Update on the diagnosis and treatment of tracheal and bronchial injury
Introduction
Tracheal and bronchial injuries are more common in patients with thoracic trauma caused by traffic accidents. However, with the development of medical treatment, iatrogenic injury is gradually increasing. Main treatment of trachea is kposthesis and anastomosis. So early diagnosis and early surgical repair are the key to reduce complications and avoid the loss of lung function in patients with tracheal and bronchial injuries.
Classification
From etiology the tracheobronchial injury can be classified as traumatic and iatrogenic sources, in which the traumatic etiology includes crush injury, firearm injury and sharp instrument injury, which can be combined with the injury of cervical and thoracic vertebrae, large vessel, lung, thyroid, heart, esophagus and so on; From mechanism it can be classified as blunt injury and sharp injury, and the blunt injury is frequently complicated by neck and chest combined injury, even severe throat edema that can result in asphyxia or pulmonary edema which can lead to respiratory distress syndrome. From the lesion site, it can be divided into cervical tracheal injury, thoracic tracheal injury, major bronchial injury and lobar/segmental bronchial injury.
Clinical manifestation
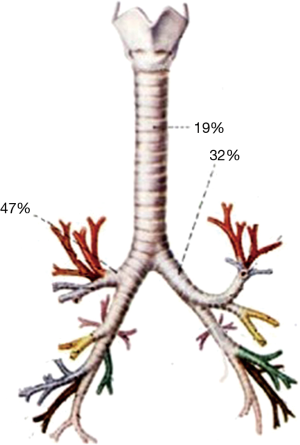
The clinical symptoms of simple airway mucosal laceration are always not obvious or only have small amount of blood sputum. It suggests presence of serious tracheobronchial injury with symptoms of shortness of breath, cyanosis, irritating cough, hemoptysis and pneumothorax. In severe chest trauma caused by traffic accidents or falling from height, the shear strain on the main bronchus caused by variable motion and the airway pressure surge caused by closed glottis can lead to rupture of the trachea and bronchi. Palade E reported that the right main bronchial rupture (47%) is more common than that in the left side (32%) for the right main bronchus is more fixed. Main tracheal rupture accounts for 19% (1) (Figure 1). But Siegel et al. found that there was no significant difference in the incidence of injury between the left and right sides (2) (Table 1).
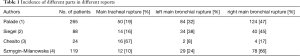
Full table
Dyspnea: there are many reasons that can cause dyspnea in tracheal rupture, such as pneumothorax, obstruction of blood or secretions in respiratory tract, pulmonary contusion that leads to oxygen exchange barriers, bronchial mucosal edema, hematoma compression to airway or lung tissue. The first symptom of main bronchial injury is pneumothorax, which often cause serious lung compression and even tension pneumothorax. As a result it blocks venous blood flow and results in heart failure, etc. (3). What’s more, even after placing pleural closed drainage, large amount of gas can be drained out with the movement of respiratory. Refractory pneumothorax and long-term pulmonary rehabilitation difficulty can also exist. The old tracheal injury can cause lobar or segmental atelectasis because of the granuloma in the lesion, so that it can present with symptoms like breathing difficulty and so on. However, the patients above always perform as recurrent pulmonary infection which is the main reason to hospital.
Subcutaneous or mediastinal emphysema: subcutaneous or mediastinal emphysema are the main symptoms of airway perforation with hemoptysis and dyspnea or not. Severe pneumomediastinum always appears in intrathoracic trachea injury, and the air can spread to the neck, head and chest, bilateral chest wall through suprasternal fossa that results in subcutaneous emphysema last. There are reports that the serious subcutaneous emphysema after trachea injury could even spread to the abdomen, perineum and lower extremity skin (4). In some cases the subcutaneous emphysema could also induce air embolism, but these patients were always associated with complex trauma and large vessel rupture etc. The severe pneumomediastinum might also compress the vena cava that led to reflux disorder and even heart failure.
Most of the hemoptysis caused by tracheal injury is slight, but it can also present with massive hemoptysis if there is bronchial artery injury or tracheal fistula with high mortality (5). Always there is fatal injury in these patients that will die from hemorrhagic shock and suffocation in short time, so that these patients have not enough time to be sent to the emergency room.
There is still a high misdiagnosis rate (68–35%) in the patients with mediastinal infection, bronchial pleural fistula, pulmonary atelectasis and injury of trachea and bronchus (6). And some patients were diagnosed until presenting with mediastinal infection and persistent pulmonary atelectasis.
Iatrogenic injury: the main symptoms of superficial injury are small hemoptysis, while the large damage can cause mediastinal or subcutaneous emphysema. Patients with ventilator support can occur with sudden lower airway pressure or tension pneumothorax. Such injuries are common in clinical practice, most of which occur in the operation of tracheotomy (0.2%), tracheal intubation (0.1%) and esophageal surgery (0.4%) (7). It is difficult to find the mild injury which may even be delayed into a chronic airway injury and be found until the airway stenosis exist.
Diagnosis of tracheal injury
It is not difficult to diagnose the cervical tracheal injury with clear history of injury and wound sucking sound associated with respiratory movement. But the injury of thoracic trachea and bronchus are often overlooked. Barrett et al. believed that: the tracheal injury should be excluded in chest closed injury patients in spite of pneumothorax, especially in severe crush injury, blast injury or falling injury patients (8).
Examination means includes chest X-ray, chest CT and bronchoscopy. X-ray examination is simple and fast with clear diagnosis for complete rupture of the trachea. The “lung fall syndrome” always prompts the loss of bronchial suspension so that the injured lung decreases to the cardio-diaphragmatic angle, which is different from the compression of normal lung tissue to the hilum of lung for pneumothorax. The main tracheal rupture can also present with this decline for gravity which can be diagnosed with the tracheal disruption that could be performs on the chest X-ray.
Chest CT is better than chest radiograph in the diagnosis of the rupture of main bronchus or lobe/segment bronchus. The characteristic expression of tracheal rupture in CT performs as follows: (I) gas dispersion around the broken ends (59%); (II) bronchial lumen stenosis or blockage (50%); (III) bronchial displacement or angular deformity (50%) (9). The chest CT of the patients with chronic bronchial injury can be manifested as capsular bag change in the end of the proximal rupture, or local tubal wall stenosis with corresponding distal pulmonary atelectasis. But some researchers believe that the diagnostic value of CT scan is not better than the chest X-ray, because tracheal fracture is always accompanied by multiple contusion, edema, hemorrhage or bronchial secretions blocking the lumen in the mediastinum and pulmonary, so that it is difficult to clearly determine whether there is tracheal injury by CT (10). For patients who cannot tolerate bronchoscopy, we can choose multi-planar two-dimensional or three-dimensional reconstruction and simulation bronchoscopy technology which can show the airway disease in conventional axial CT imaging in just a few minutes. For cases with severe chest trauma whose CT is negative but highly suspected bronchial rupture, the technique of three-dimensional reconstruction of MDCT can be used to reconstruct the bronchial tree for the diagnose of complete bronchus rupture.
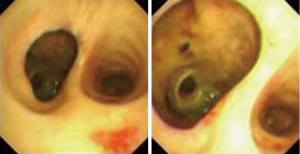
Bronchoscopy is one of the diagnosis methods under which we can find the tube wall rupture (Figure 2), and it is better than the former above in the diagnose of small injury (11). Bronchus injury with unobvious symptoms can be found through this technique. At the same time, bronchoscopy can be used to accurately locate and estimate the degree/scope of damage so as to guide the treatment. Wood et al. suggested that it was necessary to use conventional bronchoscopy for trauma patients with high suspicion of bronchial rupture as soon as possible if patients’ general status was available (12).
Tracheography can also be used in the diagnosis of tracheal injury, which is always used in patients with chronic bronchial injury or tracheal stenosis, especially in patients with trachea-esophageal fistula and trachea-pleural fistula.
Tracheography can also be used to distinguish the bronchial dilation or bronchial foreign body and chronic airway injury which is difficult to be identified by CT. In addition, because granulation tissue hyperplasia can lead to stenosis which provides blurred vision under bronchoscopy, so the tracheography has more diagnostic advantage (13). However, it is higher for the requirement of coordination degree in tracheography, so it is not suitable for patients with acute injury accompanied with hemoptysis, pulmonary atelectasis and bad general conditions.
Treatment of tracheal injury
Conservative treatment
The simple airway mucosal tearing is always self-limited without any special treatment. Cui et al. believed that if the breach was less than 1 cm, it could gradually stop leaking and naturally be cured (14). Most scholars thought that simply small crack could be treated conservatively (15). The indications of conservative treatment: (I) <2–3 cm or <1/3 diameter; (II) no other injury (such as esophagus), mild symptoms and signs, no signs of infection, stable and patency airway, stable spontaneous breathing; (III) intrathoracic trachea-bronchial injury without persistent air leakage or reexpansion of the lung after chest tube drainage. In addition to the use of antibiotics to prevent infection, combination of closed thoracic drainage and negative pressure suction is also necessary. It can not only promote the ipsilateral lung reexpansion, but also absorb the surrounding tissue to pack the crack. The size of crack determines the degree of negative pressure. The larger gap requires the larger negative pressure to ensure the lung reexpansion. There were reports that suction with large negative pressure could be used for the treatment of bronchial rupture whose diameter was about 1.4 cm (16).
Emergency treatment
Most airway rupture is urgent and the patients are always sent to the emergency department. In the emergency treatment, airway patency should be the first step, we should clear the secretions in airway to ensure the supply of oxygen. If patients are in acute stage with severe air leakage, breathing difficulties and unstable general condition, they should be intubated after making a definite diagnosis. Intubation can also support the collapsed trachea (17). What’s more, sometimes tracheal intubation can also play a role in temporarily blocking the tracheal rupture by breaking over the crack in the cervical or upper thoracic tracheal injury. For the patients with injury of inferior segment or bronchus, the cannula can be placed to the contralateral main bronchus for one-lung ventilation, and the operation had better be finished under the guide of flexible bronchofiberscope to avoid aggravating the injury (18). It is better to avoid the positive pressure ventilation to prevent further expansion of tear as far as possible. The cannula can be placed in the subglottis with high frequency ventilation, which helps to prevent rupture from further expanding; it needs emergency thoracotomy surgery for the patients with difficult intubation or difficult ventilation. Cannula could be placed into the contralateral main bronchus by the guide of operator’s finger. In recent years, the cardiopulmonary bypass (ECMO) was also used for the patients with difficult intubation to ensure the oxygen saturation (19). This method can be applied to the tracheal operation with wide range of crack which is difficult to repair. Patients with complete tracheal rupture caused by penetrating injury in the neck can also be directly rescued by intubating through the open wound in an emergency. In addition, the chest or mediastinal decompression is also very important in emergency treatment, and pleural closed drainage is often the preferred method (20).
Surgical treatment
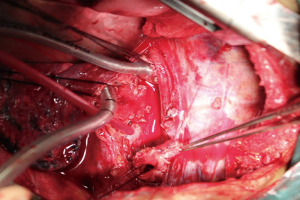
In principle, rupture of the trachea and bronchus should be operated as soon as possible. The achievement ratio is very high in early repair on healthy tissue with quick improvement to the dysfunction of ventilation and better long-term outcome (21); the broken end delayed to late stage may appear scar stricture, infection, retraction and adhesion, which is not conducive to surgical repair. General surgery includes repair, end to end anastomosis, sleeve resection, lobectomy or pneumonectomy, autologous tissue repair or reconstruction (Figure 3). Most cases can be cured by repair or anastomosis. In addition to patients with severe pulmonary parenchymal injury, there is no need for lung resection. The unilateral whole pulmonary atelectasis caused by old main bronchial rupture can be reexpanded through tracheal intubation after removing lumen secretions in the airway. The combined injury should be repaired at the same time. Especially in patients with esophageal laceration, we can use adjacent healthy tissue or greater omentum to cover the laceration while repairing it (22).
Selection of operative incision
If the injury occurs in the proximal 2/3 trachea, the incision could be selected on the neck. When the trauma is mild and complication is little, we can use local anesthesia. At first, a curved incision was made on the sternal notch with a cross finger. Then reveal the trachea by separating the anterior cervical muscle. If it is difficult to expose, we can do part or whole sternotomy (23). When the fracture occurs on the lower section of the sternum or main bronchus, incision could be selected on the posterior lateral right side. Then cut off the azygos vein to expose the trachea and carina. We can also select middle chest incision, so that there is no need to enter the pleural cavity with less impact on the breath and better postoperative recovery (24). However, thoracotomy is suggested to the patients with blunt injury or hemopneumothorax so as to detect the pleural hemorrhage and fracture, etc. (25).
Exploration
The neck injury or perforation is more common in the injury of neck. Injury site always located in the sagittal plane of trachea or the junction of cartilage and membranous part, which is close to the hematoma. Thoracic crack can be identified by pneumomediastinum or gas leakage. Most injuries (80%) locate in the carina within 2.5 cm (26). There were reports that tracheal injury can be complicated with cardiac vascular injury (27). Therefore, it is necessary to explore the major vessels of the heart in patients with severe injury. When there is obvious infection or putrid flavor, we need to focus on exploring the esophageal injury (28).
End to end anastomosis
After a thorough debridement and hemostasis, the edge of the gap should be trimmed to guarantee the wound end to end alignment, then the whole layer of the bronchial gap should be sutured. If the tension of the broken end is too high, the gap could be sutured with thick seam to hang together to reduce the tension, and the remaining is closed with a U type or interrupted suture from membranous part to the front line. The sutures should be kept outside of the lumen so as to avoid the postoperative irritating cough and the stenosis from granulation tissue hyperplasia. When the main airway injury is serious enough to make the upper and lower ends far apart, the neck can be fixed in 35 degree flexion with Pearson position to reduce the tension of the airway. Some studies found that the maximum distance of the main airway relaxation was 4.5 cm (29). When the difference of the diameter from the upper end to the lower end is big enough, the needle should be arranged evenly and sometimes one side could be cut off to expand the incision, or using the membranous part for correction. The needle had better go through the cartilage as far as possible, and the first suture should be made on the difficult exposed part. The worked trachea should be avoided form tension, distortion and angle. After all of these above, it is better to cover the pleural flap or the muscle flap on the anastomotic stoma.
Lobectomy and pneumonectomy
Whenever possible, use bronchial rupture repair and anastomosis, and try the best to protect the lung tissue. We’d better avoid using lung resection, especially the whole lung resection which will significantly improve the postoperative mortality rate (30). But for the patients with serious lung damage that can not be repaired and prone to infection after operation, removal of the damaged lung is a necessary way for saving life. What’s more, if the scope of the tracheal injury is wide enough that makes the operation more difficult and tends to postoperative tracheal stenosis, it is recommended to remove lung disease if the residual lung injury allows (26).
Chronic tracheal rupture
Stenosis always appears in chronic tracheal rupture due to the growth of granulation tissue or scar which should be resected and coincided in surgery. When the stenosis length is too large to cause high anastomotic tension, neck fixation could be used for relaxing and coinciding within 4.5 cm resection. If the distance is more than 4.5 cm, 3 cm distance could be prolonged through loosing and separating the upper and lower ends, separating the structure around hilum and loosing the explant adhesion.
Grillo et al. thought that prolonged distance could be finished through loosing inferior pulmonary ligament, separating large vessels and accretio cordis, and cutting off the left main bronchus and transplanting to the right main middle section in some special circumstances (31). The total length of trachea resection can be as long as 6.6 cm. One side whole pulmonary atelectasis caused by chronic main bronchial rupture can be well reexpanded by removing the airway secretions and using intubation ventilation. It has been reported that even the history of chronic tracheal injury was more than 2 years, the function of the distant lung could be recovered after surgery (32).
Postoperative treatment
After surgery, the lower jaw should be fixed to the skin of frontier chest with a thick line, so that the neck is positioned in Pearson position from which it can prevent the postoperative neck from suddenly moving back again to break the not yet healed wound. The suture should be reserved for about 1 week until the breach has healed. The neck can be free after 2 weeks. But some scholars believed that the neck should be fixed for one month to prevent tracheal anastomotic stenosis (33).
The intubation can be removed after surgery. Patients complicated with pulmonary contusion should be kept intubation with the support of ventilation. We should pay attention to the position of the air bag that might be moved to the anastomotic site, because even the low pressure air bag will also affect the healing of tracheal anastomotic site (34).
After surgery we should remember to maintain the airway patency, resolve the phlegm, wet the trachea, aspirate sputum with flexible bronchofiberscope, maintain the drainage fluently, and promote pulmonary rehabilitation. If there is a small leakage, it is suggested to use negative pressure suction earlier with continuous 5–10 cmH2O negative pressure. What more, it is also very important to correct the pulmonary contusion caused by trauma, limit the amount of liquid, and reduce pulmonary edema. If there is bronchial rupture, it is necessary to avoid using positive pressure ventilation although this is one of the effective methods for the treatment of pulmonary edema (35). Early use of hormones can be helpful to the edema of stoma and pulmonar, but there are also some scholars believed that this might increase the risk of infection (36).
Conclusions
Early diagnosis is a prerequisite for the successful treatment of bronchial rupture patients, in which successful intubation is a basic guarantee. Reasonable treatment of complications can reduce the mortality rate, at the same time well intraoperative airway management makes the stomas more precise. For these patients as soon as diagnosis is made we should take active surgical treatment. The key to successful operation lies in low tension neat anastomosis. All of above can ensure the successful rehabilitation and a good quality of life after surgery.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Palade E, Passlick B. Surgery of traumatic tracheal and tracheobronchial injuries. Chirurg 2011;82:141-7. [Crossref]
- Siegel B, Bent JP, Weinstein S. Tracheal rupture in complicated delivery: a case report and review of the literature. Int J Pediatr Otorhinolaryngol 2014;78:1784-8. [Crossref]
- Cheaito A, Tillou A, Lewis C, et al. Traumatic bronchial injury. Int J Surg Case Rep 2016;27:172-5. [Crossref]
- Szmygin-Milanowska K, Grzywa-Celińska A, Krusiński A, et al. Pneumomediastinum - a case report. Pol Merkur Lekarski 2016;41:93-6.
- Kulyapina A, Díaz DP, Rodríguez TS, et al. Tracheoinnominate fistula: a rare acute complication of penetrating neck injury. Asian Cardiovasc Thorac Ann 2015;23:478-80. [Crossref]
- Kurgansky IS, Makhutov VN, Lepekhova SA. The methods for the treatment and prevention of cicatrix stenoses of trachea. Vestn Otorinolaringol 2016;81:66-71. [Crossref]
- Dias A, O'Neill P, Fenton J. Iatrogenic tracheal tear. West Indian Med J 2010;59:578-80.
- Barrett E. Management of a traumatic tracheal tear: a case report. AANA J 2011;79:468-70.
- Baisi A, Nosotti M, Cioffi U, et al. Diagnosis of complete mainstem bronchus avulsion by 3-dimensional spiral CT scan of the chest. Minerva Chir 2003;58:587-9.
- Karmy-Jones R, Avansino J, Stern EJ. CT of blunt tracheal rupture. AJR Am J Roentgenol 2003;180:1670. [Crossref]
- Singh S, Gurney S. Management of post-intubation tracheal membrane ruptures: A practical approach. Indian J Crit Care Med 2013;17:99-103. [Crossref]
- Wood JW, Thornton B, Brown CS, et al. Traumatic tracheal injury in children: a case series supporting conservative management. Int J Pediatr Otorhinolaryngol 2015;79:716-20. [Crossref]
- Parshin VD, Koroleva IM, Mishchenko MA. Evolution of diagnostic methods for cicatrical tracheal stenosis and tracheomalacia]. Khirurgiia (Mosk) 2016.17-25. [Crossref]
- Cui Y, Wang X, Zhu W. A case of tracheal tube rupture of an adult patient. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2014;28:426-7.
- Brinas P, Bréhin C, Breinig S, et al. Conservative management of tracheal injuries in children: Clinical case and literature review. Arch Pediatr 2016;23:1067-70. [Crossref]
- Altinok T, Can A. Management of tracheobronchial injuries. Eurasian J Med 2014;46:209-15. [Crossref]
- Menkiti ID, Badmus OO, Adekola OO, et al. Tracheal Intubation in the Emergency Department of a Sub-Saharan Teaching Hospital:A One-Year Survey at Lagos University Teaching Hospital, Nigeria. West Afr J Med 2014;33:201-5.
- Welter S, Hoffmann H. Injuries to the tracheo-bronchial tree. Zentralbl Chir 2013;138:111-6.
- Zhou R, Liu B, Lin K, et al. ECMO support for right main bronchial disruption in multiple trauma patient with brain injury--a case report and literature review. Perfusion 2015;30:403-6. [Crossref]
- Buschmann CT, Tsokos M, Kurz SD, et al. Tension pneumomediastinum and tension pneumothorax following tracheal perforation during cardiopulmonary resuscitation. Anaesthesist 2015;64:520-6. [Crossref]
- Lui N, Wright C. Intraoperative Tracheal Injury. Thorac Surg Clin 2015;25:249-54. [Crossref]
- Gazala S, Bedard E. Surgisis mesh for tracheal reconstruction. Ann Thorac Surg 2012;93:2076-7. [Crossref]
- Welter S, Cheufou D, Darwiche K, et al. Tracheal injuries, fistulae from bronchial stump and bronchial anastomoses and recurrent laryngeal nerve paralysis: management of complications in thoracic surgery. Chirurg 2015;86:410-8. [Crossref]
- Murthy T. Anaesthetic management of carinal resection and reconstruction-a case report. Indian J Anaesth 2009;53:340-3.
- Goykhman Y, Paz J, Sarid E, et al. Blunt chest trauma with disruption in the intrathoracic trachea. Isr Med Assoc J 2010;12:770-2.
- Szyfter W, Nowak K, Kruk-Zagajewska A. Experiences with treatment of extended laryngo-tracheal stenosis with employment of transversal resection of trachea. Otolaryngol Pol 2008;62:695-9. [Crossref]
- Kim S, Park JS, Yoo SM, et al. Traumatic aortic regurgitation combined with descending aortic pseudoaneurysm secondary to blunt chest trauma. Cardiovasc J Afr 2014;25:e5-8. [Crossref]
- He S, Chen X, Zhou X, et al. Sudden death due to traumatic ascending aortic pseudoaneurysms ruptured into the esophagus: 2 case reports. Medicine (Baltimore) 2015;94:e716. [Crossref]
- Tsutsui H, Ikeda N. Tracheal resection for the treatment of thyroid cancer invading the trachea--circumferential sleeve resection followed by end-to-end anastomosis. Nihon Geka Gakkai Zasshi 2012;113:469-71.
- Tanaka A, Miyajima M, Obama T, et al. Thoracic surgery for the penetrating lung or tracheal trauma. Kyobu Geka 2006;59:1018-22.
- Grillo HC, Dignan EF, Miura T. Extensive resection and reconstruction of mediastinal trachea without prosthesis or graft: an anatomical study in man. J Thorac Cardiovasc Surg 1964;48:741-9.
- Cai RJ, Mu F, Chen G, et al. Diagnosis and treatment of traumatic tracheobronchial ruptures: report of 17 cases. Di Yi Jun Yi Da Xue Xue Bao 2003;23:177-8.
- Ariyama J, Nakamura C, Nakagawa H, et al. Case of perioperative tracheal laceration by electrocautery. Masui 2013;62:1422-5.
- Brass P, Hellmich M, Ladra A, et al. Percutaneous techniques versus surgical techniques for tracheostomy. Cochrane Database Syst Rev 2016;7:CD008045.
- Talekar CR, Udy AA, Boots RJ, et al. Tracheal cuff pressure monitoring in the ICU: a literature review and survey of current practice in Queensland. Anaesth Intensive Care 2014;42:761-70.
- Demirel CB, Haltaş H, Pampal HK, et al. Comparison of the effects of different percutaneous tracheotomy techniques on acute tracheal trauma. Turk J Med Sci 2014;44:68-72. [Crossref]