Pulmonary sequestration mimicking a pancreas herniation in a case of recurrent Bochdalek hernia
Introduction
Bochdalek hernia is the most common congenital diaphragmatic hernia (CDH) but remains rare (incidence: 1/2,500 live births) (1). It is caused by a defect in the latero-posterior pleuroperitoneal compartment which can lead to herniation of abdominal organs into the thorax (1). Herniations of stomach, greater omentum, liver, spleen, colon, small bowels, or pancreas through CDH have been previously described. In neonates, liver herniation is related to a worse prognosis (2). This is why this defect is specifically searched in the pre-/postnatal ultrasound. In adults, herniation of abdominal organs in CDH can cause pain or gastrointestinal symptoms, whereas in newborns respiratory distress is the most often present symptom.
Pulmonary sequestration (PS) is a congenital pulmonary malformation with arterial supply arising from systemic arteries that can originate from the abdomen or thorax independently of the standard pulmonary blood supply (3). PS results in lung tissue that is not connected to the tracheobronchial tree. PS represents between 0.15% and 6.5% of all congenital pulmonary malformations (4).
We report a case of recurrent CDH associated with abdominal pain and an image mimicking pancreatic tail herniation through the thorax in an 18-year-old patient. The patient was managed surgically, and it was found that the radiological image corresponded to a PS with arterial supply originating from the celiac trunk.
Case presentation
An 18-year-old patient presented with a 2-month history of left flank pain, dyspnea, nausea and vomiting. He underwent surgery via laparotomy for a CDH 2 days after birth. The hernia recurred 14 years later with kidney herniation causing hydronephrosis which was treated by nephrectomy and hernia repair with dura mater patch done by laparotomy. The remaining medical history was irrelevant apart from a hyperactivity disorder treated by methylphenidate.
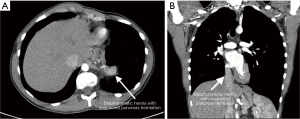
A CT-scan revealed a left-posterior CDH with an image consistent with a pancreatic tail and omentum majus herniation (Figure 1).
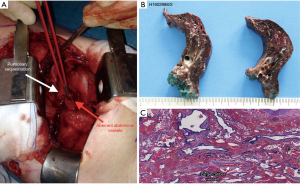
Redo surgery was performed via a left postero-lateral thoracotomy. Intraoperatively, fatty tissue bulging through the CDH recurrence was found as well as a solid compact mass with a vascular pedicle originating from the celiac trunk (Figure 2A). After careful dissection, the greater omentum was replaced in the abdomen through the diaphragmatic foramen. The solid mass was resected and sent for pathological analysis. The defect was closed by a Prolene mesh that was sutured circumferentially around the orifice. The anatomopathology report confirmed the presence of greater omentum and of an extralobar PS (7 cm) containing systemic arterialization (Figure 2B,C). The histologic exam showed that the PS was encircled by its own visceral pleura.
The postoperative course was marked by an ipsilateral pneumonia that was successfully treated with amoxicillin and clavulanic acid for 7 days. The patient was discharged on postoperative day 9.
Discussion
This case reports a rare case of greater omentum herniation through a recurrent CDH incorporating a concomitant extralobar PS.
Recurrence of CDH has a 10−20% incidence after surgical repair (5). Recurrences mainly depend on the diaphragmatic defect size, on the repair technique (open/minimally invasive, primary closure, patch use, or muscle flap), and on the follow-up length (6). Once diagnosed CDH should be managed surgically to avoid complications such as ileus, volvulus, or organ strangulation related to herniation. Operative treatment of this congenital hernia can be undertaken either by laparotomy/laparoscopy or thoracotomy/thoracoscopy. Each technique has its own advantages. An abdominal approach is generally suggested as it allows a good control and reposition of the abdominal organs and has interesting mesh placement capacities. However, CDH thoracic approaches are thought to be more effective as they allow better diaphragm repair, especially in recurrence case.
PS is characterized by congenital non-functional lung tissue with aberrant systemic vascularization usually from the thoracic/abdominal aorta (4). In the present case, the vascularization originated from the celiac trunk, and three arteries were found in the histopathology report. Moreover, PS can be intra- or extralobar depending on whether or not the sequestration has its own pleural envelope. In this patient, the PS was extralobar, and the visceral pleura were attached to the herniated greater omentum by fibrous tissue. Extralobar PS can be associated with other anomalies including CDH, congenital pulmonary airway malformation, pulmonary hypoplasia, congenital lobar emphysema, bronchogenic cyst, congenital heart disease, vertebral anomalies, or intestinal duplications. It is important to be aware of the association between PS and CDH. Early recognition of PS in a stable patient with CDH allows resection of an extralobar PS at the same time as the CDH repair, which can prevent a subsequent operation for an incidentally found mediastinal mass later in life. In 15−30% of CDH patients PS will also be present. PS have previously been reported to cause recurrent infections, hemoptysis, and pain. In the present case, the patient symptoms were completely relieved after surgery. In addition, this case highlights the misleading radiological image of pancreas herniation while it corresponded to PS.
This case report emphasizes that surgeons should be prepared to encounter other unsuspected findings intraoperatively. In case of CDH, one should look for a PS during CDH repair as the association between these two pathologies is quite frequent. This case report also shows that CT-scan can be misleading to diagnose the intrathoracic content of a diaphragmatic hernia.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- de Buys Roessingh AS, Dinh-Xuan AT. Congenital diaphragmatic hernia: current status and review of the literature. Eur J Pediatr 2009;168:393-406. [Crossref]
- Kays DW, Talbert JL, Islam S, et al. Improved Survival in Left Liver-Up Congenital Diaphragmatic Hernia by Early Repair Before Extracorporeal Membrane Oxygenation: Optimization of Patient Selection by Multivariate Risk Modeling. J Am Coll Surg 2016;222:459-70. [Crossref]
- Corbett HJ, Humphrey GM. Pulmonary sequestration. Paediatr Respir Rev 2004;5:59-68. [Crossref]
- Halkic N, Cuénoud PF, Corthésy ME, et al. Pulmonary sequestration: a review of 26 cases. Eur J Cardiothorac Surg 1998;14:127-33. [Crossref]
- Nagata K, Usui N, Terui K, et al. Risk factors for the recurrence of the congenital diaphragmatic hernia-report from the long-term follow-up study of Japanese CDH study group. Eur J Pediatr Surg 2015;25:9-14.
- Chan E, Wayne C, Nasr A. Minimally invasive versus open repair of Bochdalek hernia: a meta-analysis. J Pediatr Surg 2014;49:694-9. [Crossref]


