Effect of gender on perioperative outcomes after robotic-assisted pulmonary lobectomy
Introduction
Primary lung cancer remains the leading cause of cancer-related deaths in the United States, causing 28% and 26% of all cancer deaths in men and women, respectively, and results in more deaths than breast, prostate, and colorectal cancers combined (1). An exponential increase in lung cancer was observed in the early 1970’s due to the smoking habits of previous decades (2). However, due to different smoking behaviors among women, their peak incidence of lung cancer occurred later and at a lower level, and death rates are unlikely to equal that for male smokers as more men continue to smoke (3).
Gender has been shown to be an independent risk factor for and to affect prognosis and the histology of lung cancer (4-6). Women are more likely to develop adenocarcinoma, which has been partly attributed to a greater rate of mutations in the epidermal growth factor receptor (EGFR) gene, which codes for a tyrosine kinase that regulates cell proliferation and apoptosis, and which suggests that there may be a gender-related response to treatment as well (7). Recently, female gender has also been identified as a predictive factor for mediastinal lymph node (LN) involvement in primary lung cancers (8). A recently published video-assisted thoracoscopic (VATS) surgery experience shows that significantly more patients with advanced age, male sex, hypertension, ischemic heart disease, chronic pulmonary disease, and a smoking history had respiratory complications following lung resection (9). On the other hand, women experience adverse events from smoking and diabetes, including stroke and heart disease, at greater rates than men (10-13).
The daVinci® robotic surgical system (Intuitive Surgical Corp., Sunnyvale, CA, USA) provides robotic-assisted video-thoracoscopic (RAVT) surgery several advantages over conventional VATS surgery, including improved visualization with 3-dimensional imaging, increased dexterity, absence of physiologic tremor, scaled-down motions, and ergonomic positioning (14). Its disadvantages include lack of tactile feedback, expensive equipment and maintenance, and lack of proven benefit over conventional VATS.
Over 600 studies have been published addressing use of robotics in cardiothoracic surgery. However, no studies have addressed effects of gender on outcomes and complications following RAVT pulmonary lobectomy. Our research will attempt to address these disparities.
Methods
We retrospectively studied 282 consecutive patients who underwent robotic-assisted pulmonary lobectomy by one surgeon from September 2010 through January 2015 at a single institution. This study was performed through a database protocol that was approved by our institution’s Scientific Review Committee (MCC #16512) and our university’s Institutional Review Board (IRB #Pro00002678), which waived informed consent for this retrospective study, which is considered as review of existing data. Nevertheless, all of our patients gave informed consent for fiberoptic bronchoscopy, RAVT wedge resection and/or RAVT (completion) lobectomy, mediastinal lymph node dissection (MLND), and possible thoracotomy. Patients with clinical chest wall invasion by tumor also gave informed consent for en bloc chest wall resection and possible reconstruction at the time of their lobectomy.
All our patients underwent fiberoptic bronchoscopy by the operating surgeon after the induction of general anesthesia. After placement of the dual-lumen endotracheal tube, the patient is then placed in either right or left lateral decubitus position. Our robotic-assisted lobectomy technique utilizes a three-port system, which includes a 4-cm camera port along the 6th intercostal space (ICS) at the anterior axillary line, which doubles as the assistant’s access port, and two 1-cm instrument ports along the 3rd ICS at the anterior axillary line and along the 9th ICS at the posterior axillary line.
From September 2010 through December 2011, our group used the da Vinci® “S”™ robotic surgical system, with the “Si”™ system being used from January 2012 to the present. Lobectomy is performed with the pulmonary vein divided first, then division of the pulmonary artery branch(es) and bronchus, and then completion of the pulmonary fissures. After delivery of the lobectomy within an endopouch through the 6th ICS port incision, robotic-assisted complete MLND is then performed. At the end of the procedure, a 32-French chest tube is introduced through the 9th ICS port incision and connected to drainage at −20 cmH2O continuous suction.
Of 287 consecutive patients over this 53-month period, four required completion pneumonectomy and one was performed in combination with an Ivor Lewis esophagectomy, all five of whom were excluded from the study. Our remaining cohort of 282 patients included all pathologies reported for our lobectomies, including non-small cell lung cancer (NSCLC), early-stage small cell lung cancer (SCLC), pulmonary metastases, and benign tumors that required lobectomy due to size and central location. For NSCLC, we included early-stage (I and II) NSCLC, resectable stage-IIIA NSCLC with or without induction chemotherapy +/–radiation therapy, and resectable stage-IV NSCLC with isolated brain metastases.
Patients who only underwent sublobar resection, such as wedge resection or segmentectomy without lobectomy or who required pneumonectomy, were excluded from this study. Patients who underwent lobectomy by other surgical approaches, such as conventional VATS or thoracotomy (other than after conversion from robotic-assisted approach), were also excluded from our cohort.
We investigated differences in surgical outcomes between male and female patients by measuring variables, such as operative time, estimated blood loss (EBL), chest tube duration, hospital length of stay (LOS), conversion to open lobectomy, perioperative complications, and in-hospital mortality. Any clinically significant intraoperative complications were noted and compared between male and female patients, including bleeding from major pulmonary vessels, phrenic or recurrent laryngeal nerve injury, bronchial injury, or diaphragm injury. Clinically significant postoperative complications were also recorded and compared, including pulmonary-related complications such as pulmonary embolism, respiratory failure, and hemothorax requiring intervention, as well as cardiac complications including atrial fibrillation and myocardial infarction.
Past medical history and smoking history were obtained from the preoperative history and physical examination. We defined current smokers as smokers that still smoked or had quit within 3 months prior to surgery. Former smokers include those patients that quit smoking for at least 3 months before surgery.
Extensive literature reviews were then performed on gender differences in surgical outcomes after conventional VATS or thoracotomy. Due to lack of available data about differences in complication profiles between men and women after RAVT lobectomy, our paper will attempt to address these endpoints.
All statistical analyses were performed using IBM SPSS version 22.0. Mean, median, standard error of the mean (SEM), and range were used to report continuous and ordinal variables. Number counts and percentages were used for categorical variables. Chi-square (χ2), Fisher’s exact test, Analysis of Variance (ANOVA), Student’s t-test, and Kruskal-Wallis or Mood’s median test were used to compare variables mentioned above. Statistical significance was established at P≤0.05.
Multivariable logistic regression analyses were then performed incorporating age, body surface area (BSA), co-morbidity (coronary artery disease or diabetes mellitus), smoking history, FEV1, DLCO, tumor size, histology, and having stage IA into a model to estimate the magnitude of effect of gender on EBL, skin-to-skin operative time, and hospital LOS, using a backward stepwise method, with a significant level to stay at P≤0.05. In addition, the variables of history of infection and pleural adhesions were examined in the model for EBL.
Results
This study included 154 (55%) female patients and 128 (45%) male patients (Table 1). The mean age of 65.9±0.8 yr (range, 29–87 yr) in women was significantly less than that for men [68.8±0.9 yr (range, 34–86 yr); P=0.02] (Table 1). Female patients also had smaller BSA than males (1.8±0.02 vs. 2.0±0.02 m2; P<0.001), but there was no difference in body mass index (BMI) between the two groups (P=0.85). Preoperative pulmonary function shows women having a higher mean forced expiratory volume in 1 second (FEV1) as percentage of predicted (FEV1%, P<0.001), with 72.7% of the women having a FEV1% ≥80% (P=0.001) (Table 1). The diffusion capacity of the lung for carbon monoxide (DLCO) was lower in women as an absolute measurement (15.6 vs. 18.8 mL/mmHg/min, P<0.001), but did not differ between genders as a percentage of predicted (DLCO%; P=0.95).
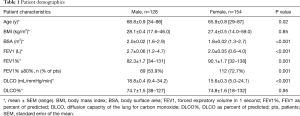
Full table
Former smokers were more common in males (55.5%; P=0.03) and non-smokers were more common in females (27.3%; P<0.001) (Table 2). Males in our cohort had more co-morbidities compared to females, including chronic obstructive pulmonary disease (COPD) (20.3% vs. 11.0%; P=0.009), diabetes mellitus (24.2% vs. 15.6%; P=0.07), atrial fibrillation (13.3% vs. 3.3%; P=0.002), and coronary artery disease (20.3% vs. 11.7%; P=0.05) (Table 2).
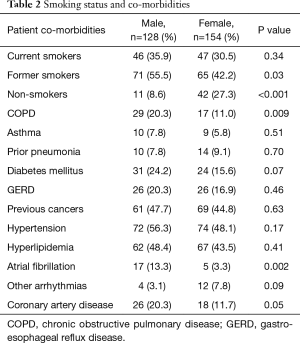
Full table
Women also tended to have smaller tumors, with average diameter of 3.0±0.1 cm, compared to men with mean tumor diameter of 3.5±0.2 cm (P=0.054) (Table 3). Adenocarcinoma was the most common histology for both genders, but more women had adenocarcinoma (63.6% vs. 47.7%, P=0.007), and more men had squamous cell carcinoma (26.6% vs. 12.3%, P=0.002) (Table 3).
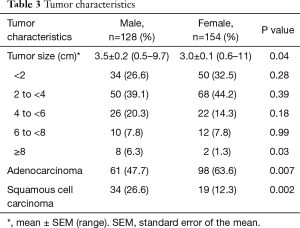
Full table
There were no differences in the extent of resection performed or in the laterality of resected specimens, with the exception of a higher proportion of right middle lobectomies in females (P=0.04) (Table 4). Approximately 90% of our cohort underwent lobectomy alone or required additional wedge resections to get adequate margins and/or to biopsy additional individual lesions. Table 5 demonstrates that, while more women had pathological stage-IA lung cancer (42.9% vs. 32.0%, P=0.06), there were no significant gender differences in the more advanced stages of primary lung cancers.
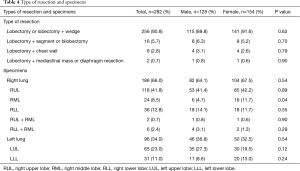
Full table
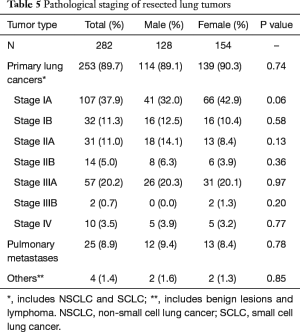
Full table
Rates of intraoperative complications and conversion rates were similar (Tables 6,7). The rate of overall intraoperative complications, such as bleeding, phrenic or recurrent laryngeal nerve injury, bronchial injury, or diaphragmatic injury, was 7.1% for the female group and 8.6% for the male group (P=0.65). Overall conversion rates to open lobectomy were also comparable, with 7.8% of women and 8.6% of men (P=0.81) requiring conversion, but only 3.9% of men and 2.6% of women (P=0.53) required emergent conversion for bleeding control.
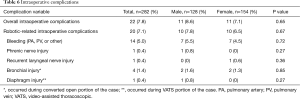
Full table
Full table
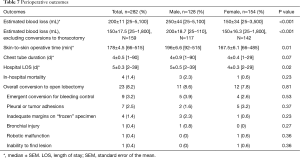
Perioperative outcomes tended to be in favor of women, with significantly lower median EBL (P<0.001), shorter median operative times (P=0.01), and shorter median hospital LOS (P=0.02) (Table 7). Median chest tube duration was 4 days for both genders (P=0.07), and in-hospital mortality did not differ between genders (P=0.23).
Women experienced fewer overall post-operative complications (27.9% vs. 44.5%, P<0.004), the majority of which were accounted for by prolonged air leak ≥7 days (13.0% vs. 22.7%, P=0.03), atrial fibrillation (7.1% vs. 14.8%, P=0.04), and other types of arrhythmias (0% vs. 3.9%, P=0.01) (Table 8). Other relevant pulmonary complications were pneumonia (7.8% of women vs. 10.2% of men, P=0.49) and mucous plug requiring intervention (4.5% of women vs. 7.0% of men, P=0.37).
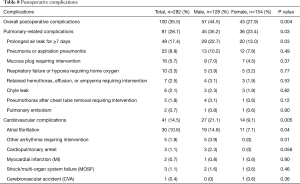
Full table
More men than women had pulmonary complications (35.2% vs. 23.4%, P=0.03) or cardiovascular complications (21.1% vs. 9.1%, P=0.005). Three men suffered cardiopulmonary arrest after surgery. Two of these three patients suffered cardiopulmonary arrest during the first 50 cases of our robotic-assisted lobectomy cohort. The first patient had pulmonary artery bleeding during attempted robotic-assisted right upper lobectomy, which required conversion to thoracotomy for bleeding control, but had a cardiac arrest during a second pulmonary artery bleeding episode during open completion right upper lobectomy. This patient subsequently developed multi-organ system failure and died from a third cardiac arrest on postoperative day #18 (POD18). The other two patients had prolonged respiratory complications with prolonged air leaks and pneumonia, which resulted in a cardiac arrest on POD16 for one patient and on POD17 for the other patient.
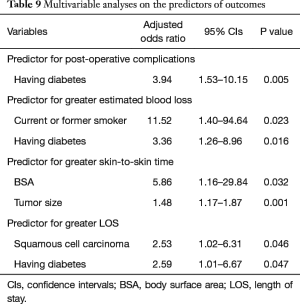
We subsequently performed analyses to identify the independent predictors of EBL, skin-to-skin operative time, total postoperative complications, and hospital LOS (Table 9). For our cohort, the median EBL was 200 cc, the median skin-to-skin operative time was 178 minutes, and the median hospital LOS was 5 days. We found that female gender was not an independent predictor of post-operative complications. Rather, having diabetes mellitus was the only factor predicting the occurrence of post-operative complications. Furthermore, having diabetes mellitus also independently predicted higher EBL and longer hospital LOS.
Full table
Discussion
Demographic and histological characteristics of participants in this study compare to those previously reported in the literature, with women being diagnosed an average of 2.8 years younger than their male counterparts and having a higher rate of adenocarcinoma and a lower rate of squamous cell carcinoma (4-6,15). The survival advantage for women after surgery for NSCLC has been documented to be independent of age at diagnosis, stage, histology, and life expectancy (6,16).
Women had higher FEV1% prior to surgery, which may be indicative of a lower rate of smoking and of underlying lung disease, such as COPD. Women in our cohort had a three-fold higher percentage of nonsmoker patients and almost half the percentage of COPD patients compared to the male group. Pre-operative pulmonary function has been shown to correlate with both complication rates and survival prognosis following resection when utilizing FEV1 ≥80% of predicted as the critical point in differentiating normal and impaired lung function (17,18). In our study, 72.7% of women met or exceeded the FEV1% ≥80% benchmark, while only 53.9% of men did.
Reports have suggested that women may delay seeking healthcare or treatment and may be treated with bias by physicians, leading to a delay in appropriate care (9,19,20). Neal et al. correlated gender and delayed procurement of secondary care in lung cancer patients, although this was not significant when controlling for age at presentation (20). The present study showed that women were more likely to present at our facility with a stage-IA tumor and did not show higher rates of T3 or T4 tumors, compared to what has been previously reported (4). Nevertheless, due to a younger age at presentation and higher likelihood of non-smoking-related cancers, continued diligence by primary providers in maintaining a low threshold for suspicion of pulmonary carcinomas is perhaps even more crucial when caring for women.
In terms of operative outcomes, women fared better in almost all categories. While there were no differences in intraoperative complications or in conversion to open lobectomy, women had a median operative time 30 minutes shorter, a median EBL 100 mL less, and a median hospital LOS one day less than men following surgery. Our reported complication rates for both genders compared well with ranges established in a systematic review of RAVT lobectomy published in 2012 (21). In addition to these factors, males have a documented higher incidence of 30-day re-admissions, related to underlying co-morbidities and postoperative complications (22). Similarly, our reported in-hospital mortality rates of 2.3% for men and 0.6% for women and our overall conversion rates of 8.6% in men and 7.8% in women also compare well with rates reported in that systematic review. Univariable models of individual postoperative complications using the Society of Thoracic Surgeons (STS) General Thoracic Database demonstrated that male gender was a significant predictor of pulmonary, cardiac, neurologic, hematologic, infectious, and gastrointestinal complications, with worse outcomes (23).
Park et al. published on 325 RAVT pulmonary lobectomies for NSCLC in 2011, reporting similar perioperative outcomes and causes for conversion, with adhesions (2.2%) and bleeding (0.9%) as the primary reasons after incomplete fissures (2.8%) (24). We reported a higher conversion rate to open lobectomy for bleeding in both genders (3.9% in males and 2.6% in females; P=0.72) and for adhesions in females (3.2% vs. 1.6% for males; P=0.37). These reasons for conversion to open lobectomy are likely related to our inclusion of more advanced stages of lung cancer, particularly those with bulky hilar or mediastinal LN involvement, in our cohort.
Despite female gender being a reported risk factor for complications in cardiovascular surgery, our study found female gender as protective for both pulmonary and cardiovascular complications following RAVT lobectomy (25-27). Most complications in both genders were minor and at rates similar to those previously reported, including prolonged air leaks (28-30). Men had a higher risk in developing atrial fibrillation and other types of arrhythmias requiring intervention (P<0.05). Increased rates of arrhythmias, particularly unstable arrhythmias, in men may be related to their underlying comorbidities, such as smoking status, COPD, and heart failure (31,32). In our study, males had higher rates of COPD and of coronary artery disease compared to females, supporting previous reports.
Expanding on our discussion of postoperative complications, other factors, such as pain, could be affecting surgical outcomes. In our practice, we use a standard pain control regimen. After creating our port incision, we place by VATS an extrapleurally tunneled On-Q Silver Soaker Catheter™ (I-Flow Corporation, Lake Forest, CA, USA) for postoperative intercostal nerve block. The On-Q system provides continuous postoperative analgesia as well as patient-controlled demand analgesia for regional nerve block, which is discontinued when the chest tube is removed. Perioperatively, we add non-steroidal anti-inflammatory drugs (NSAIDs), intravenous acetaminophen, medications intended for neuropathic pain relief, such as gabapentin, transdermal local anesthetic, and low-dose narcotics. Our goal is to decrease the amount of narcotics used and to increase the patient’s ability to take deep breaths and to participate in physical therapy. The relationship of our pain regimen and post-operative complications needs to be studied, but promising results using On-Q catheters have been published (33,34). Future research may use incentive spirometry recordings and which post-operative day of first ambulation to more objectively address the role of pain in the development of complications after thoracic surgery.
Female gender has also been identified as a positive prognostic factor for survival after lung cancer diagnosis as well as after lung resection in NSCLC, with one study reporting a hazard ratio of 0.5 at 5 years after resection (5-7,16). Lower rates of smoking, COPD, and pre-existing cardiovascular disease in women better explain differences in prolonged air leaks, and consequently in chest tube days and hospital LOS, as FEV1 ≤80% of predicted is a known risk factor (35,36). In our multivariable analyses of perioperative outcomes, including intraoperative EBL, operating time and hospital LOS, female gender was not found to be an independent predictor of these outcomes. The observation of fewer post-operative complications among female patients could be, in part, due to the lower incidence of diabetes among female patients. Furthermore, among female patients, the higher proportion of non-squamous cell carcinoma histology, their lower BSA, and their smaller tumor size contributed to their observed better outcomes overall. This relationship of diabetes mellitus and worse outcomes after pulmonary resection has been previously described. Diabetes mellitus is a presumed independent risk factor for bronchopleural fistula after pulmonary resections, with an odds ratio (OR) of 2 (37).
Limitations to the present study included lack of information about menopausal status of women, and complications were not stratified to account for as-yet undescribed variables that may underlie these differences. Further studies addressing these issues would be pertinent.
Conclusions
Female gender was not associated with increased intraoperative complications or conversion to open lobectomy nor with increased hospital LOS or in-hospital mortality following RAVT lobectomy. On the contrary, women had lower rates of both pulmonary and cardiovascular postoperative complications, mainly due to lower rates of prolonged air leaks ≥7 d and of atrial fibrillation. Smaller tumors and a higher rate of stage-1a primary lung cancers in females could be part of their improved surgical outcomes. Female gender was an independent predictor for lower intraoperative EBL. Our study suggests that RAVT lobectomy is safe and feasible in female patients and presents opportunities for future research comparing surgical techniques as well as hormonal and stress responses between genders in the early post-operative period.
Acknowledgements
This research was supported by 2014 Summer Scholarly Awards to JR Glover and EP Ng from the Scholarly Concentrations Program and a 2015 Summer Scholarly Award to K Toosi from the Office of Research, Innovation & Scholarly Endeavors (RISE) at the University of South Florida (USF) Health Morsani College of Medicine.
Footnote
Conflicts of Interest: EM Toloza and JP Fontaine have had financial relationships with Intuitive Surgical Corp. in the form of honoraria as robotic surgery proctors and observations sites. No other authors have any financial conflicts of interest to disclose. This manuscript updates our preliminary study previously presented at the 15th World Conference on Lung Cancer of the International Association for the Study of Lung Cancer in Sydney, Australia, on October 29, 2013.
Ethical Statement: The study was approved by our institution’s Scientific Review Committee (MCC #16512, MCC #16728, and MCC #18761) and by our Institutional Review Boards (USF IRB #Pro00002678, USF IRB #Pro00022263, and Chesapeake IRB #Pro00017745), and written informed consent was obtained from all patients.
References
- American Cancer Society. Cancer Facts & Figures 2015. Atlanta: American Cancer Society. Available online: http://www.cancer.org/acs/groups/content/@editorial/documents/document/acspc-044552.pdf
- Dela Cruz CS, Tanoue LT, Matthay RA. Lung cancer: epidemiology, etiology, and prevention. Clin Chest Med 2011;32:605-44. [Crossref] [PubMed]
- Alberg AJ, Samet JM. Epidemiology of lung cancer. Chest 2003;123:21S-49S. [Crossref] [PubMed]
- Minami H, Yoshimura M, Miyamoto Y, et al. Lung cancer in women: sex-associated differences in survival of patients undergoing resection for lung cancer. Chest 2000;118:1603-9. [Crossref] [PubMed]
- Ferguson MK, Wang J, Hoffman PC, et al. Sex-associated differences in survival of patients undergoing resection for lung cancer. Ann Thorac Surg 2000;69:245-9; discussion 249-50. [Crossref] [PubMed]
- Nakamura H, Ando K, Shinmyo T, et al. Female gender is an independent prognostic factor in non-small-cell lung cancer: a meta-analysis. Ann Thorac Cardiovasc Surg 2011;17:469-80. [Crossref] [PubMed]
- North CM, Christiani DC. Women and lung cancer: what is new? Semin Thorac Cardiovasc Surg 2013;25:87-94. [Crossref] [PubMed]
- Xiong J, Wang R, Sun Y, et al. Clinical analysis of sixty-four patients with T1aN2M0 stage non-small cell lung cancer who had undergone resection. Thorac Cancer 2016;7:215-21. [Crossref] [PubMed]
- Nojiri T, Hamasaki T, Inoue M, et al. Long-Term Impact of Postoperative Complications on Cancer Recurrence Following Lung Cancer Surgery. Ann Surg Oncol 2016. [Epub ahead of print]. [Crossref] [PubMed]
- Mucha L, Stephenson J, Morandi N, et al. Meta-analysis of disease risk associated with smoking, by gender and intensity of smoking. Gend Med 2006;3:279-91. [Crossref] [PubMed]
- Sasco AJ, Secretan MB, Straif K. Tobacco smoking and cancer: a brief review of recent epidemiological evidence. Lung Cancer 2004;45 Suppl 2:S3-9. [Crossref] [PubMed]
- Gale EA, Gillespie KM. Diabetes and gender. Diabetologia 2001;44:3-15. [Crossref] [PubMed]
- Juutilainen A, Kortelainen S, Lehto S, et al. Gender difference in the impact of type 2 diabetes on coronary heart disease risk. Diabetes Care 2004;27:2898-904. [Crossref] [PubMed]
- Melfi FM, Mussi A. Robotically assisted lobectomy: learning curve and complications. Thorac Surg Clin 2008;18:289-95. vi-vii. [Crossref] [PubMed]
- Bethune G, Bethune D, Ridgway N, et al. Epidermal growth factor receptor (EGFR) in lung cancer: an overview and update. J Thorac Dis 2010;2:48-51. [PubMed]
- Båtevik R, Grong K, Segadal L, et al. The female gender has a positive effect on survival independent of background life expectancy following surgical resection of primary non-small cell lung cancer: a study of absolute and relative survival over 15 years. Lung Cancer 2005;47:173-81. [Crossref] [PubMed]
- Bernard A, Ferrand L, Hagry O, et al. Identification of prognostic factors determining risk groups for lung resection. Ann Thorac Surg 2000;70:1161-7. [Crossref] [PubMed]
- Berry MF, Jeffrey Yang CF, et al. Impact of Pulmonary Function Measurements on Long-Term Survival After Lobectomy for Stage I Non-Small Cell Lung Cancer. Ann Thorac Surg 2015;100:271-6. [Crossref] [PubMed]
- Smith LK, Pope C, Botha JL. Patients' help-seeking experiences and delay in cancer presentation: a qualitative synthesis. Lancet 2005;366:825-31. [Crossref] [PubMed]
- Neal RD, Allgar VL. Sociodemographic factors and delays in the diagnosis of six cancers: analysis of data from the "National Survey of NHS Patients: Cancer". Br J Cancer 2005;92:1971-5. [Crossref] [PubMed]
- Cao C, Manganas C, Ang SC, et al. A systematic review and meta-analysis on pulmonary resections by robotic video-assisted thoracic surgery. Ann Cardiothorac Surg 2012;1:3-10. [PubMed]
- Medbery RL, Gillespie TW, Liu Y, et al. Socioeconomic Factors Are Associated With Readmission After Lobectomy for Early Stage Lung Cancer. Ann Thorac Surg 2016;102:1660-7. [Crossref] [PubMed]
- Tong BC, Kosinski AS, Burfeind WR Jr, et al. Sex differences in early outcomes after lung cancer resection: analysis of the Society of Thoracic Surgeons General Thoracic Database. J Thorac Cardiovasc Surg 2014;148:13-8. [Crossref] [PubMed]
- Park BJ. Robotic lobectomy for non-small cell lung cancer (NSCLC): Multi-center registry study of long-term oncologic results. Ann Cardiothorac Surg 2012;1:24-6. [PubMed]
- Nguyen LL, Hevelone N, Rogers SO, et al. Disparity in outcomes of surgical revascularization for limb salvage: race and gender are synergistic determinants of vein graft failure and limb loss. Circulation 2009;119:123-30. [Crossref] [PubMed]
- Song HK, Grab JD, O'Brien SM, et al. Gender differences in mortality after mitral valve operation: evidence for higher mortality in perimenopausal women. Ann Thorac Surg 2008;85:2040-4; discussion 2045. [Crossref] [PubMed]
- Edwards FH, Carey JS, Grover FL, et al. Impact of gender on coronary bypass operative mortality. Ann Thorac Surg 1998;66:125-31. [Crossref] [PubMed]
- Ciriaco P, Mazzone P, Canneto B, et al. Supraventricular arrhythmia following lung resection for non-small cell lung cancer and its treatment with amiodarone. Eur J Cardiothorac Surg 2000;18:12-6. [Crossref] [PubMed]
- Nasir BS, Bryant AS, Minnich DJ, et al. Performing robotic lobectomy and segmentectomy: cost, profitability, and outcomes. Ann Thorac Surg 2014;98:203-8; discussion 208-9. [Crossref] [PubMed]
- Giambrone GP, Wu X, Gaber-Baylis LK, et al. Incidence and implications of postoperative supraventricular tachycardia after pulmonary lobectomy. J Thorac Cardiovasc Surg 2016;151:982-8. [Crossref] [PubMed]
- Konecny T, Park JY, Somers KR, et al. Relation of chronic obstructive pulmonary disease to atrial and ventricular arrhythmias. Am J Cardiol 2014;114:272-7. [Crossref] [PubMed]
- Zhu W, Yuan P, Shen Y, et al. Association of smoking with the risk of incident atrial fibrillation: A meta-analysis of prospective studies. Int J Cardiol 2016;218:259-66. [Crossref] [PubMed]
- Forastiere E, Sofra M, Giannarelli D, et al. Effectiveness of continuous wound infusion of 0.5% ropivacaine by On-Q pain relief system for postoperative pain management after open nephrectomy. Br J Anaesth 2008;101:841-7. [Crossref] [PubMed]
- Wheatley GH 3rd, Rosenbaum DH, Paul MC, et al. Improved pain management outcomes with continuous infusion of a local anesthetic after thoracotomy. J Thorac Cardiovasc Surg 2005;130:464-8. [Crossref] [PubMed]
- Elsayed H, McShane J, Shackcloth M. Air leaks following pulmonary resection for lung cancer: is it a patient or surgeon related problem? Ann R Coll Surg Engl 2012;94:422-7. [Crossref] [PubMed]
- Mueller MR, Marzluf BA. The anticipation and management of air leaks and residual spaces post lung resection. J Thorac Dis 2014;6:271-84. [PubMed]
- Li SJ, Fan J, Zhou J, et al. Diabetes Mellitus and Risk of Bronchopleural Fistula After Pulmonary Resections: A Meta-Analysis. Ann Thorac Surg 2016;102:328-39. [Crossref] [PubMed]


