Evolutional trends in the management of tracheal and bronchial injuries
Introduction
Tracheal and tracheobronchial injuries are rare, but serious consequences of blunt trauma, penetrating wounds and iatrogenic injuries associated with endotracheal intubation and mechanical ventilatory support and with endobronchial intervention including airway dilatation (1-3).
The incidence of these complications is not known, although a study reported a total of 1,033 tracheal injuries over a 5-year period in Germany (1). A total of 429 of these were non-iatrogenic (blunt trauma 276, penetrating wounds 94, bullet wounds 16, other aetiologies 43) and 604 of these injuries were iatrogenic (endotracheal intubation/mechanical ventilation 372, dilatational tracheostomy 181, endoscopic interventions 51). Another study reviewed the world literature on blunt intrathoracic tracheobronchial injuries and identified 265 patients (4).
Blunt trauma is a major cause of death from thoracic trauma (4). Although it is believed that over 80% of patients who sustain blunt traumatic tracheal or bronchial injury die before arriving at hospital (5,6), post-mortem findings suggest an incidence of 2.8% of tracheobronchial injuries in patients who die following blunt chest trauma (7). Often, the right main bronchus is affected more than the left perhaps as a consequence of relative protection of the left main bronchus afforded by the aorta (8).
Tracheobronchial injuries can be transverse between tracheal rings or may be longitudinal or spiral across the membranous portion of the trachea and main bronchi or indeed may present with a combination of both type of injuries (9).
Typically, in iatrogenic injuries, a longitudinal running defect in the posterior wall is encountered (1,10-13). This may be more common, in my opinion, when a bougie is employed for patients when endotracheal tube insertion is difficult.
It is appreciated that although tracheobronchial injuries are rare, the number of patients who sustain these injuries will be encountered more frequently in clinical practice. This will reflect the increasing numbers of patients who sustain traumatic injuries in the community who survive to hospital admission, thanks to improved pre-hospital medical care. Furthermore, with the expanding development of percutaneous tracheostomy techniques in intensive care units and the expansion of endobronchial intervention services worldwide, it is likely that further iatrogenic injuries will occur (14,15). Therefore, familiarity with techniques to successfully manage these patients among Surgical, Emergency Medical and Intensive Care Teams and Anaesthetists is becoming increasingly important.
Diagnosis
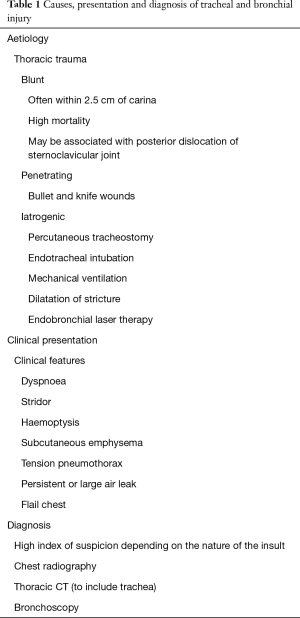
It is important to have a high index of suspicion for tracheobronchial injuries among patients who have sustained thoracic injury (blunt on penetrating) or who may have experienced iatrogenic injury at the time of endotracheal intubation/mechanical ventilation or following large airway intervention (Table 1).
Full table
Typical clinical features will include stridor, dyspnoea, haemoptysis, subcutaneous emphysema, tension pneumothorax and persistent or large air leak, which will mandate the deployment of one or more chest tubes or indeed urgent surgical intervention. The patient may have a flail chest.
Routine investigations include chest radiography, thoracic CT scan (to include the trachea) and bronchoscopy. In patients who have non iatrogenic traumatic injury it must be appreciated that other injuries may co-exist, e.g., to the oesophagus, lung parenchyma, heart and great vessels, brain, abdomen etc. Injuries are diagnosed and prioritised and several teams may be involved in patient management.
Rigid and flexible bronchoscopy is used to confirm the diagnosis of the injury and to determine its extent and to define its anatomy. High-frequency jet ventilation or low tidal volume using a Sanders injector is given to minimise additional airway injury and subcutaneous emphysema while the airway injury is inspected and defined (10-13,16,17). While considering treatment strategies, the rigid bronchoscope is passed beyond the injury and a Bougie is deployed in the main bronchus. The rigid bronchoscope is removed and an endotracheal tube is inserted over the Bougie to ensure that it bypasses the defect. The position of the tube is then confirmed with a flexible bronchoscope. It may be necessary to consider deployment of a dual-lumen endotracheal tube depending on the location and extent of the airway injury.
Treatment options
Surgery
As these complications are rare, it is quite possible that the attending teams may not have the surgical capabilities to manage these patients. Under such circumstances, prompt early discussion with Specialist Centres and urgent transfer if and when the patient is deemed suitable for surgical intervention should be made. However, it may be that the patients have other significant comorbidities which would render their tolerability of formal surgical intervention prohibitive or transfer may not be possible and therefore other avenues may have to be pursued.
Surgical approaches include thoracotomy, sternotomy, clamshell incision and cervical incision. For tracheal separation, previous authors have described passing the endotracheal tube across the lacerated trachea and completing the repair over the endotracheal tube and this has also been used for incomplete tears. For main bronchial lacerations, selective intubation of the non-injured main bronchus is usually performed and injuries are repaired completely. A variety of different techniques to surgically manage these patients has been described (1-8,18-21).
Techniques described for managing complete tracheal transection involve passing an endotracheal tube across the injured area and completing the repair over the tube. A dual lumen tube or selective intubation of the injured side can be used to manage patients with a main bronchial injury (18). The same approach has been used in both blunt and penetrating injuries. Primary repair with end to end anastomosis using non-absorbable (e.g., Prolene) suture is preferred for circumferential injury. Perioperative sepsis must be aggressively managed. Devitalised tissue is removed, primary closure without tension is performed and vascular supply to the wound edges is preserved as much as possible (19). Postoperative airway stenosis (18) or dehiscence may occur. Surgical mortality of 4–30% has been reported (18-21) and early surgical intervention (within two hours of trauma) may influence outcome (18). Mortality appears to be higher among patients with blunt rapture (18). However, these injuries are rare and not all surgeons have ongoing still in their management. Furthermore patients may have other diverse injuries within the confines of their trauma which may influence outcome. This must be borne in mind when considering the indications for, and outcomes of, surgery.
Endobronchial techniques
It is not always possible to perform primary surgical repair either because of coexistent comorbidities, multiple associated trauma injuries, patient instability to facilitate transfer or lack of local expertise. Under such circumstances, endobronchial manoeuvres are being increasingly explored. A rigid and flexible bronchoscope can be inserted into the airway and ventilatory support can be applied as described above. A covered expandable metallic stent can be inserted into the airway and an endotracheal tube (or if appropriate a tracheostomy tube) can be positioned to lie within the stent using a fiberoptic bronchoscope. The fiberoptic bronchoscope is passed through the endotracheal tube or the tracheostomy tube and is then inserted into the stent allowing for the definitive airway to be placed with confidence into the centre of the stent over the bronchoscope itself (22). We have had encouraging experience in managing patients in this fashion, where the stent has acted as a scaffold to promote tissue healing. Bronchial toilet is essential and antibiotic therapy is prescribed to provide prophylaxis against or to treat intercurrent infection with close ongoing communication with microbiologists and prospective microbiological surveillance.
For tears, less than 5 mm diameter, it may be possible to seal the defect by direct application of BioGlue (CryoLife Europa, UK) applied directly using pledgets (23).
Over the past 5 years, 10 patients were referred to our unit with traumatic or iatrogenic tracheal tears. All patients were managed by the cardiothoracic intensive care unit team. Formal surgical repair was contraindicated for each patient on account of significant medical co-morbidities. Five patients were treated with endotracheal stenting (3 patients) and with the application of Bio Glue (2 patients). Four (80%) of these patients survived. The other five patients had sustained a large tear (>2 cm length) and were managed conservatively. Three of these patients died of sepsis and 2 (40%) survived.
Conclusions
Although rare, it is believed that an increasing number of patients with tracheal and bronchial injuries will be seen in hospital as a consequence of improvement in prehospital medical care and the expansion in percutaneous tracheostomy insertions and large airway intervention techniques. Thus increasing awareness of the aetiology, diagnosis and management of patients with these complications is necessary for emergency medical and surgical teams, anaesthetists and these involved in intensive care. Traditionally surgical intervention has been the main management strategy but the encouraging results of endobronchial techniques suggests that such an approach should be considered for all high-risk candidates with tracheal defects in the region of 1.5 cm or less.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Schneider T, Volz K, Dienemann H, et al. Incidence and treatment modalities of tracheobronchial injuries in Germany. Interact Cardiovasc Thorac Surg 2009;8:571-6. [Crossref]
- Borasio P, Ardissone F, Chiampo G. Post-intubation tracheal rupture. A report on ten cases. Eur J Cardiothorac Surg 1997;12:98-100. [Crossref]
- Massard G, Rougé C, Dabbagh A, et al. Tracheobronchial lacerations after intubation and tracheostomy. Ann Thorac Surg 1996;61:1483-7. [Crossref]
- Kiser AC, O'Brien SM, Detterbeck FC. Blunt tracheobronchial injuries: treatment and outcomes. Ann Thorac Surg 2001;71:2059-65. [Crossref]
- Ecker RR, Libertini RV, Rea WJ, et al. Injuries of the trachea and bronchi. Ann Thorac Surg 1971;11:289-98. [Crossref]
- Kummer C, Netto FS, Rizoli S, Yee D. A review of traumatic airway injuries: potential implications for airway assessment and management. Injury 2007;38:27-33. [Crossref]
- Bertelsen S, Howitz P. Injuries of the trachea and bronchi. Thorax 1972;27:188-94. [Crossref]
- Symbas PN, Justicz AG, Ricketts RR. Rupture of the airways from blunt trauma: treatment of complex injuries. Ann Thorac Surg 1992;54:177-83. [Crossref]
- Chu CP, Chen PP. Tracheobronchial injury secondary to blunt chest trauma: diagnosis and management. Anaesth Intensive Care 2002;30:145-52.
- Eruchie C, Ramsay M, Madden B. Should Endoscopic Tracheal Techniques Be Considered as First Line Management in High Risk Patients with Appropriate Extended Tracheal Injury? American Thoracic Society 2015;Abstract A3723.
- Madden B, Datta S, Hussain I, et al. Tracheal stenting for rupture of the posterior wall of the trachea following percutaneous tracheostomy. Monaldi Arch Chest Dis 2001;56:320-1.
- Madden BP, Sheth A, Ho TB, et al. Novel approach to management of a posterior tracheal tear complicating percutaneous tracheostomy. Br J Anaesth 2004;92:437-9. [Crossref]
- Creagh-Brown B, Sheth A, Crerar-Gilbert A, et al. A novel approach to the management of acute tracheal tear. J Laryngol Otol 2008;122:1392-3. [Crossref]
- Bacon JL, Wilde MP, Walker ME, et al. The Diagnosis of Large Airway Pathology and the Role of Rigid Bronchoscopy. Current Respiratory Medicine Reviews 2013;9:11-25. [Crossref]
- Bacon JL, Patterson CM, Madden BP. Indications and interventional options for non-resectable tracheal stenosis. J Thorac Dis 2014;6:258-70.
- Madden BP, Sheth A, Ho TB, et al. A novel approach to the management of persistent postpneumonectomy bronchopleural fistula. Ann Thorac Surg 2005;79:2128-30. [Crossref]
- Davis N, Madden BP, Sheth A, et al. Airway management of patients with tracheobronchial stents. Br J Anaesth 2006;96:132-5. [Crossref]
- Balci AE, Eren N, Eren S, et al. Surgical treatment of post-traumatic tracheobronchial injuries: 14-year experience. Eur J Cardiothorac Surg 2002;22:984-9. [Crossref]
- Sulek M, Miller RH, Mattox KL. The management of gunshot and stab injuries of the trachea. Arch Otolaryngol 1983;109:56-9. [Crossref]
- Ramzy AI, Rodriguez A, Turney SZ. Management of major tracheobronchial ruptures in patients with multiple system trauma. J Trauma 1988;28:1353-7. [Crossref]
- Flynn AE, Thomas AN, Schecter WP. Acute tracheobronchial injury. J Trauma 1989;29:1326-30. [Crossref]
- Jones C, Crerar-Gilbert AJ, Madden BP. Anaesthesia for endobronchial intervention and tracheobronchial stents. Curr Anaesth Crit Care 2009;20:160-3. [Crossref]
- Ranu H, Gatheral T, Sheth A, et al. Successful endobronchial seal of surgical bronchopleural fistulas using BioGlue. Ann Thorac Surg 2009;88:1691-2. [Crossref]


