Thoracoscopic esophageal repair with barbed suture material in a case of Boerhaave’s syndrome
Introduction
Spontaneous esophageal rupture was first reported by Boerhaave in 1724 and typically occurs in conjunction with vomiting, retching, or swallowing a large food bolus. This condition is potentially life threatening and causes severe mediastinitis, empyema, and sepsis, unless appropriate and early treatment is initiated (1). Surgical results for the treatment of this condition with thoracoscopic surgery are similar to those with conventional thoracotomy (2,3). Patients are usually operated in the lateral decubitus position for thoracoscopy as well as for open thoracotomy, which only provides limited access to the esophagus. Thoracoscopic suturing of esophagus requires advanced expertise, irrespective of whether an intracorporeal hand-sewn technique or an extracorporeal technique is used. Recent report suggests that laparoscopic gastrojejunostomy can be performed safely and efficiently by using barbed suture material (4). Herein, we report the first successful case of thoracoscopic repair of a spontaneous rupture of the esophagus by using barbed suture material.
Case presentation
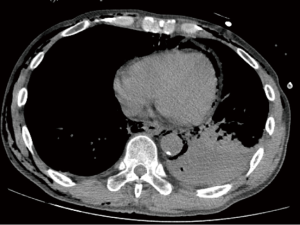
A 53-year-old man was admitted to a local hospital with complaints of violent vomiting and hematemesis following excessive alcohol consumption. Upper gastrointestinal endoscopy, performed with the suspicion of Mallory-Weiss syndrome, revealed a perforation on the left side of his lower esophagus. Patient then sustained a cardiopulmonary arrest secondary to tension pneumothorax. He was transferred to our hospital after resuscitation and insertion of a thoracic drain. Urgent computed tomography (CT) of the chest revealed pneumomediastinum, left pneumothorax, and left pleural empyema (Figure 1). The findings on computed tomography and upper gastrointestinal endoscopy confirmed the diagnosis of Boerhaave’s syndrome, without the need for a contrast study. At admission in our hospital, the patient was conscious, with a blood pressure of 115/82 mmHg and heart rate of 127 bpm. Laboratory tests revealed a hemoglobin concentration of 12.2 g/dL, white blood cell count of 3,400/mm3, and C-reactive protein level of 28.7 mg/dL. Arterial blood gas analysis at inspired oxygen flows of 3.0 L/min revealed the following results: pH, 7.503; oxygen tension, 81.2 mmHg; and carbon dioxide tension, 32.4 mmHg. A thoracoscopic operation was performed 30 h after the onset of his symptoms.
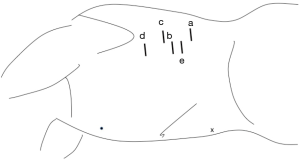
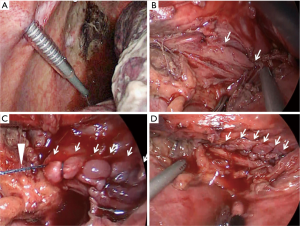
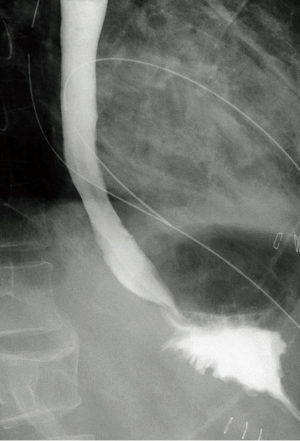
The patient was placed in the right semi-prone position (Figure 2), and carbon dioxide pneumothorax was created at a pressure of 6 to 8 mmHg. Port placement included a 12-mm port in the 9th intercostal space along the posterior axillary line (video camera), a 12-mm port in the 7th intercostal space along the middle axillary line (operator’s use), a 5-mm port each in the 5th intercostal space along the middle axillary line, and 6th intercostal space along the posterior axillary line (grasping forceps), and a 12-mm port in the 8th intercostal space along the middle axillary line (assistant’s use) (Figure 2). The mediastinum was widely incised, and copiously irrigated with physiological saline. In the semi-prone position, the irrigation fluid accumulates anteriorly, enabling effective suctioning (Figure 3A). The esophagus was exposed and a 4-cm longitudinal perforation was identified on the left side of the lower esophagus (Figure 3B). The esophageal tear was repaired in 2 layers, mucosal and muscularis, by using barbed absorbable suture material (V-Loc™180, VLOCL0804, Medtronics, Minneapolis, USA) (Figure 3C,D). Intraoperative esophageal endoscopy, and subsequent air insufflation confirmed the integrity of the esophageal repair. The chest wall was closed after inserting three catheters to drain the chest. Of the total time taken for the procedure of 245 min, only 32 min were taken to complete suture repair of the esophagus by using barbed suture material. Patient recovered well, and was shifted out of the intensive care unit three days after the operation. Oral feeds were started on the postoperative day 7 after upper gastrointestinal endoscopy and barium swallow confirmed the absence of any leak or stenosis at site of the esophageal repair (Figure 4). The empyema caused by the esophageal perforation responded well to intra-operative lavage, and the catheters draining the chest were removed by postoperative day 21. The patient was discharged from the hospital on postoperative day 28, and followed up in the outpatient clinic of the local hospital for 2 months. He did not require further re-hospitalization in the course of his recovery.
Discussion
Spontaneous perforation of the esophagus (Boerhaave’s syndrome) is a life-threatening condition. Early diagnosis and appropriate treatment are necessary to prevent sepsis and lethal outcomes. Diagnostic upper gastrointestinal endoscopy, following a clinical diagnosis of Mallory-Weiss syndrome at another hospital, resulted in the patient developing tension pneumothorax and sustaining a cardiopulmonary arrest. There are other reports, of unusual presentations of Boerhaave’s syndrome, and upper gastrointestinal endoscopy therein resulting in respiratory distress secondary to pneumothorax (5). It is important to consider Boerhaave’s syndrome in the differential diagnosis of patients presenting with hematemesis, or suspected Mallory-Weiss syndrome.
Although there are successful reports that endoscopic clipping closure and stenting was undergone for patients with Boerhaave’s syndrome (6,7), the standard recommendation for this disease is to consider surgery within 24 h of onset (8-11).
Tissue necrosis and edema following delay in management may prevent successful primary repair of the esophageal tear. However, successful primary repair of the esophagus in the presence of significant fibrosis has been reported in a case of perforated Barrett’s ulcer (12). Several recent reports recommend surgery, regardless of the delay in presentation (13,14). Studies also suggest similar clinical outcomes between thoracoscopic repair and repair with open thoracotomy, for esophageal rupture in patients with Boerhaave’s syndrome (2). Minimally invasive thoracoscopic techniques may be associated with lesser surgical stress while allowing wide mediastinal drainage and adequate esophageal repair (2,15). Thoracoscopic suturing of esophageal tears using by conventional surgical instruments is difficult due to the awkward angle between the esophagus and the shaft of the forceps (12). In addition, both intracorporeal and extracorporeal knotting requires advanced thoracoscopic skills. Suturing devices such as Endo Stitch (Medtronics, Minneapolis, USA), or SILS Stitch (Medtronics, Minneapolis, USA), which are routinely used in gynecological and urological surgery, have also been successfully used for esophageal suturing (12). While these devices simplify thoracoscopic placement of sutures, knot-formation continues to remain challenging. Against this background, the use of barbed suture material in gastrointestinal surgery eliminates the need to form knots while performing minimally invasive surgery. Studies have confirmed that barbed suture material is similar to conventional monofilament in safety and efficacy, and enables simpler and quicker suturing while performing laparoscopic gastrointestinal anastomosis (4,16-18). We reinforce the suture line by using fibrin glue (19), and ensure that the cut-end of the barbed thread does not come in to direct contact with the lung.
Since the esophageal perforation is located deep in the thoracic cavity, and access to it is narrow (12), it is difficult to adequately retract the lung and maintain a clear operative view, with the patient in the lateral position. This limitation was recognized in performing esophagectomy, and overcome by changing the patient position to prone. Minimally invasive esophagectomy in the prone position is associated with improved patient outcomes, and fewer complications such as pneumonia (20,21). In this position, the lungs are naturally retracted from the operative field owing to the effect of gravity and carbon dioxide pneumothorax. The operative space is considered adequate in prone position, even without the use of one-lung ventilation (22). However, we anticipated the need for conversion to the conventional lateral decubitus position or open thoracotomy while operating on the present case. To achieve this, we modified our approach in two ways. One, a double lumen endotracheal tube was used for one-lung ventilation. Two, a semi-prone position was used, instead of prone, as it enables easier positional change to the lateral position, while retaining the benefits of the fully prone position (23,24). In the semi-prone position, similar to the fully prone position, most of the exudate or irrigant accumulates in the anterior chest cavity, away from the site of the esophageal perforation. This enabled meticulous irrigation of the thoracic cavity, and the food debris, and necrotic material could be effectively removed. The semi-prone position also allowed good access to the posterior mediastinum to accomplish the esophageal repair.
Conclusions
Our case report, of a patient with Boerhaave’s syndrome, demonstrates successful esophageal repair by using barbed absorbable suture material, and highlights the safety and simplicity of this technique. It also demonstrates the advantages of pneumothorax and semi-prone position in gaining thoracoscopic access to the esophagus.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Chang CH, Lin PJ, Chang JP, et al. One-stage operation for treatment after delayed diagnosis of thoracic esophageal perforation. Ann Thorac Surg 1992;53:617-20. [Crossref] [PubMed]
- Cho JS, Kim YD, Kim JW, et al. Thoracoscopic primary esophageal repair in patients with Boerhaave's syndrome. Ann Thorac Surg 2011;91:1552-5. [Crossref] [PubMed]
- Haveman JW, Nieuwenhuijs VB, Kobold JP, et al. Adequate debridement and drainage of the mediastinum using open thoracotomy or video-assisted thoracoscopic surgery for Boerhaave's syndrome. Surg Endosc 2011;25:2492-7. [Crossref] [PubMed]
- Costantino F, Dente M, Perrin P, et al. Barbed unidirectional V-Loc 180 suture in laparoscopic Roux-en-Y gastric bypass: a study comparing unidirectional barbed monofilament and multifilament absorbable suture. Surg Endosc 2013;27:3846-51. [Crossref] [PubMed]
- O'Kelly F, Lim KT, Cooke F, et al. An unusual presentation of Boerhaave Syndrome: a case report. Cases J 2009;2:8000. [Crossref] [PubMed]
- Ota K, Takeuchi T, Higuchi K. Temporary insertion of a covered self-expandable metal stent for spontaneous esophageal rupture. Dig Endosc 2014;26:607-8. [Crossref] [PubMed]
- Van Weyenberg SJ, Stam FJ, Marsman W. Successful endoscopic closure of spontaneous esophageal rupture (Boerhaave syndrome). Gastrointest Endosc 2014;80:162. [Crossref] [PubMed]
- Jones WG 2nd, Ginsberg RJ. Esophageal perforation: a continuing challenge. Ann Thorac Surg 1992;53:534-43. [Crossref] [PubMed]
- Okten I, Cangir AK, Ozdemir N, et al. Management of esophageal perforation. Surg Today 2001;31:36-9. [Crossref] [PubMed]
- Whyte RI. Boerhaave's syndrome. N Engl J Med 2001;344:139. [PubMed]
- Wright CD, Mathisen DJ, Wain JC, et al. Reinforced primary repair of thoracic esophageal perforation. Ann Thorac Surg 1995;60:245-8; discussion 248-9. [Crossref] [PubMed]
- Volders JH, Witteman B, Mulder AH, et al. Right hemothorax: An unusual presentation of a Barrett's ulcer perforation. Int J Surg Case Rep 2013;4:375-7. [Crossref] [PubMed]
- Cho S, Jheon S, Ryu KM, et al. Primary esophageal repair in Boerhaave's syndrome. Dis Esophagus 2008;21:660-3. [Crossref] [PubMed]
- Jougon J, Mc Bride T, Delcambre F, et al. Primary esophageal repair for Boerhaave's syndrome whatever the free interval between perforation and treatment. Eur J Cardiothorac Surg 2004;25:475-9. [Crossref] [PubMed]
- Ikeda Y, Niimi M, Sasaki Y, et al. Thoracoscopic repair of a spontaneous perforation of the esophagus with the endoscopic suturing device. J Thorac Cardiovasc Surg. 2001;121:178-9. [Crossref] [PubMed]
- De Blasi V, Facy O, Goergen M, et al. Barbed versus usual suture for closure of the gastrojejunal anastomosis in laparoscopic gastric bypass: a comparative trial. Obes Surg 2013;23:60-3. [Crossref] [PubMed]
- Facy O, De Blasi V, Goergen M, et al. Laparoscopic gastrointestinal anastomoses using knotless barbed sutures are safe and reproducible: a single-center experience with 201 patients. Surg Endosc 2013;27:3841-5. [Crossref] [PubMed]
- Blanc P, Lointier P, Breton C, et al. The Hand-sewn Anastomosis with an Absorbable Bidirectional Monofilament Barbed Suture Stratafix® During Laparoscopic One Anastomosis Loop Gastric Bypass. Retrospective Study in 50 Patients. Obes Surg 2015;25:2457-60. [Crossref] [PubMed]
- Sulpice L, Dileon S, Rayar M, et al. Conservative surgical management of Boerhaave's syndrome: experience of two tertiary referral centers. Int J Surg 2013;11:64-7. [Crossref] [PubMed]
- Biere SS, van Berge Henegouwen MI, Maas KW, et al. Minimally invasive versus open oesophagectomy for patients with oesophageal cancer: a multicentre, open-label, randomised controlled trial. Lancet 2012;379:1887-92. [Crossref] [PubMed]
- Teshima J, Miyata G, Kamei T, et al. Comparison of short-term outcomes between prone and lateral decubitus positions for thoracoscopic esophagectomy. Surg Endosc 2015;29:2756-62. [Crossref] [PubMed]
- Noshiro H, Miyake S. Thoracoscopic esophagectomy using prone positioning. Ann Thorac Cardiovasc Surg 2013;19:399-408. [Crossref] [PubMed]
- Li X, Lai FC, Qiu ML, et al. Minimally Invasive Esophagectomy in the Lateral-prone Position: Experience of 226 Cases. Surg Laparosc Endosc Percutan Tech 2016;26:60-5. [Crossref] [PubMed]
- Lin J, Kang M, Chen C, et al. Thoracoscopic oesophageal mobilization during thoracolaparoscopy three-stage oesophagectomy: a comparison of lateral decubitus versus semiprone positions. Interact Cardiovasc Thorac Surg 2013;17:829-34. [Crossref] [PubMed]


