pro-B-Type Natriuretic Peptide and High-Sensitivity Cardiac Troponin Measurements During Albumin Replacement in Patients With Severe Sepsis or Septic Shock. Crit Care Med 2016;44:707-16. [PubMed]
- Morelli A, Ertmer C, Westphal M, et al. Effect of heart rate control with esmolol on hemodynamic and clinical outcomes in patients with septic shock: a randomized clinical trial. JAMA 2013;310:1683-91. [Crossref] [PubMed]
- Morelli A, Singer M, Ranieri VM, et al. Heart rate reduction with esmolol is associated with improved arterial elastance in patients with septic shock: a prospective observational study. Intensive Care Med 2016;42:1528-34. [Crossref] [PubMed]
- Cholley B, Le Gall A. Ventriculo-arterial coupling: the comeback? J Thorac Dis 2016;8:2287-9. [Crossref] [PubMed]
- Mathieu C, Zieleskiewicz L, Leone M. Beta-blockers in septic shock: a magnifying glass on the relation heart vessel. J Thorac Dis 2016;8:E802-4. [Crossref] [PubMed]
- Kimmoun A, Wei C, Levy B, et al. Heart rate reduction may be a major determinant of vascular tone in esmolol-treated septic shock patients-although still remains to be confirmed! J Thorac Dis 2016;8:E829-32. [Crossref] [PubMed]
- Kadoi Y, Kawahara H, Fujita N. The end-systolic pressure- Volume relationship and ventriculoarterial coupling in patients undergoing coronary artery by pass graft surgery. Acta Anaesthesiol Scand 1998;42:369-75. [Crossref] [PubMed]
- Sunagawa K, Maughan WL, Burkhoff D, et al. Left ventricular interaction with arterial load studied in isolated canine ventricle. Am J Physiol 1983;245:H773-80. [PubMed]
- Sunagawa K, Maughan WL, Sagawa K. Optimal arterial resistance for the maximal stroke work studied in isolated canine left ventricle. Circ Res 1985;56:586-95. [Crossref] [PubMed]
- Sunagawa K, Sagawa K, Maughan WL. Ventricular interaction with the loading system. Ann Biomed Eng 1984;12:163-89. [Crossref] [PubMed]
- Asanoi H, Sasayama S, Kameyama T. Ventriculoarterial coupling in normal and failing heart in humans. Circ Res 1989;65:483-93. [Crossref] [PubMed]
- Colin P, Slama M, Vahanian A, et al. Hemodynamic correlates of effective arterial elastance in mitral stenosis before and after balloon valvotomy. J Appl Physiol (1985) 1997;83:1083-9. [PubMed]
- Kelly R, Karamanoglu M, Gibbs H, et al. Noninvasive carotid pressure wave registration as an indicator of ascending aortic pressure. J Vasc Med Biol 1989;1:241-7.
- Kelly RP, Ting CT, Yang TM, et al. Effective arterial elastance as index of arterial vascular load in humans. Circulation 1992;86:513-21. [Crossref] [PubMed]
- Chen CH, Nakayama M, Talbot M, et al. Verapamil acutely reduces ventricular-vascular stiffening and improves aerobic exercise performance in elderly individuals. J Am Coll Cardiol 1999;33:1602-9. [Crossref] [PubMed]
- Hagiwara S, Iwasaka H, Maeda H, et al. Landiolol, an ultrashort-acting beta1-adrenoceptor antagonist, has protective effects in an LPS-induced systemic inflammation model. Shock 2009;31:515-20. [Crossref] [PubMed]
- Giannattasio C, Vincenti A, Failla M, et al. Effects of heart rate changes on arterial distensibility in humans. Hypertension 2003;42:253-6. [Crossref] [PubMed]
- Daviaud F, Grimaldi D, Dechartres A, et al. Timing and causes of death in septic shock. Ann Intensive Care 2015;5:16. [Crossref] [PubMed]


