To complete, or not to complete, that is the question of revascularization in percutaneous coronary intervention with drug-eluting stents for multivessel disease
In patients with multivessel (MV) coronary artery disease (CAD) (MV-CAD) except for acute myocardial infarction (acute MI, AMI) [including acute ST-segment elevation MI (STEMI)], the clinical impact of completeness of revascularization (RV) in percutaneous coronary intervention (PCI) with drug-eluting stents (DES) (DES-PCI) on major adverse cardiac (and cerebrovascular) events [MAC(C)E] remains unclear. Recently, Chang et al. (1) compared the outcomes in patients with MV-CAD achieving complete versus incomplete RV (C-RV vs. IC-RV) at the time of PCI. This analysis included consecutive 3,901 patients with MV-CAD undergoing DES-PCI, and the primary and secondary outcomes were all-cause death; and the rates of MI, stroke, and repeat RV (R-RV), respectively. Propensity-score matching was used, and 1,402 pairs of similar baseline characteristics in each group of C-RV and IC-RV were identified. As compared with C-RV at a median follow-up of 4.9 (interquartile range, 2.4 to 7.5) years, IC-RV was associated with similar risks of all-cause death [hazard ratio (HR), 1.03; 95% confidence interval (CI), 0.80 to 1.32; P=0.83], stroke (HR, 1.26; 95% CI, 0.76 to 2.09; P=0.37), and R-RV (HR, 1.15; 95% CI, 0.93 to 1.41; P=0.19); but a higher risk of MI (HR, 1.86; 95% CI, 1.08 to 3.19; P=0.024). As compared with C-RV in patients with MV-CAD (except for STEMI) treated with DES-PCI, the authors (1) concluded that IC-RV was associated with a similar risk of all-cause death but a higher risk of MI during follow-up.
A number of meta-analyses (2-4) have been performed to focus C-RV versus IC-RV in PCI or coronary artery bypass grafting (CABG) in patients with MVD (except for AMI). In unrestricted PCI, the first meta-analysis by Garcia et al. (2) of 35 studies including 89,883 patients with 4.6±4 years follow-up showed that C-RV was associated with lower all-cause death [risk ratio (RR), 0.73; 95% CI, 0.65 to 0.82; P<0.001], MI (RR, 0.80; 95% CI, 0.71 to 0.91; P=0.001), and R-RV (RR, 0.72; 95% CI, 0.63 to 0.81; P<0.001) relative to IC-R. In unlimited CABG, however, C-RV was associated with lower all-cause death (RR 0.70; 95% CI, 0.62 to 0.80; P<0.001); but with neither MI (RR, 0.69, 95% CI, 0.44 to 1.10; P=0.12) nor R-RV (RR, 0.92; 95% CI, 0.67 to 1.28; P=0.64) (2). In PCI with stents (including not only DES but also bare-metal stents), a recent meta-analysis by Zimarino et al. (3) of 28 studies including 83,695 patients with 4.7±4.3 years follow-up confirmed that C-RV conferred clinical benefits in all-cause death (RR, 0.73; 95% CI, 0.64 to 0.82), MI (RR, 0.69; 95% CI, 0.59 to 0.82), and R-RV (RR, 0.74; 95% CI, 0.63 to 0.86) as compared with IC-R. In CABG with arterial graft(s) in ≥80% of cases, however, C-RV was associated with reduced all-cause death (RR, 0.76; 95% CI, 0.63 to 0.90); but with neither MI (RR, 0.89; 95% CI, 0.67 to 1.18) nor R-RV (RR, 0.94; 95% CI, 0.65 to 1.36) (3). Another recent meta-analysis (4) of exclusive adjusted-risk estimates from 14 studies enrolling 30,389 patients demonstrated a statistically significant reduction in follow-up mortality with C-RV relative to IC-RV CABG (HR, 0.63; 95% CI, 0.53 to 0.75; P<0.00001).
For MV-CAD (except for AMI), despite evidence from the meta-analyses (2-4) regarding impacts of C-RV versus IC-RV in PCI (including DES-PCI) and CABG, findings concerning effects of RV completeness in exclusive DES-PCI are limited. Our systematic search using keywords including “complete” or “completeness”; “incomplete” or “culprit”; “revascularization”; and “drug-eluting” identified 14 studies (1,5-17) summarized in Tables 1,2. The design of all studies was a non-randomized observational study, and all but one (13) studies reported adjusted HRs for outcomes of interest in “C-RV vs. IC-RV” or “IC-RV vs. C-RV”. Nine (1,5-7,9,11,13-15), 5 (6,8,9,16,17), 3 (1,6,11), 2 (1,6), 5 (1,6,11,13,16), and 11 studies (1,6,8-16) provided HRs for all-cause death, cardiac death, MI, stroke, R-RV, and MAC(C)E, respectively. In 5 (5-7,14,15) of the 9 studies, C-RV was associated with reduced all-cause death. In all but one (9) of the 5 studies, C-RV was associated with reduced cardiac death. In one (1) of the 3 studies, C-RV was associated with reduced MI. Only two studies (1,6) reported no association of C-RV with stroke. In 3 (11,13,16) of the 5 studies, C-RV was associated with reduced R-RV. In 8 (6,9-11,13-16) of the 11 studies, C-RV was associated with reduced MAC(C)E.
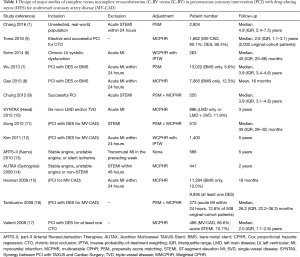
Full table
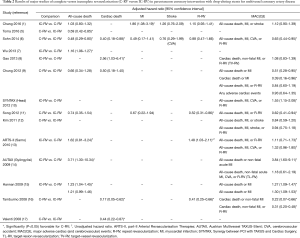
Full table
There were a number of important issues, however, in the aforementioned studies (1,5-17) of C-RV versus IC-RV in DES-PCI for MV-CAD (except for AMI) (Figure 1). First, “angiographic” (successful angioplasty of all diseased lesions in the major epicardial coronary vessels and their first degree side branches) and “proximal” C-RV definitions (successful angioplasty of all diseased proximal arteries) according to a study by Kim et al. (18) are more accurate and clinically relevant. In a study by Gao et al. (8), although angiographic IC-RV (not meeting the definition of angiographic C-RV) was associated with a higher rate of cardiac death (P=0.04), proximal IC-RV (not meeting the definition of proximal C-RV) was not (P=0.08).
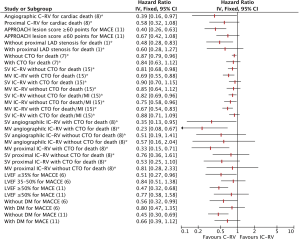
Second, although the angiographic Synergy between PCI with Taxus and Cardiac Surgery (SYNTAX) score (19) is used to assess the complexity of CAD, the Alberta Provincial Project for Outcome Assessment in Coronary Heart Disease (APPROACH) lesion score (20) is calculated to assess the amount of myocardium at risk. In a study by Song et al. (11), the incidence of MACE was significantly lower in the C-RV group than in the IC-RV group for patients with an APPROACH lesion score ≥60 points (HR for C-RV vs. IC-RV, 0.41; 95% CI, 0.26 to 0.63); but not for those with that <60 points (HR, 0.67; 95% CI, 0.42 to 1.08).
Third, the impact of the completeness of PCI may be based on presence of proximal left anterior descending artery (LAD) stenosis. In the study by Chang et al. (1), the group without proximal LAD stenosis suggests better survival with C-RV (HR for IC-RV versus C-RV, 2.08; 95% CI, 1.20 to 3.59) than that with proximal LAD stenosis (HR, 1.66; 95% CI, 0.79 to 3.51) (1). Also in a study by Wu et al. (7), IC-RV was associated with significantly greater risk of death than C-RV in the group without proximal LAD stenosis (P=0.003); but not in that with proximal LAD stenosis (P=0.30).
Fourth, persistent chronic total occlusion (CTO) lesions are associated with significantly worse survival than persistent non-occlusive coronary lesions. Within the group of IC-RV in a study by Toma et al. (5), mortality differed significantly depending on whether the IC-RV involved CTO (HR for IC-RV with succeed versus failed CTO, 0.67; 95% CI, 0.50 to 0.92; P=0.012). Whereas, in the study by Wu et al. (7), IC-RV was associated with significantly greater risk of death than C-RV in the group without CTO (P=0.004); but not in that with CTO (P=0.24).
Fifth, IC-RV may sometimes be justified in patients with CTO (in danger of having worse longer-term outcomes) when there is no viable myocardium to be preserved. In a study by Hannan et al. (15), IC-RV was associated with significantly higher mortality in patients with single-vessel (SV) IC-RV without CTO (P=0.03) and those with MV IC-RV with CTO (P=0.002); but in neither those with SV IC-RV with CTO (P=0.39) nor those with MV IC-RV without CTO (P=0.26). IC-RV was also associated with significantly higher mortality/MI rates in patients with SV IC-RV without CTO (P=0.02), those with MV IC-RV without CTO (P=0.03), and those with MV IC-RV with CTO (P<0.001); but not in those with SV IC-RV with CTO (P=0.24). These results suggest that although the benefit of C-RV is highest for patients with MV IC-RV and CTO, those with SV IC-RV and no CTO have significantly higher mortality and mortality/MI than C-RV patients do, and those with MV IC-RV and no CTO have significantly higher mortality/MI than C-RV ones do (18). Meanwhile, in the study by Gao et al. (8), angiographic IC-RV patients had significantly higher rates of cardiac death for SV IC-RV with CTO (P=0.04) and MV IC-RV with CTO (P=0.007); but for neither SV IC-RV without CTO (P=0.20) nor MV IC-RV without CTO (P=0.38). Whereas, proximal IC-RV was associated with significantly higher rates of cardiac death only for MV IC-RV with CTO (P=0.005); but not for SV IC-RV without CTO (P=0.47), SV IC-RV with CTO (P=0.09), and MV IC-RV without CTO (P=0.70) (8).
Sixth, improvement of left ventricular (LV) ejection fraction (LVEF) by reduction of ischemic burden after C-RV could possibly contribute to the decline of mortality in long-term follow up. In a study by Sohn et al. (6), although the rate of MACCE for patients with LVEF <35% was significantly lower in the C-RV group (HR, 0.51; 95% CI, 0.27 to 0.96), that for those with LVEF ≥35% (and <50% of inclusion criteria) was not (HR, 0.84; 95% CI, 0.51 to 1.38). Meanwhile, in the study by Song et al. (11), the incidence of MACE was significantly lower in the C-RV group than in the IC-RV group for patients with LVEF ≥50% (HR for C-RV versus IC-RV, 0.47; 95% CI, 0.32 to 0.68); but not for those with LVEF <50% (HR, 0.77; 95% CI, 0.38 to 1.58). Silent ischemia might mask the need for RV in ischemia-driven PCI, which is a possible explanation for the attenuation of the C-RV effect in patients with LV dysfunction.
Last, diabetes mellitus (DM) is an independent predictor of target-vessel RV after DES-PCI (21), which may attenuate the benefit of C-RV. In the study by Sohn et al. (6), although the rate of MACCE for patients without DM was significantly lower in the C-RV group (HR for C-RV vs. IC-RV, 0.56; 95% CI, 0.32 to 0.99), that for those with DM was not (HR, 0.80; 95% CI, 0.47 to 1.35). Also in the study by Song et al. (11), the incidence of MACE was significantly lower in the C-RV group than in the IC-RV group for patients without DM (HR for C-RV vs. IC-RV, 0.46; 95% CI, 0.30 to 0.69); but not for those with DM (HR, 0.66; 95% CI, 0.39 to 1.12).
To investigate aforementioned important issues, further studies of C-RV versus IC-RV in DES-PCI for MV-CAD (except for AMI) should be required. Furthermore, to determine whether C-RV is associated with reduced all-cause death, cardiac death, MI, stroke, R-RV, or MAC(C)E, a meta-analysis of currently available studies would be performed.
Acknowledgements
None.
Footnote
Provenance: This is an invited Editorial commissioned by the Section Editor Yue Liu (Associate professor, Department of Cardiology, The First Affiliated Hospital of Harbin Medical University, Harbin, China).
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Chang M, Ahn JM, Kim N, et al. Complete versus incomplete revascularization in patients with multivessel coronary artery disease treated with drug-eluting stents. Am Heart J 2016;179:157-65. [Crossref] [PubMed]
- Garcia S, Sandoval Y, Roukoz H, et al. Outcomes after complete versus incomplete revascularization of patients with multivessel coronary artery disease: a meta-analysis of 89,883 patients enrolled in randomized clinical trials and observational studies. J Am Coll Cardiol 2013;62:1421-31. [Crossref] [PubMed]
- Zimarino M, Ricci F, Romanello M, et al. Complete myocardial revascularization confers a larger clinical benefit when performed with state-of-the-art techniques in high-risk patients with multivessel coronary artery disease: A meta-analysis of randomized and observational studies. Catheter Cardiovasc Interv 2016;87:3-12. [Crossref] [PubMed]
- Takagi H, Watanabe T, Mizuno Y, et al. A meta-analysis of adjusted risk estimates for survival from observational studies of complete versus incomplete revascularization in patients with multivessel disease undergoing coronary artery bypass grafting. Interact Cardiovasc Thorac Surg 2014;18:679-82. [Crossref] [PubMed]
- Toma A, Gick M, Minners J, et al. Survival after percutaneous coronary intervention for chronic total occlusion. Clin Res Cardiol 2016;105:921-9. [Crossref] [PubMed]
- Sohn GH, Yang JH, Choi SH, et al. Long-term outcomes of complete versus incomplete revascularization for patients with multivessel coronary artery disease and left ventricular systolic dysfunction in drug-eluting stent era. J Korean Med Sci 2014;29:1501-6. [Crossref] [PubMed]
- Wu C, Dyer AM, Walford G, et al. Incomplete revascularization is associated with greater risk of long-term mortality after stenting in the era of first generation drug-eluting stents. Am J Cardiol 2013;112:775-81. [Crossref] [PubMed]
- Gao Z, Xu B, Yang YJ, et al. Long-term outcomes of complete versus incomplete revascularization after drug-eluting stent implantation in patients with multivessel coronary disease. Catheter Cardiovasc Interv 2013;82:343-9. [Crossref] [PubMed]
- Chung JW, Park KH, Lee MH, et al. Benefit of complete revascularization in patients with multivessel coronary disease in the drug-eluting stent era. Circ J 2012;76:1624-30. [Crossref] [PubMed]
- Head SJ, Mack MJ, Holmes DR Jr, et al. Incidence, predictors and outcomes of incomplete revascularization after percutaneous coronary intervention and coronary artery bypass grafting: a subgroup analysis of 3-year SYNTAX data. Eur J Cardiothorac Surg 2012;41:535-41. [Crossref] [PubMed]
- Song YB, Lee SY, Hahn JY, et al. Complete versus incomplete revascularization for treatment of multivessel coronary artery disease in the drug-eluting stent era. Heart Vessels 2012;27:433-42. [Crossref] [PubMed]
- Kim YH, Park DW, Lee JY, et al. Impact of angiographic complete revascularization after drug-eluting stent implantation or coronary artery bypass graft surgery for multivessel coronary artery disease. Circulation 2011;123:2373-81. [Crossref] [PubMed]
- Sarno G, Garg S, Onuma Y, et al. Impact of completeness of revascularization on the five-year outcome in percutaneous coronary intervention and coronary artery bypass graft patients (from the ARTS-II study). Am J Cardiol 2010;106:1369-75. [Crossref] [PubMed]
- Gyöngyösi M, Christ G, Lang I, et al. 2-year results of the AUTAX (Austrian Multivessel TAXUS-Stent) registry beyond the SYNTAX (synergy between percutaneous coronary intervention with TAXUS and cardiac surgery) study. JACC Cardiovasc Interv 2009;2:718-27. [Crossref] [PubMed]
- Hannan EL, Wu C, Walford G, et al. Incomplete revascularization in the era of drug-eluting stents: impact on adverse outcomes. JACC Cardiovasc Interv 2009;2:17-25. [Crossref] [PubMed]
- Tamburino C, Angiolillo DJ, Capranzano P, et al. Complete versus incomplete revascularization in patients with multivessel disease undergoing percutaneous coronary intervention with drug-eluting stents. Catheter Cardiovasc Interv 2008;72:448-56. [Crossref] [PubMed]
- Valenti R, Migliorini A, Signorini U, et al. Impact of complete revascularization with percutaneous coronary intervention on survival in patients with at least one chronic total occlusion. Eur Heart J 2008;29:2336-42. [Crossref] [PubMed]
- Kim YH, Park DW, Lee JY, et al. Impact of angiographic complete revascularization after drug-eluting stent implantation or coronary artery bypass graft surgery for multivessel coronary artery disease. Circulation 2011;123:2373-81. [Crossref] [PubMed]
- Serruys PW, Morice MC, Kappetein AP, et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med 2009;360:961-72. [Crossref] [PubMed]
- Graham MM, Faris PD, Ghali WA, et al. Validation of three myocardial jeopardy scores in a population-based cardiac catheterization cohort. Am Heart J 2001;142:254-61. [Crossref] [PubMed]
- Marzocchi A, Saia F, Piovaccari G, et al. Long-term safety and efficacy of drug-eluting stents: two-year results of the REAL (REgistro AngiopLastiche dell'Emilia Romagna) multicenter registry. Circulation 2007;115:3181-8. [Crossref] [PubMed]


