Uniportal video-assisted thoracic surgery: the Middle East experience
Introduction
The introduction of video-assisted thoracic surgery (VATS) into the surgical armamentarium of the past two decades has changed the face of thoracic surgery. The field has moved from the traditional extensive thoracotomy to a minimally invasive video-based approach for a wide array of pathologies with improved results, shorter hospital stays, less pain and reduced costs (1-4). VATS technique reduced surgical trauma and maintains the same oncological principles of traditional open procedures (5-8). Due to its minimally invasive nature and shorter recovery, some groups have demonstrated an improved tolerance to adjuvant chemotherapy. VATS originated with the application of a 1–3 trocar incisions as well as a utility incision for major lung resections (4,5,9). Yamamoto et al. (10) first reported the initial experience of uniportal VATS in a series of six patients. This work was followed by Rocco and his group at the National Cancer Institute in Naples, Italy (11-15). Rocco reported his initial experience over the period of 2003–2006 for a wide variety of pathologies including pleural effusion, pleurodesis, biopsies, wedge resection and mediastinal pathologies. The real breakthrough and milestone for this technique was by Dr. Gonzalez-Rivas at University of a Coruña, Spain who performed the first major lung resection with radical lymphadenectomy for non-small-cell lung cancer (NSCLC) (16). Dr. Gonzalez-Rivas went on to perform complex procedures such as segmentectomies, pneumonectomies, sleeve vascular and bronchoplastic resections, and chest wall resections (17-27). Management of significant bleeding proved to be safe in experts’ hands with this technique (28,29). The most recent development was uniportal lobectomy in a non-intubated patient (30,31). Implementation of uniportal VATS technique is gaining wide and rapid application across the globe with initial very positive outcomes (27,32-41). Long-term data are still awaited. The purpose of this study was to analyze the initial experience with uniportal VATS performed in Israel.
Methods
One hundred ninety two [192] cases of uniportal VATS were performed between November 2013 and June 2016. A retrospective study from prospectively collected data from our institutional database was carried out for patients undergoing a uniportal VATS procedure. The results are analyzed and are included in this study. The results of postoperative pain level are also analyzed in the first 90 patients. The review board at the Shaare Zedek University Hospital, Jerusalem, Israel, approved this study. The main endpoint of this study was feasibility of technique, postoperative pain level, 30-day mortality, morbidity, and conversion rate.
Surgical technique
(I) All operations were done under general anesthesia utilizing a double-lumen tube or bronchial blocker for intraoperative single-lung ventilation. Positioning of the lung isolation device was guided by flexible bronchoscope. Double-lumen tube was preferable in right sided lung resections because it provides better lung deflation during intraoperative lung manipulations. An arterial line is usually used in major procedures for hemodynamic and arterial blood gas monitoring. Peripheral intravenous lines were employed for fluid and drug administration. In major surgeries, Foley catheter was inserted. In the majority of cases, paravertebral block was performed by our anesthesia colleagues prior to the induction of anesthesia; alternatively, intercostal block was performed by the surgeon intraoperatively. We rarely placed an epidural catheter.
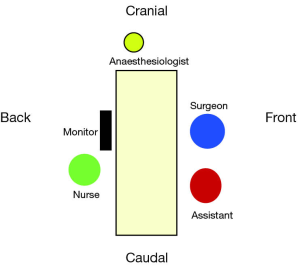
(II) The patient is placed in a lateral decubitus position, both arms along the body (prayer’s position) (Figure 1) with the bed maximally flexed and the breakpoint just above the superior iliac crest. This helps spread the intercostal spaces.
Both the surgeon and the assistant are positioned in front of the patient in order to have the same thoracoscopic vision during all steps of the procedure, thus allowing more coordinated movements. The scrub nurse should be positioned behind the patient (Figure 2).
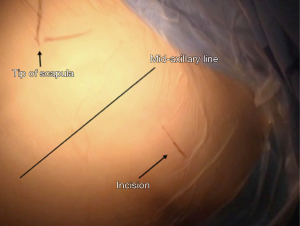
A 3–5 cm incision is performed preferably in the 5th intercostal space in the anterior axillary line area (Figure 3). This location provides better approach for hilar dissection and insertion of staplers, in some cases when approaching the anterior mediastinum (e.g., pericardial window) the incision was made a little bit more posterior than usual. This can provide better exposure and comfort for the surgeon to deal with the anterior mediastinum.
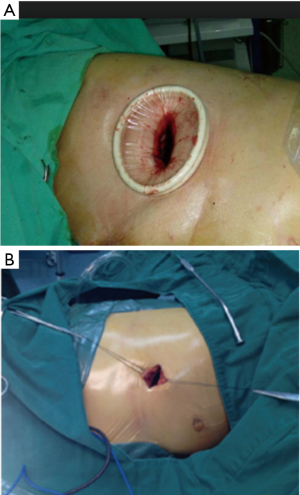
In this procedure, there was no need to use a rib spreader or thoracoscopic trocar. In most of the cases a wound protector (Figure 4A) could be helpful in obese patients or according to surgeon preference. Retracting the wound using two stitches, one from each side, could also be helpful, especially for opening the wound and to avoid contamination of the camera (Figure 4B).
The thoracoscope (preferably 10 mm 30 degrees) should be inserted and maintained in the posterior part of the incision. Eleven sympathectomy operations (5.7%) were done with single lumen tube using a 0 degree thoracoscope with working channel introduced through a small incision at the mid axillary line of the base of axilla with insufflation of CO2 during the surgery.
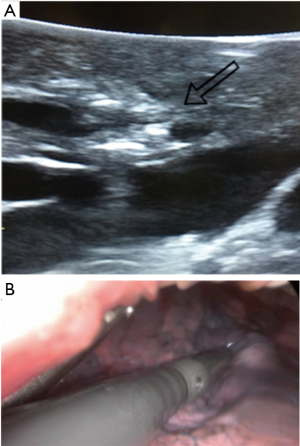
All operations were conducted using this methodology with the exception of one case. No additional incisions were made for any purpose such as drain placement, or further instrumentation. A complete lymphadenectomy was carried out in all cases of lung cancer. Digital palpation of nodules when necessary was smoothly carried out through the incision, but in cases with small lesions or GGO (14 cases) we used intraoperative ultrasonography to identify the lesions (Figures 5,6). All tumor specimens were removed from the chest using a retrieval bag. At the end of surgery a single 20–28 Fr chest tube was inserted and secured into position at the posterior part of the incision.
Postoperative management
Post-operative management included a fast-track concept designed by our department. Most patients were transferred to a regular ward after a brief period in the general recovery ward (PACU). Some high-risk patients recovered overnight in an ICU. Mobilization and respiratory physiotherapy began in the overwhelming majority of patients on the operation day. Most patients did not receive epidural catheter for pain management and received oral pain medications. Chest X-ray was performed on the day of surgery, on the first postoperative day and after chest tube removal prior to discharge. Chest tube removal occurred with normal CXR findings, no air leak and secretions of less than 250 cc in 24 hours. No patient was discharged with a chest tube in place.
Results
Spectrum of procedures
Uniportal VATS technique has been adopted in the cardiothoracic surgery department at Shaare Zedek Medical Center (SZMC) in November 2013. Between November 2013 and June 2016 we performed 192 procedures using the uniportal VATS technique. Patients ages were between 12–83 years (mean age 49.6 years) and 72 patients (37%) were female. Anatomical resections numbered 35 (18% of cases) which included 31 lobectomies, 2 segmentectomies, 2 pneumonectomies (Table 1).
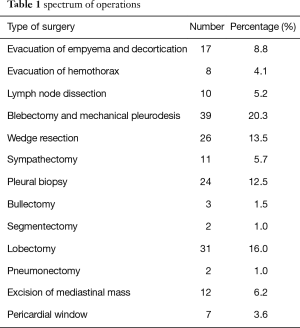
Full table
Perioperative mortality and morbidity
There was no operative or 30-day mortality. For 35 cases of anatomical resection, conversion to anterolateral thoracotomy occurred in 3 cases (8%), one case due to significant bleeding and two cases due to technical difficulties. Conversion to multiple port VATS was done in one case due to technical difficulties. Six patients (3%) had a prolonged air leak for more than 4 days. Three patients (1.5%) were after decortication and evacuation of empyema while the other 3 patients (1.5%) were after anatomical resections. The average chest drain duration was 3.25 days (1–23 days) and the average length of stay was 4.2 days (1–25 days). Three patients (1.5%) underwent re-exploration due to postoperative bleeding. One patient (0.5%) with stage 4 lung cancer underwent decortication and evacuation of empyema which developed after insertion of a long-term palliative chest drain (pleurx catheter; PleurX™). This patient required reintubation for one week due to severe acute respiratory distress syndrome (ARDS) (Table 2).
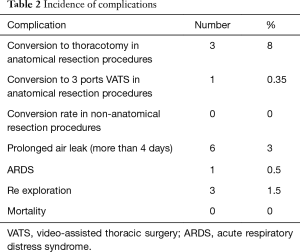
Full table
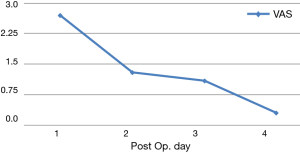
Postoperative pain was retrospectively analyzed in the first 90 patients during the first four postoperative days (Figure 7). According to visual analog scale (VAS), the average level of pain was 2.7 on POD 1 and dropped to 0.3 by the morning of POD 4.
Discussion
Uniportal VATS is being applied worldwide for both minor and major lung and mediastinal resections. Its feasibility has been established with several publication demonstrating excellent early outcomes. To date there have not been any randomized controlled prospective studies comparing uniportal VATS to conventional VATS or to open thoracotomy. However, there have been several recent publications comparing uniportal VATS to traditional VATS and open thoracotomies that have shown advantages of uniportal technique. Uniportal VATS lung resection is feasible. It allows for complete resection of the lung according to cancer operation principles, and has reduced length of stay, has reduced cost and improved patient satisfaction.
The uniportal VATS program began at our institution in November 2013 with the assistance and guidance of Dr. Gonzalez-Rivas. The operations were performed according to availability of instrumentation designed to facilitate the technique and taking into account the learning-curve and experience of the thoracic surgeon. Over time we have undertaken more complex surgical resections including segmentectomy and pneumonectomy, and have reduced our operative times.
Our report represents the first Middle Eastern experience with uniportal VATS surgery for a heterogeneous group of patients, undergoing a variety of surgical procedure both simple and complex resection with excellent early results, low conversion rate to either traditional multi incision VATS or thoracotomy and minimal morbidity.
Uniportal VATS technique can be optimally learned under the supervision of a team proficient and experienced surgeon. Adoption of this technique was facilitated by usage of surgical instruments designed to be of low profile relative to traditional VATS instruments, excellent anesthetic management, teamwork and application of good postoperative management. Further randomized controlled studies are necessary to compare uniportal VATS with other techniques in terms of lymph node dissection, postoperative pain, length of stay as well as mid and long-term results. Uniportal VATS technique is an emerging tool in the thoracic surgery armamentarium.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the review board at the Shaare Zedek University Hospital, Jerusalem, Israel (Helsinki Committee approval number: 0096-16-SZMC) and written informed consent was obtained from all patients.
References
- Roviaro G, Rebuffat C, Varoli F, et al. Videoendoscopic pul- monary lobectomy for cancer. Surg Laparosc Endosc 1992;2:244-7. [PubMed]
- McKenna RJ Jr, Houck W, Fuller CB. Video-assisted thoracic surgery lobectomy: experience with 1,100 cases. Ann Thorac Surg 2006;81:421-5. [Crossref] [PubMed]
- Daniels LJ, Balderson SS, Onaitis MW, et al. Thoracoscopic lobectomy: a safe and effective strategy for patients with stage I lung cancer. Ann Thorac Surg 2002;74:860-4. [Crossref] [PubMed]
- Balderson SS, D'Amico TA. Thoracoscopic lobectomy for the management of non-small cell lung cancer. Curr Oncol Rep 2008;10:283-6. [Crossref] [PubMed]
- Wang BY, Liu CY, Hsu PK, et al. Single-incision versus multiple-incision thoracoscopic lobectomy and segmentectomy: a propensity-matched analysis. Ann Surg 2015;261:793-9. [Crossref] [PubMed]
- Hazelrigg SR, Nunchuck SK, Landreneau RJ, et al. Cost analysis for thoracoscopy: thoracoscopic wedge resection. Ann Thorac Surg 1993;56:633-5. [Crossref] [PubMed]
- Lacin T, Swanson S. Current costs of video-assisted thoracic surgery (VATS) lobectomy. J Thorac Dis 2013;5 Suppl 3:S190-3. [PubMed]
- Zhang Z, Zhang Y, Feng H, et al. Is video-assisted thoracic surgery lobectomy better than thoracotomy for early-stage non-small-cell lung cancer? A systematic review and meta-analysis. Eur J Cardiothorac Surg 2013;44:407-14. [Crossref] [PubMed]
- Nesher N, Galili R, Sharony R, et al. Videothorascopic sympathectomy (VATS) for palmar hyperhidriosis: summary of a clinical trial and surgical results. Harefuah 2000;138:913-6,1008. [PubMed]
- Yamamoto H, Okada M, Takada M, et al. Video-assisted thoracic surgery through a single skin incision. Arch Surg 1998;133:145-7. [Crossref] [PubMed]
- Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg 2004;77:726-8. [Crossref] [PubMed]
- Rocco G, Khalil M, Jutley R. Uniportal video-assisted thoracoscopic surgery wedge lung biopsy in the diagnosis of interstitial lung diseases. J Thorac Cardiovasc Surg 2005;129:947-8. [Crossref] [PubMed]
- Jutley RS, Khalil MW, Rocco G. Uniportal vs standard three-port VATS technique for spontaneous pneumothorax: comparison of post-operative pain and residual paraesthesia. Eur J Cardiothorac Surg 2005;28:43-6. [Crossref] [PubMed]
- Rocco G, Romano V, Accardo R, et al. Awake single-access (uniportal) video-assisted thoracoscopic surgery for peripheral pulmonary nodules in a complete ambulatory setting. Ann Thorac Surg 2010;89:1625-7. [Crossref] [PubMed]
- Rocco G, Martucci N, La Manna C, et al. Ten-year experience on 644 patients undergoing single-port (uniportal) video-assisted thoracoscopic surgery. Ann Thorac Surg 2013;96:434-8. [Crossref] [PubMed]
- Gonzalez D, Delgado M, Paradela M, et al. Uni-incisional video-assisted thoracoscopic left lower lobectomy in a patient with an incomplete fissure. Innovations (Phila) 2011;6:45-7. [Crossref] [PubMed]
- Sihoe AD. The evolution of minimally invasive thoracic surgery: implications for the practice of uniportal thoracoscopic surgery. J Thorac Dis 2014;6:S604-17. [PubMed]
- Gonzalez-Rivas D, de la Torre M, Fernandez R, et al. Single-port video-assisted thoracoscopic left upper lobectomy. Interact Cardiovasc Thorac Surg 2011;13:539-41. [Crossref] [PubMed]
- Gonzalez-Rivas D, Paradela M, Fernandez R, et al. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg 2013;95:426-32. [Crossref] [PubMed]
- Gonzalez-Rivas D, de la Torre M, Fernandez R, et al. Video: Single-incision video-assisted thoracoscopic right pneumonectomy. Surg Endosc 2012;26:2078-9. [Crossref] [PubMed]
- Gonzalez-Rivas D. Single port video-assisted thoracoscopic lobectomy and chest wall resection by posterior incision. Innovations 2012;7:81-4.
- Gonzalez-Rivas D, Mendez L, Delgado M, et al. Uniportal video-assisted thoracoscopic anatomic segmentectomy. J Thorac Dis 2013;5 Suppl 3:S226-33. [PubMed]
- Gonzalez-Rivas D, Yang Y, Stupnik T, et al. Uniportal video-assisted thoracoscopic bronchovascular, tracheal and carinal sleeve resections. Eur J Cardiothorac Surg 2016;49 Suppl 1:i6-16. [PubMed]
- Gonzalez-Rivas D, Delgado M, Fieira E, et al. Double sleeve uniportal video-assisted thoracoscopic lobectomy for non-small cell lung cancer. Ann Cardiothorac Surg 2014;3:E2. [PubMed]
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Uniportal video-assisted thoracoscopic sleeve lobectomy and other complex resections. J Thorac Dis 2014;6:S674-81. [PubMed]
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Uniportal video-assisted thoracoscopic lobectomy. J Thorac Dis 2013;5 Suppl 3:S234-45. [PubMed]
- Gonzalez-Rivas D. VATS lobectomy: surgical evolution from conventional VATS to uniportal approach. Scientific World Journal 2012;2012:780842.
- Gonzalez-Rivas D, Stupnik T, Fernandez R, et al. Intraoperative bleeding control by uniportal videoassisted thoracoscopic surgery. Eur J Cardiothorac Surg 2016;49 Suppl 1:i17-24. [PubMed]
- Abu Akar F, Gonzalez-Rivas D, Fink D. Management of bleeding from an abnormally located S6 arterial branch in a common origin with S2 branch during live surgery. J Vis Surg 2016;2:87. [Crossref]
- Gonzalez-Rivas D, Bonome C, Fieira E, et al. Non-intubated video-assisted thoracoscopic lung resections: the future of thoracic surgery? Eur J Cardiothorac Surg 2016;49:721-31. [Crossref] [PubMed]
- Gonzalez-Rivas D, Fernandez R, de la Torre M, et al. Single-port thoracoscopic lobectomy in a nonintubated patient: the least invasive procedure for major lung resection? Interact Cardiovasc Thorac Surg 2014;19:552-5. [Crossref] [PubMed]
- Gonzalez-Rivas D, Yang Y, Ng C. Advances in Uniportal Video-Assisted Thoracoscopic Surgery: Pushing the Envelope. Thorac Surg Clin 2016;26:187-201. [Crossref] [PubMed]
- Scarci M, Zahid I, Billé A, et al. Is video-assisted thoracoscopic surgery the best treatment for paediatric pleural empyema? Interact Cardiovasc Thorac Surg 2011;13:70-6. [Crossref] [PubMed]
- Ng CS, Gonzalez-Rivas D, D'Amico TA, et al. Uniportal VATS-a new era in lung cancer surgery. J Thorac Dis 2015;7:1489-91. [PubMed]
- Bertolaccini L, Rocco G, Viti A, et al. Geometrical characteristics of uniportal VATS. J Thorac Dis 2013;5 Suppl 3:S214-6. [PubMed]
- Drevet G, Ugalde Figueroa P. Uniportal video-assisted thoracoscopic surgery:safety, efficacy and learning curve during the first 250 cases in Quebec, Canada. Ann Cardiothorac Surg 2016;5:100-6. [Crossref] [PubMed]
- Shen Y, Liu Y, Feng M, et al. Uniportal video-assisted thoracoscopic lobectomy: Zhongshan experience. J Vis Surg 2015;1:5.
- Ismail M, Helmig M, Swierzy M, et al. Uniportal VATS: the first German experience. J Thorac Dis 2014;6:S650-5. [PubMed]
- Ng CS. Uniportal VATS in Asia. J Thorac Dis 2013;5:S221-5. [PubMed]
- Guido Guerrero W, Gonzalez-Rivas D, Hernandez Arenas LA, et al. Techniques and difficulties dealing with hilar and interlobar benign lymphadenopathy in uniportal VATS. J Vis Surg 2016;2:23.
- Ng CS, Lau KK, Gonzalez-Rivas D, et al. Evolution in surgical approach and techniques for lung cancer. Thorax 2013;68:681. [Crossref] [PubMed]
- Abu Akar F, Gonzalez-Rivas D, Ismail M, et al. Using Intra-operative Ultrasonography for finding small lung lesions. Asvide 2017;4:064. Available online: http://www.asvide.com/articles/1363