Chronic expanding hematoma: a late complication 45 years after thoracoplasty
Introduction
The term “chronic expanding hematoma” was first introduced in reference to hematomas with continuous growth (1). Histologically, a mixture of old and new hematoma accompanied by a fibrous pseudocapsule is seen in the condition. Chronic expanding hematoma occurs in various locations in the body (1,2).
Thoracoplasty involves removing ribs from the chest wall in order to collapse the cavities created by tubercular infection. Although thoracoplasty is rarely used in developed countries because of the widespread availability and use of anti-tubercular medications, it is still a clinical option in developing countries (3).
Previously, several cases of chronic expanding hematoma of the chest after thoracic surgery have been reported (4). In particular, chronic expanding hematoma has been described as a possible complication after thoracoplasty for tuberculosis treatment (1,5-7). In the current article, we describe a case of an extra-thoracic chronic expanding hematoma after thoracoplasty.
Case presentation
A 69-year-old right-handed male was referred to our institute. Forty-five years earlier, he underwent thoracoplasty of the right upper thorax for tuberculosis. Six months prior to his visit with us, he had noticed a slight swelling on his back, and 3 months before the visit, the size of the swollen area gradually increased after bowling. After a visit to a nearby hospital, he was referred to our institute. Initial laboratory examination was unremarkable.
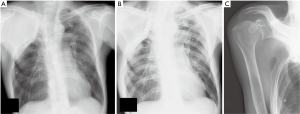
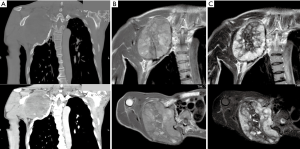
Plain radiographs showed a deformity of the thorax secondary to prior thoracoplasty (Figure 1). Plain computed tomography (CT) showed an extra-thoracic lesion measuring 120 mm in diameter. An ossified capsule was seen at the border between the lesion and the chest wall (Figure 2A). Contrast-enhanced CT depicted newly formed vessels inside the lesion on the thoracic side (Figure 2A). Magnetic resonance imaging (MRI) demonstrated nodularity of the lesion, with a slightly high signal intensity on T1 weighted images (Figure 2B). The lesion had heterogeneous low to high signal intensity on T2 weighted images. The T2 weighted images furthermore showed high signal intensity at the periphery of the lesion, and low signal intensity inside the lesion (Figure 2C). High signal intensity areas on both T1 and T2 weighted images were not suppressed on fat-suppressed T2-weighted images (Figure 2C). Heterogeneous signal intensity on MRI inside the lesion was assumed to be a mixture of various ages of hematoma. A thin pseudocapsule characterized by low intensity on T1 and T2 weighted images was also seen (Figure 2B,C). Taking into consideration the clinical course, the diagnosis of a chronic expanding hematoma was made.
Embolization of the vessels supplying the lesion was performed before the operation. Resection was then undertaken. The surgical approach was through the medial aspect of the scapula with dissection of the overlying muscle. During the operation, the pseudocapsule on the thoracic side was left in place as it was adherent to the chest wall. Total blood loss during the operation was 850 mL. Blood transfusion was given postoperatively, and the patient was stable throughout. Rehabilitation of the shoulder joint began 1 week postoperatively. He was discharged from the hospital after 21 days. Shoulder rehabilitation continued for almost 6 months at a near-by hospital. Histologically, the resected lesion was confirmed to be a hematoma. The patient had no functional deficits in his shoulder postoperatively, and no recurrence with a 5-year follow-up.
Discussion
Various histologic and radiographic findings inside a chronic expanding hematoma are observed over time. A pseudocapsule characterized by low signal intensity on T1 and T2 weighted images is a consistent finding in chronic expanding hematomas; the pseudocapsule was thin in the current case. Histologically, the pseudocapsule is composed of fibrous tissue, hemosiderin deposits and iron-laden macrophages (1). MRI findings of a chronic hematoma are similar to that in hemorrhagic soft tissue sarcomas (8). In order to diagnose chronic expanding hematomas, a combination of clinical course and imaging is helpful.
The definitive treatment of a chronic expanding hematoma is complete removal, including the pseudocapsule (9); incomplete removal may lead to recurrence. However, complete removal is often difficult because the pseudocapsule is frequently adherent to the surrounding tissue. In the current case of an extra-thoracic chronic expanding hematoma, separation of the pseudocapsule from the thoracic wall may have caused massive bleeding. Therefore, the pseudocapsule on the chest well was preserved. Similar incomplete resections, however, have been reported with good overall results (10).
According to reported cases of chronic expanding hematoma after thoracoplasty performed for tuberculosis, chronic expanding hematomas can occur from 24 to 42 years after surgery (4-7,11). Chronic expanding hematomas are thus considered a late complication. Among these reported cases, extrapleural pneumonolysis (plombage) with polymethyl methacrylate (Lucite) balls was frequently performed. Though we assume there to be an association between chronic expanding hematomas and the plombage operation (11), thoracoplasty alone seems to be a risk factor for chronic expanding hematoma. The frequency of this complication is not known due to the paucity of reported cases. Tuberculosis was extremely prevalent in Japan, with 3,000,000 people having active tuberculosis in the 1950s. Thoracoplasty was one of the effective treatments for pulmonary tuberculosis in this period (12). In a case report of chronic expanding hematoma after thoracoplasty in 2003, the author made the comment that the case was the 5th such case reported in Japan in the English literature (4).
In the current report, the patient was asymptomatic for more than 40 years, and 6 months before admission with us he began to notice swelling on his back. He had no medical history nor was he on a medication that would predispose him to hematoma formation. The exact cause of chronic expanding hematoma after thoracoplasty is not known. However, because chronic expanding hematoma occurs in an extra-thoracic lesion with no evidence of active tuberculosis infection at the occurrence site, the thoracic deformity created with thoracoplasty seems to be related to hematoma formation. The small vessel branches to the surrounding tissue including to the thoracic wall may be less flexible and susceptible to damage. In support of this, in the current case, the size increase of the hematoma accelerated after bowling.
In the current case, we report on a chronic expanding hematoma after thoracoplasty. With improvements in antibiotics against tuberculosis, thoracoplasty is rarely performed in the present day. However, chronic expanding hematomas can occur long after the original thoracoplasty, and malignancy must always be considered in the differential diagnoses. Chronic expanding hematoma should be suspected with a growing mass lesion over a previous thoracoplasty site.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Reid JD, Kommareddi S, Lankerani M, et al. Chronic expanding hematomas. A clinicopathologic entity. JAMA 1980;244:2441-2. [Crossref]
- Negoro K, Uchida K, Yayama T, et al. Chronic expanding hematoma of the thigh. Joint Bone Spine 2012;79:192-4. [Crossref]
- Gomes MM, Alves M, Correia JB, et al. Empyema necessitans: very late complication of pulmonary tuberculosis. BMJ Case Rep 2013;2013. pii: bcr2013202072.
- Takanami I. Successful treatment of huge chronic expanding hematoma after thoracoplasty. J Thorac Cardiovasc Surg 2003;126:1202-3. [Crossref]
- Uramoto H, Nakanishi R, Eifuku R, et al. Chronic expanding hematoma in the chest. J Cardiovasc Surg (Torino) 2000;41:143-6.
- Hanagiri T, Muranaka H, Hashimoto M, et al. Chronic expanding hematoma in the chest. Ann Thorac Surg 1997;64:559-61. [Crossref]
- Takeo S, Hara N, Ohtsu Y, et al. Giant extrathoracic hematoma after thoracoplasty--a case report. Jpn J Surg 1991;21:360-3. [Crossref]
- Imaizumi S, Morita T, Ogose A, et al. Soft tissue sarcoma mimicking chronic hematoma: value of magnetic resonance imaging in differential diagnosis. J Orthop Sci 2002;7:33-7. [Crossref]
- Muramatsu T, Shimamura M, Furuichi M, et al. Treatment strategies for chronic expanding hematomas of the thorax. Surg Today 2011;41:1207-10. [Crossref]
- Roper CL, Cooper JD. Chronic expanding hematoma of the thorax. J Thorac Cardiovasc Surg 2001;122:1046-8. [Crossref]
- Ueda H, Baba H, Ondo K. Chronic expanding hematoma of thorax extended to the neck. Ann Thorac Cardiovasc Surg 2014;20 Suppl:535-8. [Crossref]
- Tamura A, Hebisawa A, Hayashi K, et al. Lung cancer in patients who had received thoracoplasty for pulmonary tuberculosis. Jpn J Clin Oncol 1999;29:541-5. [Crossref]


