Chance missed, but still there! Memoirs at the 10th anniversary of 2003 SARS outbreak
It has been ten years since the outbreak of severe acute respiratory syndrome (SARS) was recognized in Guangdong Province, China, in November 2002. As the new infectious disease first emerging at the beginning of the twenty-first century like AIDS in 1980s, SARS posed a serious threat to global health security, human livelihood, functioning of health systems and stability and growth of economies.
Although the last human chain of SARS transmission in the first outbreak (from November 2002 to July 2003) was successfully disrupted on 5 July 2003 owing to global cooperation, the international spread of SARS coronavirus (SARS-CoV) had resulted in 8,098 SARS cases in 26 countries, with 774 deaths (1).
SARS-CoV appeared unexpectedly without warning in Guangdong, China and disappeared dramatically in the world. But the questions where SARS-CoV came from and have gone and whether the disease will reemerge remain poorly understood and frankly puzzling.
We should remember two lessons from our fight against SARS.
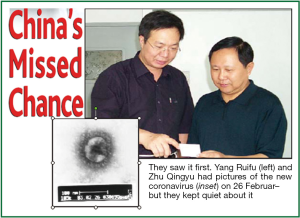
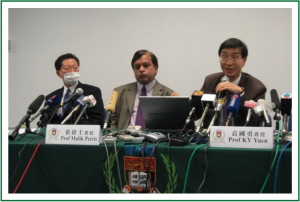
Firstly, scientists in mainland China could have been the earliest to nail the pathogen that caused SARS. Researchers at the Academy of Military Medical Sciences (AMMS) in Beijing discovered the coronavirus on February 26, 2003. Yang Ruifu and Zhu Qingyu from AMMS saw the new coronavirus in an electron micrograph, about 3 weeks before WHO initiated a virtual network of laboratories to investigate the cause of SARS on March 18, 2003 and one month before the Department of Microbiology, Faculty of Medicine, University of Hong Kong (Figure 1) first announced its discovery on a novel coronavirus of SARS on March 27, 2003. “But they kept quiet about it” (Figure 2), therefore, mainland China missed the chance to be the first identifier of the pathogen causing SARS (2-4). Ironically on February 18, 2003, experts in Chinese Centre for Disease Control and Prevention announced that Chlamydia had been identified as the cause of a pneumonia outbreak in Guangdong Province, but this allegation proved wrong (5-7).
Secondly, mainland China could have been the first reporter of the new emerging infectious disease and the first one to name the disease. Unfortunately, the chance was missed again!
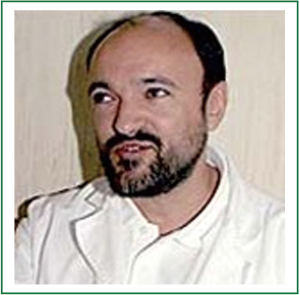
In a document (May, 2003), the World Health Organization (WHO) said that the first cases of SARS were known to have emerged in mid-November of 2002 in Guangdong Province, China. The first official report on an outbreak of atypical pneumonia by the province, revealing the new disease had affected 305 persons and caused 5 deaths (Figure 3), was received by WHO on 11 February, 2003. However, as a matter of fact, SARS was first identified in Vietnam on 28 February, when Dr Carlo Urbani (Figure 4), an epidemiologist from the WHO office in Hanoi, examined a patient with a severe form of pneumonia with no known cause (8).

Why has mainland China missed or lost two chances in the fighting against SARS? As one researcher said and many have noted, this stemmed in part from systemic problems in Chinese community of science: poorly organized coordination or collaboration, stifling political considerations, hesitation to challenge authorities, and isolation from the rest of the world (2).
WHO pointed out that some cases during the earliest phase of the SARS outbreak were not openly reported, thus allowing a severe disease to become silently established in ways that made further international spread almost inevitable. This is the most important lesson for all nations. In a globalized, electronically connected world, attempts to conceal cases of an infectious disease, for fear of social and economic consequences, must be recognized as a short-term stop-gap measure that carries a very high price - loss of credibility in the eyes of the international community, escalating negative impacts on domestic economic, damage to the health and finance of neighboring countries, and a very real risk that outbreaks within the country’s own territory can spiral out of control (8).
In response to the infectious diseases or public health emergency, we should follow the International Health Regulations, “Know the game, play the game”. Mainland China has experienced three outbreaks of SARS. The first and most treacherous one, resulting in 5,327 cases, spanned 9 months from November 2002 to July 2003. The second one only witnessed four sporadic community-acquired cases in Guangzhou between December 2003 and January 2004. Of the four cases, three were related to palm civets sold by a restaurant. In the third outbreak, nine cases arose from a laboratory incident in Beijing between March and April 2004. Thereafter, no new SARS case has been reported in the world (1).
The chance to answer where the notorious virus came from and have gone is still waiting for the scientists on this planet.
Studies have indicated that the SARS-CoV is believed to have crossed the species barrier from animals to humans (9-13). For years, a scientific team led by Xu Dezhong at the Fourth Military Medical University has been looking for the origin of SARS-CoV with biotechnology. They have arrived at a conclusion that SARS-CoV may be non-natural and probably not be entirely of a zoonosis (14). Hopefully they have caught the right answer, but not “Chlamydia” again!
SARS will not be the last emerging infectious disease that threatens human. Control of emerging diseases is never a local issue; it is a mission beyond any geographical or political boundaries and frontiers. Global support, international collaboration and concerted efforts across different specialties and disciplines have contributed to the success in nipping the problem in the bud.
The key to controlling an epidemic is to break up the chain of transmission from the infected to healthy individuals. The successful control measures of SARS epidemics in Guangdong included: (I) Early case identification (an efficient surveillance and reporting system, public information and education to encourage prompt reporting of symptoms); (II) Prompt and effective patient isolation (strict hospital infection control); (III) Timely contact tracing (management of close contacts by home confinement or quarantine); and (IV) Rigorous wild animal administration (covering farms, markets, restaurants, etc).
We all remember when the most terrible outbreak of cholera occurred in London in August 1854, the enterotoxic Vibrio cholerae was totally unknown to all. John Snow’s (Figure 5) conclusion that contaminated water was associated with cholera was entirely based on observational data. In 1883, 29 years later, Robert Koch finally identified Vibrio cholerae as the causative agent. This was a major victory for Snow’s theory and field practice of public health.
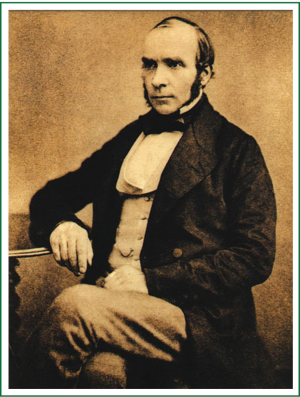
The point is that although it is extremely important for us to maximize our knowledge of the biology and pathogenesis of a disease, it is not always necessary to know every detail of the pathogenic mechanism to be able to prevent a disease (15).
Mainland China had its last indigenous polio case in 1994 and was certificated as a polio-free country by the Regional Commission for the Certification of Poliomyelitis Eradication (RCC) in the WHO Western Pacific Region in 2000. However, between July and October 2011, mainland China experienced an outbreak caused by imported wild poliovirus type 1 (WPV1) from Pakistan, which paralyzed a total of 21 people in four prefectures of Xinjiang. With a tremendous effort to vaccinate the vulnerable population, mainland China successfully interrupted transmission of the virus and terminated the outbreak in record-time (16). Fundamental factors contributing to the successful response to this outbreak have been the extensive partnering between health authorities and other sectors of the Chinese Government, and the highly commendable intercountry and interregional coordination and collaboration with colleagues at the Global Polio Eradication Initiative (GPEI) (17). “I want to express our admiration for the way China had responded to this importation and recommended that it be an example to the rest of the world on how to respond to similar emergencies.” said Prof Anthony Adams, Chairman of the Regional Commission for the Certification of Poliomyelitis Eradication (18,19).
“As we face the new millennium, we must renew our commitment to the prevention and control of infectious diseases, recognizing that the competition between humans and microbes will continue long past our lifetimes and those of our children.” Said Jeffrey P. Koplan, Director of US Center for Disease Control and Prevention. So infectious diseases outbreak, even emerging infectious disease outbreak, is predictable but emergency event, and we need not panic about it. In emergency response, public expect government provide transparent and real time information about the event (outbreak) in their community. Government should adopt the best policy, transparent, in health risk communication.
Health risk communication may be defined as “the art and technique of informing, influencing, and motivating individual, institutional, and public audiences about important health issues”. The scope of health communication includes disease prevention, health promotion, health care policy, and the business of health care as well as enhancement of the quality of life and health of individuals within the community - Healthy People 2010 (20,21).
Reviewing the SARS outbreak in 2003, influenza pandemic (H1N1) in 2009 and poliovirus outbreak (WPV1) in Xinjiang in 2011, we should realize that honesty, openness, transparency and fairness are more valuable than intelligence in health risk communication.
Acknowledgements
Disclosure: The author declares no conflict of interest.
References
- WHO (World Health Organization). 2004. WHO SARS risk assessment and preparedness framework. WHO/CDS/CSR/ARO/2004.2. Available online: http://www.who.int/csr/resources/publications/CDS_CSR_ARO_2004_2.pdf. (accessed 5 Dec 2012).
- Enserink M. SARS in China. China’s missed chance. Science 2003;301:294-6. [PubMed]
- Coronavirus pneumonia: An international research breakthrough. 2003. Available online: http://www.uhs.hku.hk/he/flu/press_releases/pre_0327.pdf. (accessed 6 Dec 2012).
- Enserink M. Infectious diseases. A second suspect in the global mystery outbreak. Science 2003;299:1963. [PubMed]
- Chlamydia has been identified as the pathogen of atypical pneumonia in Guangdong. 2003. Available online: http://news.xinhuanet.com/st/2003-02/18/content_734596.htm. (accessed 18 Dec 2012).
- Experts come to a preliminary confirmation: ChlaInydia-like agent is the perpetrator to atypical pneumonia. 2003. Available online: http://www.chinanews.com/n/2003-04-04/26/291207.html. (accessed 4 Jan 2013).
- Chinese scientists find chlamydia bacteria in SARS cases. 2003. Available online: http://www.chinadaily.com.cn/en/doc/2003-04/04/content_160910.htm. (accessed 24 Dec 2012).
- World Health Organisation - Communicable disease surveillance and response severe acute respiratory syndrome (SARS): Status of the outbreak and lessons for the immediate future (Prepared for the SARS technical briefing, 56th World Health Assembly: 20 May 2003; Geneva) Geneva, Switzerland; 2003. Available online: http://www.who.int/csr/media/sars_wha.pdf .(accessed 5 Dec 2012).
- Guan Y, Zheng BJ, He YQ, et al. Isolation and characterization of viruses related to the SARS coronavirus from animals in southern China. Science 2003;302:276-8. [PubMed]
- Chinese SARS Molecular Epidemiology Consortium. Molecular evolution of the SARS coronavirus during the course of the SARS epidemic in China. Science 2004;303:1666-9. [PubMed]
- Liang G, Chen Q, Xu J, et al. Laboratory diagnosis of four recent sporadic cases of community-acquired SARS, Guangdong Province, China. Emerg Infect Dis 2004;10:1774-81. [PubMed]
- Kan B, Wang M, Jing H, et al. Molecular evolution analysis and geographic investigation of severe acute respiratory syndrome coronavirus-like virus in palm civets at an animal market and on farms. J Virol 2005;79:11892-900. [PubMed]
- Song HD, Tu CC, Zhang GW, et al. Cross-host evolution of severe acute respiratory syndrome coronavirus in palm civet and human. Proc Natl Acad Sci U S A 2005;102:2430-5. [PubMed]
- Tan Y, Sun H, Tang X, et al. Study on the neutral mutation rate of SARS-CoV and rooted phylogenetic tree again and making new ideas about the origin of SARS-CoV. Chin J Dis Control Prev 2012;16:860-2.
- Dr. John Snow. Available online: http://www.ph.ucla.edu/epi/snow.html. (accessed 4 Jan 2013).
- Poliomyelitis. Available online: http://www.wpro.who.int/china/topics/polio/en/. (accessed 20 Jan 2013).
- Western pacific region resolves to play its role in supporting global polio eradication. 2012. Available online: http://www.wpro.who.int/immunization/news/wpr_resolves_role_global_polio_eradication/en/index.html. (accessed 7 Jan 2013).
- Oversight body affirms China’s polio-free status. 2012.
- Available online: http://www.wpro.who.int/china/mediacentre/releases/2012/20121129/en/. (accessed 29 Dec 2012).
- Health communication. Available online: http://www.healthypeople.gov/2010/Document/HTML/Volume1/11HealthCom.htm. (accessed 20 Jan 2013).
- Health communication. Available online: http://en.wikipedia.org/wiki/Health_communication. (accessed 20 Jan 2013).