The influence of chest tube size and position in primary spontaneous pneumothorax
Introduction
Initial management of symptomatic primary spontaneous pneumothorax (PSP) is evacuation of air from the pleural space by placement of a chest tube or by simple aspiration. The British Thoracic Society guidelines from 2010 recommend that the tip of the inserted chest tube or a pigtail catheter should be positioned at the top and front of the pleural cavity because it is assumed that this location is the most optimal (1). This assumption, however, has not been scientifically documented. Furthermore, it is uncertain whether treatment of a simple pneumothorax is influenced by chest tube drainage by pigtail catheters or surgical chest tubes.
According to the American College of Chest Physicians (2) a large PSP can be managed with a small-bore pleural catheter (≤14 French catheter) or a chest tube (16–22 Fr catheter). These guidelines also state that 24–28 Fr surgical chest tubes are only required if the patient is suspected to have a bronchopleural fistula with a large air leak or if the patient requires positive-pressure ventilation. Never the less, large surgical chest tubes are still used routinely in many centres worldwide for the treatment of simple pneumothorax as this decision is most often left to the surgeon but it may also depend on local tradition. Previous studies showed that pigtail catheters or small-bore catheters are equivalent with larger surgical chest tubes for the treatment of spontaneous pneumothorax (3-5), but they all recommend further studies to verify their findings. In favour of small size chest tubes such as pigtail catheters is the reduction of pain and discomfort related to the procedure (6).
The aim of this study was to evaluate the influence of chest tube size and position on chest tube duration in patients hospitalized with PSP.
Methods
In accordance with Danish Law the national ethics committee waives review and consent requirements for retrospective follow-up studies, but the Danish data protection agency approved the present study. Data was retrospectively collected and reviewed for all consecutive patients admitted and diagnosed with PSP at the Odense University Hospital from January 2009 to December 2013. Patients with empyema, hydrothorax, previous lung surgery or any suspicion of catamenial pneumothorax were excluded. Patients with a secondary-, iatrogenic- or traumatic pneumothorax were also excluded. All patients with known underlying pulmonary diseases were categorized as secondary pneumothorax.
The primary treatment strategy for spontaneous pneumothorax at our hospital is chest tube drainage but the decision to use different types and sizes is left at the discretion of the attending surgeon and can vary from a silicone chest tube (size 21–24 Fr) to a pigtail catheter (size 12–16 Fr). Insertion of pigtail or chest tube is always inserted in the “safe triangle” (1), the triangle bordered by the anterior border of the latissimus dorsi, the lateral border of the pectoralis major muscle, a line superior to the horizontal level of the nipple, and an apex below the axilla. Therefore, the chest tubes most often were placed mid-axillary in IC5.
Chest tube management did not follow a specific protocol but followed general chest tube management by dedicated general thoracic surgery staff and consisted primarily of early and maximum ambulation. When suction was considered necessary this was used at all times except when the patient was ambulating in the ward. Chest tubes were only removed when there was absolutely no detectable air leakage during forceful coughing whereas the amount of clear chest tube fluid was never a reason for continuing drainage. Patients were always discharged with a fully expanded lung except when a small pneumothorax less than 10 mm after chest tube removal was diminishing on a subsequent chest X-ray the following day and such patients were always seen in the outpatient clinic after one week to ensure full expansion of the lung.
All patient charts and chest X-rays taken before and after placement of the chest tube or pigtail catheter were retrieved and re-analysed. Patients were excluded from analysis if the chest X-rays were not available. The following variables were recorded from the patient’s chart: gender, age (categorized as <30 years, 30–60 years and >60 years), length of hospitalization, history of smoking, history of previous pneumothorax, side and severity of the pneumothorax, treatment, type and size of chest tube (pigtail catheter or surgical chest tube), duration of chest tube drainage, if suction was applied to the chest tube, and whether the patient experienced recurrence within the first 24 hours after chest tube removal.
The chest X-ray used to diagnose the pneumothorax was used to measure the size of the pneumothorax, which was categorized into four groups: total (total collapsed lung), subtotal (apical, lateral and basal slip), apical (apical slip and/or lateral slip) and basal (basal slip). The location of the tube tip was categorized as: apical, middle, and basal depending if the tip was located in the top third, middle third or lower third of the pleural cavity as measured on the chest X-ray immediately following chest tube placement. All chest tube drainage was performed in local anaesthesia and chest tubes were connected to a simple water seal. If the lung was not expanded on subsequent chest X-ray suction could be applied to the water seal at the surgeon’s discretion. The chest tube was left in place until there was no detectable air leak in the water seal after which it was removed during positive airway pressure by Vasalva maneuver. A skin suture left in place during insertion of the chest tube was used to close the drainage site. Treatment was considered complicated if the patient experienced recurrence of the pneumothorax within 24 hours after removal of the chest drainage that needed re-insertion of a chest tube, if the attending surgeon decided to replace the chest tube/pigtail catheter due to lack of expansion of the lung or if the pneumothorax required surgical treatment because of sustained air leakage longer than 5 days.
For statistical analyses, we used ANOVA to compare baseline characteristics. A Cox proportional hazards regression model was used to estimate hazard ratios and to calculate P values as well as 95% CI for predictors of treatment duration. All 134 patients were included in the COX analyses where the complicated were censored.
Patients who were treated with a surgical chest tube was further analysed to examine any differences between size of the chest tubes and chest tube duration. Multivariate logistic regression analysis was used to estimate predictors of complicated in-hospital stay. Furthermore, ordinal logistic regressions analysis was used to investigate differences between the three groups of tube sizes. We used IBM SPSS version 22 for MAC (New York, USA) for all statistical calculations and P values <0.05 were considered significant.
Results
During a 5-year period (January 1st 2009 to December 31th 2013) 297 consecutive patients were diagnosed and treated for pneumothorax at Odense University Hospital. We excluded 163 patients from analysis because of secondary pneumothorax (n=41), iatrogenic pneumothorax (n=21), traumatic pneumothorax (n=32), missing chest X-ray (n=22), empyema (n=10), and hydro- or haemopneumothorax (n=37).
The remaining 134 patients had a median age of 32 years (range, 16–92 years) and a male/female ratio of 2.5. Baseline characteristics between patients who were treated with a pigtail catheter or a chest tube showed that type of chest tube and side of pneumothorax were significantly different as larger surgical chest tubes were used more frequently on the left side and pigtail catheters used more frequently on the right side (P=0.03). All other baseline variables did not differ significantly between the groups, shown in Table 1. The median duration of chest tube drainage was 27 hours for pigtail catheters (range, 10–259 hours), 40 hours for 21 Fr chest tubes (range, 5–136 hours) and 42 hours for 24 Fr chest tubed (range, 11–315 hours). After drainage the postoperative course was uncomplicated in 97 patients (72%). In the remaining 37 patients (14 treated with pigtail catheter and 23 treated with surgical chest tube) 28 patients underwent VATS (11 pigtail; 17 surgical chest tube). Eight patients needed a new chest drainage due to recurrence of the pneumothorax within 24 hours after removal of the chest drainage (3 pigtail, 5 chest tube) and 9 patients required reposition of the chest tube (3 pigtail, 6 chest tube). Fourteen patients were treated with suction coupled to the drain. Twelve of these were complicated cases and only 2 of them uncomplicated.
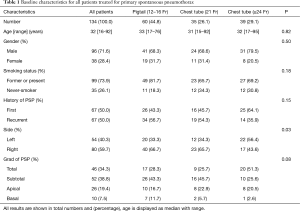
Full table
A Cox regression analysis revealed that female gender, age <30 years, severity of the pneumothorax, use of a surgical chest tube and a history of previous pneumothorax were all significant predictors of prolonged chest tube duration as demonstrated in Table 2.
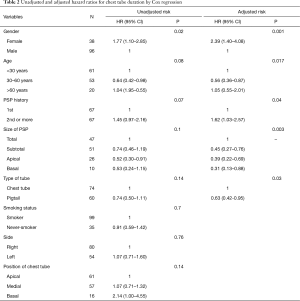
Full table
Due to the fact that the surgical chest tube was revealed as a predictor of prolonged chest tube duration, we made a similar cox regression analysis only for the patients treated with surgical chest tube (n=79). This revealed that chest tube duration was significantly longer for large 24 Fr surgical chest tubes compared with smaller surgical chest tube 21 Fr (HR =1.89; 95% CI, 1.01–3.45; P=0.045). An analysis comparing pigtail and surgical chest tube size 21 Fr was performed. This showed no significant difference in chest tube duration (P=0.28). However, female gender (P=0.02), the grade of pneumothorax (P<0.01) and a history of pneumothorax (P=0.02) where still predictors of prolonged chest tube duration as shown in the Cox regression analysis for all patients. Multiple logistic regression analysis demonstrated that female gender was the only significant predictor of a complicated in-hospital stay (RR =3.54; P<0.01) and that this was not influenced by type or location of the chest tube.
When we compared the three groups of chest tube size with ordinal regressions analysis the side of the pneumothorax was the only predictor for choice of treatment: Pigtail catheters were used significantly more frequently on the right side (OR =1.27; P=0.03).
Discussion
The most interesting finding in the present study was that the location of the chest tube in the pleural space did not significantly influence chest tube duration. This result contrast with the general assumption that chest tubes should be directed to the apical region of the pleural cavity for optimal treatment of pneumothorax as listed in the British Thoracic Society guidelines (1). Our findings also contrast with a previous study by Benton et al. (3), where they found fewer complications when the tip of the tube was placed in the apical region of the pleura, while 29% of the chest tubes not located in the apex failed to re-expand the lung. We have no clear explanation for this discrepancy but in theory one would expect that air move freely in the pleural cavity, which is one continuous space, by simple differences in pressure gradient towards the lowest pressure point where it is drained by a chest tube.
The present study also demonstrates that chest tube duration was significantly longer in patients admitted with PSP when a conventional surgical chest tube was used. Several previous studies (3-5) compared large chest tubes with pigtail catheter or small tubes and found no significant difference in the in-hospital length of stay. It is not unlikely that results from the previous reports were due to their limited number of patients (n=35 to 102) (3-5). Our results demonstrate a significance difference in treatment duration between chest tube size 21 Fr and size 24 Fr surgical chest tubes, but there was no difference in treatment time between chest tube size 21 and pigtail catheters. None of the previous studies distinguished between chest tube sizes, which may have contributed to their negative findings. The primary treatment strategy for spontaneous pneumothorax at our hospital is chest tube drainage but the decision to use different types and sizes is left to the discretion of the attending surgeon and can vary from a silicone chest tube (size 21–24 Fr) or a pigtail catheter (size 12–16 Fr). We have no obvious explanation for these findings but noticed that surgeons used fewer pigtail catheters on a left side pneumothorax than on a right side pneumothorax. Although we think this is just a random finding, it could purely speculative be due to younger surgeons fear of damaging the heart on the left side when the pigtail catheter is inserted with a sharp guide trocar in contrast with conventional surgical placement following digital exploration. In contrast, size of the pneumothorax did not influence which type or size of chest tube was used. Thus, larger sized chest tubes were not used for larger sized pneumothoraxes. Multiple regressions analysis revealed that female gender was the only predictor of a complicated hospital stay. We have no solid explanation for this finding.
The logical consequence of the present study is that one should worry less about exact chest tube placement for treatment of simple spontaneous pneumothorax. In our daily practice we aim the chest tube to the apical-anterior portion of the chest cavity when the patient presents with anything but a basal pneumothorax but if the chest X-ray subsequently reveals that the chest tube tip was not located in the apical-anterior portion of the chest cavity we do not reposition the chest tube. If the patient presents with a basal pneumothorax we now aim the chest tube basally. In any case, our clinical practice has also changed towards smaller chest tubes and pigtail catheters for a simple pneumothorax.
The present study is limited by its retrospective nature and a risk of selection bias regarding the choice of chest tube (pigtail or surgical) as well as the size, which was different among surgeons who may have had a personal preference, but such a selection bias was also present in the previous studies (3-5) and ultimately a randomized trial is needed to distinguish between the two types of chest drainage. It would have been relevant and interesting to include severity of the air leak in our analysis but these data was not captured in the patient’s charts. Furthermore, most patients only had a simple one-chamber system. All chest tubes, however, were removed during morning rounds if there was no visible air leak during coughing regardless of the severity of air leak detected during the treatment course. Finally, because it is recommended that all chest tubes should be placed anteriorly in the chest cavity information about the location of the chest tube tip in the anterior/posterior plane would have been relevant for analysis, but this information was not always available immediately after chest tube placement.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: In accordance with Danish Law the national ethics committee waives review and consent requirements for retrospective follow-up studies, but the Danish data protection agency approved the present study.
References
- Havelock T, Teoh R, Laws D, et al. Pleural procedures and thoracic ultrasound: British Thoracic Society Pleural Disease Guideline 2010. Thorax 2010;65 Suppl 2:ii61-76. [Crossref] [PubMed]
- Baumann MH, Strange C, Heffner JE, et al. Management of spontaneous pneumothorax: an American College of Chest Physicians Delphi consensus statement. Chest 2001;119:590-602. [Crossref] [PubMed]
- Benton IJ, Benfield GF. Comparison of a large and small-calibre tube drain for managing spontaneous pneumothoraces. Respir Med 2009;103:1436-40. [Crossref] [PubMed]
- Liu CM, Hang LW, Chen WK, et al. Pigtail tube drainage in the treatment of spontaneous pneumothorax. Am J Emerg Med 2003;21:241-4. [Crossref] [PubMed]
- Vedam H, Barnes DJ. Comparison of large- and small-bore intercostal catheters in the management of spontaneous pneumothorax. Intern Med J 2003;33:495-9. [Crossref] [PubMed]
- Kulvatunyou N, Vijayasekaran A, Hansen A, et al. Two-year experience of using pigtail catheters to treat traumatic pneumothorax: a changing trend. J Trauma 2011;71:1104-7; discussion 1107. [Crossref] [PubMed]


