Pulmonary function tests findings and their diagnostic value in patients with IgG4-related disease
Introduction
IgG4-related disease (IgG4-RD) is an immune-mediated fibroinflammatory condition that can affect the lung and most other organs. The main features of IgG4-RD are high serum IgG4 concentrations and infiltration of IgG4-positive plasma cells into the affected organs. IgG4-RD is a protean condition that mimics many malignant, infectious, and inflammatory disorders. This condition links many disorders previously regarded as isolated, single-organ diseases without any known underlying systemic condition; for example, autoimmune pancreatitis, sclerosing cholangitis, interstitial pneumonia retroperitoneal fibrosis, and many more. These diseases were recognized as a unified entity only 10 years ago (1,2).
IgG4-RD did not appear in medical publications until 2001 (3), and Kamisawa et al. reported the first case of autoimmune pancreatitis with interstitial pneumonia in 2003 (4). In 2005, Zen et al. confirmed that IgG4-RD may also occur in the lungs (5), in 2011, two separate names were adopted for the respiratory tract lesions of IgG4-RD: ‘IgG4-related lung disease’ and ‘IgG4-related pleural disease’ (6). In the latest published diagnostic guide in 2016, they are collectively as ‘IgG4-related respiratory disease (IgG4-RRD)’ (7). IgG4-RRD can involve only the lung or additionally affect other organs. Although many medical conditions have been attributed to IgG4-RD, relatively little is known about IgG4-RRD and it remains a rare condition. The epidemiology of IgG4-RRD is poorly understood, mainly because of challenges in recognizing the disease and in differentiating it from the many disorders it mimics. Only about 50% of patients with IgG4-RRD exhibit respiratory symptoms such as cough, dyspnea on exertion and chest pain, while the remaining 50% display only radiographic abnormalities (8).
Thoracic involvement in IgG4-RD can involve the parenchyma, airways, pleura, and mediastinum and can affect the patient’s lung function. Currently, pulmonary function tests (PFTs) are not routine examinations for IgG4-RD. Since PFTs are a sensitive method for detecting diffuse parenchymal lung disease, we considered that they might be helpful in diagnosing IgG4-RRD. To date, there have been few detailed reports of pulmonary function assessments in patients with IgG4-RD or IgG4-RRD. However, a small number of case reports have demonstrated a restrictive pattern of disease with mildly reduced diffusing capacity in IgG4-RRD patients (8-11). In this study, we evaluated the pulmonary function of IgG4-RD patients and assessed the diagnostic value of PFTs for IgG4-RRD.
Methods
Patients
We studied 17 IgG4-RD patients at the Chinese People’s Liberation Army General Hospital from 2012 to 2016. Diagnosis was based on comprehensive clinical assessments, imaging examinations, laboratory tests, histopathology, ultrasonography, and treatment effects. The clinical diagnostic criteria were in line with the international consensus guidelines (7,12,13). The patients were divided into two groups: IgG4-RRD group and IgG4-related disease extrapulmonary involvement (IgG4-RDEI) group. IgG4-RRD manifested as four major types based on thoracic computed tomography (CT) features (14,15): (I) solid nodular type (solitary nodular lesions that include a mass); (II) round-shaped ground-glass opacity (GGO) type; (III) alveolar interstitial type showing honeycombing, bronchiectasis, and diffuse GGOs; and (IV) bronchovascular type showing thickening of bronchovascular bundles and interlobular septa. The patients in IgG4-RDEI group have normal thoracic CT findings was considered to have no pulmonary involvement.
PFTs
PFTs to determine the degree of functional impairment were performed in the pulmonary function laboratory of the Chinese People’s Liberation Army General Hospital. We used standard procedures and complied with the American Thoracic Society and European Respiratory Society guidelines published in 2005 (16-19). Pulmonary ventilation, lung capacity, and gas exchange were measured with a spirometer (MasterScreen Body; Jaeger, Wurzburg, Germany). Diffusing capacity of the lungs was determined by the single-breath carbon monoxide technique. The results were analyzed with Master Lab Manager V5.31.0 software (Jaeger). Each test was repeated at least three times, and all spirometric values were expressed as a percentage of the predicted values. The main test parameters were: vital capacity (VC), forced vital capacity (FVC), forced expiratory volume in 1 s (FEV1), FEV1/FVC, peak expiratory flow (PEF), maximum expiratory flow at 75%, 50%, and 25% of FVC (MEF75%, MEF50%, MEF25%), maximal mid-expiratory flow (MMEF75/25), residual volume (RV), total lung capacity (TLC), RV/TLC, diffusing capacity of the lung for carbon monoxide (DLCO), alveolar ventilation (VA), and diffusing capacity of the lung for carbon monoxide per liter of alveolar volume (DLCO/VA). In this paper, ‘pulmonary dysfunction’ refers to the patient had at least one abnormal value in PFTs. Restrictive ventilatory dysfunction means TLC<80% predicted values; obstructive ventilatory dysfunction means FEV1/FVC<70%; mixed defect mean the patient had both restrictive ventilatory dysfunction and obstructive ventilatory dysfunction; small airway dysfunction means the patient had at least two test parameters less than 65% predicted values in MEF50, MEF25 or MMEF75/25 (16-19).
Statistical analysis
SPSS 17.0 software was used for statistical analysis. Differences in PFT and laboratory results between the two groups were analyzed using the nonparametric test (test type: Mann-Whitney U). Fisher’s exact test was used to analyze the differences in qualitative data between the two groups. The Spearman correlation test was used to assess correlations between PFT results with serum IgG and IgG subclass concentrations. Quantitative data are expressed as the mean ± standard deviation (SD). Differences were considered significant if the P value was less than 0.05.
Results
Clinical and laboratory features
The 17 patients comprised 12 men (70.6%) and 5 women (29.4%), with ages ranging from 37 to 79 (61.06±12.49) years. There were 9 patients in the IgG4-RRD group (5 men and 4 women) and 8 patients in the IgG4-RDEI group (7 men and 1 woman). The patients’ past respiratory disease history, smoking history, thoracic CT features, duration of IgG4-RRD and involved organs are shown in Table 1. There were no significant differences in age, sex, history of respiratory disease, and smoking history between the two groups (P values were 0.082, 0.277, 0.168 and 0.872 respectively).
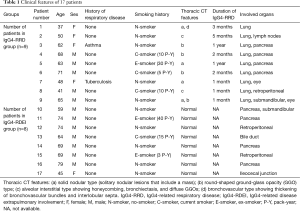
Full table
In IgG4-RRD group, there were 2 lung biopsy-proven cases and 2 postoperative histology-proven cases. The remaining patients were diagnosed by imaging examinations, laboratory tests, ultrasonography and treatment effects. All of patients in IgG4-RDEI group were confirmed by postoperative histopathology. There were 6 patients had respiratory symptoms in IgG4-RRD group, including 5 cases (83.3%) with cough, 4 cases (66.7%) with exertional dyspnea and 2 cases (33.3%) with chest pain. None of the patient in IgG4-RDEI group had respiratory symptoms.
The laboratory features of two groups are shown in Table 2. The elevated serum IgG4 and IgE levels were observed in 88% and 55% of 17 patients, respectively. The erythrocyte sedimentation rate (ESR), total serum IgG and serum IgE in IgG4-RRD group were significantly higher than in IgG4-RDEI group (P=0.02, 0.045 and, 0.007, respectively). There were no significant differences in white blood cells, percentage of eosinophils, C-reactive protein, serum IgG subclasses, complement 3 and complement 4 between the two groups. The Screening for autoantibodies and tumor markers were negative in all patients.
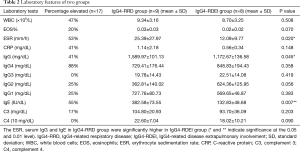
Full table
PFT features
The patients’ PFT results are shown in Table 3. DLCO/VA was significantly lower in the IgG4-RRD group than in the IgG4-RDEI group (P=0.044), but there were no other significant differences between the two groups.
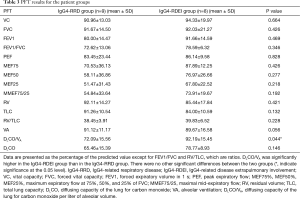
Full table
The incidences of pulmonary dysfunction in two groups are shown in Table 4. Fisher’s exact test was used to analyze the differences in the incidence of pulmonary dysfunction between the two groups. The incidence of DLCO/VA decrease were significantly higher in the IgG4-RRD group than in the IgG4-RDEI group (P=0.029), but there were no other significant differences between the two groups. Both groups of patients showed mainly restrictive ventilatory dysfunction and abnormal diffusing capacity.
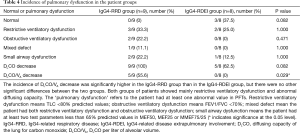
Full table
All 9 patients in the IgG4-RRD group and 5 of 8 patients (62.5%) in the IgG4-RDEI group showed evidence of pulmonary dysfunction. Nine (100%) and 5 (62.5%) patients in the IgG4-RRD and IgG4-RDEI groups, respectively, had decreased DLCO. Five (55.6%) of the IgG4-RRD group had reduced DLCO/VA, but this was normal in the IgG4-RDEI group. The incidence of patients with restrictive and obstructive ventilatory dysfunction was 33.3% and 22.2%, respectively, in the IgG4-RRD group and 25% and 0%, respectively, in the IgG4-RDEI group. It is noteworthy that, despite having normal thoracic CT scans and no respiratory symptoms, 25% of the patients in the IgG4-RDEI group had restrictive ventilatory dysfunction, and 62.5% had decreased DLCO. However, the DLCO/VA was normal in this group.
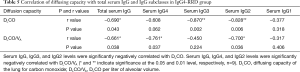
Correlation of diffusing capacity with total serum IgG and IgG subclasses in IgG4-RRD group
The Spearman correlation test was used to examine the relationship between pulmonary diffusing capacity and concentrations of total serum IgG or IgG subclasses (Table 5). Total serum IgG, IgG3, and IgG2 were significantly negatively correlated with DLCO (r=−0.690, −0.870, and −0.828, respectively), whereas IgG, IgG4, and IgG2 were significantly negatively correlated with DLCO/VA (r=−0.661, −0.761, and −0.700, respectively).
Full table
Discussion
IgG4-RD is a protean fibroinflammatory disorder involving single or multiple organs. In recent years, concern about IgG4-RD has become widespread, and an increasing number of studies are investigating the clinical features, diagnosis, and treatment of this disease (20,21). IgG4-RD with respiratory involvement, or IgG4-RRD, is rarely encountered in clinical practice, and a complete picture of the disease has not yet been elucidated. Indeed, many clinical and pathophysiological details about IgG4-RRD have yet to be examined.
IgG4-RD has atypical clinical manifestations and histopathology is the gold standard for diagnosis in most settings. Regardless of which organs are involved, the three central pathological features of IgG4-RD are lymphoplasmacytic infiltration, storiform fibrosis, and obliterative phlebitis (1,2). However, histopathological diagnosis can be complicated by the difficulty in analyzing each organ suspected to be involved. Therefore, the most accurate assessment of IgG4-RD is based on a full clinical history, physical examination, selected laboratory investigations, and appropriate radiological studies (13). The clinical, radiographic, and pathological findings of IgG4-RRD patients, as well as their treatment options, have been described previously (8,10,15,22). However, descriptions of pulmonary function in this patient group have been limited to a small number of cases (8-11). Our study suggests that PTFs could be important tools for the diagnosis of lung involvement in IgG4-RD. Since thoracic involvement in IgG4-RD can involve several sites that affect the patient’s lung function; PFTs may be helpful in assessing the extent of pulmonary disease and in monitoring treatment effects.
In this report, we described the clinical and pulmonary function of 17 IgG4-RD patients; 9 with respiratory involvement and 8 without. All patients in the IgG4-RRD group had pulmonary dysfunction; however, we also found that 5 patients in the IgG4-RDEI group had pulmonary dysfunction, despite having normal thoracic CT scans and no respiratory symptoms and none of them had history of respiratory disease. This suggests that PFTs monitoring of lung involvement may be earlier than imaging examination. Both groups of patients showed nonspecific restrictive ventilatory dysfunction and abnormal diffusing capacity, similar to the findings in patients with other diffuse parenchymal lung disease. Only mild impairment of lung function was observed, and there were no cases of severe restrictive ventilatory defects or severe diffusion dysfunction. In addition, two patients in the IgG4-RRD group had obstructive ventilatory dysfunction, which probably related to lesions involving the airway. What’s more, none of the above two patients had history of asthma or COPD or other obstructive airway diseases, but one patient was a current-smoker who had a 5 pack-year history of smoking. Decreased DLCO was observed in all of the IgG4-RRD group and in 62.5% of the IgG4-RDEI group, whereas DLCO/VA was reduced in 55.6% of the IgG4-RRD patients but none of the IgG4-RDEI patients. The incidence of DLCO/VA decrease were significantly higher in the IgG4-RRD group than in the IgG4-RDEI group (P=0.029), but there were no other significant differences between the two groups. DLCO/VA was significantly higher in the IgG4-RDEI group than in the IgG4-RRD group. The remaining PFT results were not significantly different between the two groups. Therefore, we believe that DLCO/VA plays an important role for detecting lung involvement in IgG4-RD patients. DLCO/VA is the ratio of carbon monoxide diffusing capacity to alveolar volume and represents the diffusing capacity per unit of lung volume. Since this measure excludes the influence of lung volume on the diffusing capacity, DLCO/VA is considered to be more informative than DLCO.
This is the first report of a negative correlation between pulmonary diffusing capacity and total serum IgG and IgG subclasses (IgG4, IgG3 and IgG2). Because the total serum IgG in IgG4-RRD group were significantly higher than in IgG4-RDEI group (P=0.045), we surmised that patients with high serum IgG are more prone to respiratory involvement and thus to effects on the diffusing capacity. The main features of IgG4-RD are high serum IgG4 concentrations and infiltration of IgG4-positive plasma cells into affected organs. Although high serum IgG4 concentrations are insufficiently sensitive or specific for a diagnosis and are unreliable as a single diagnostic marker, the combination of serum IgG4 and IgG concentrations are useful for screening (23-25). In this report, elevated serum IgG4 and IgG levels were observed in 88% and 41% of 17 patients, respectively. Higher serum IgG4 levels could simply come from the increased numbers of organ involvements as reported previously (26), the cell sources of IgG4 are not only the plasma cells in the lung but also those in the other organs (pancreas, lymph nodes, submandibular glands, eye, etc.). But in our study, there was no significant correlation between IgG4 and the number of organ involvement (r=0.220, P=0.430). Moreover, serum IgE levels and eosinophilia were commonly observed (8,20,27). The elevated serum IgE levels and eosinophilia were observed in 55% and 20%, respectively. We found that serum IgE levels were significantly increased in IgG4-RRD compared with IgG4-RDEL (almost 3-fold), the reasons are not clear, which may be associated with prone to respiratory involvement in IgG4-RD patients who were more prone to lung-related allergic diseases. Our future research will focus on the long-term follow-up of pulmonary function in patients with IgG4-RRD and the relationship between pulmonary function and total serum IgG and IgG subclasses after treatment.
IgG4-RRD does not usually lead to serious dyspnea and severe lung function impairment. Our studies and most reports have shown that IgG4-RRD causes only mild restrictive ventilatory defects and mild diffusing dysfunction (9-11). However, there are a small number of reports that IgG4-RRD can result in severe dyspnea (25), including a case of a patient who became hypoxemic and required supplemental domiciliary oxygen. Her PFTs showed moderate airflow limitation (FEV 66% of predicted and FVC 82% of predicted) and severe impairment of gas exchange (DLCO 28% of predicted).
IgG4-RRD is a disease with many faces. The most accurate assessment of IgG4-RD is based on a full clinical history, physical examination, selected laboratory investigations, and appropriate radiology studies. Greater awareness in the medical community of this disease is needed to ensure earlier diagnosis and prevent severe organ damage, disabling tissue fibrosis, and death. Our study suggests that PFTs may be an important tool in diagnosing lung involvement in IgG4-RD and should be considered whether or not the patient has chest radiographic abnormalities, especially if high concentrations of total serum IgG and/or IgG subclasses (IgG4, IgG3 and IgG2) are present. These data will increase our understanding of IgG4-RRD and may have important implications for the diagnosis and management of IgG4-RRD and the design of future studies. Our observations warrant further investigation of pulmonary function in IgG4-RRD.
Conclusions
Our study found that IgG4-RRD patients display nonspecific restrictive ventilatory dysfunction with abnormal diffusing capacity, and a small number of patients showed obstructive ventilatory dysfunction. DLCO/VA plays an important role for detecting lung involvement in IgG4-RD patients. Some IgG4-RD patients with normal thoracic CT scans and no respiratory symptoms also showed mild restrictive ventilatory dysfunction and abnormal diffusing capacity. This is the first report of a negative correlation between pulmonary diffusing capacity and total serum IgG and IgG subclasses (IgG4, IgG3 and IgG2), suggesting that patients with high serum IgG may be more prone to respiratory involvement.
Acknowledgements
We are grateful to Feng-Ying Hao, Xiao-Qing Wang, Jian-Guo Wang and other technicians in the Pulmonary Function Testing Room of Chinese People’s Liberation Army General Hospital for their contribution to this study.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by Ethics Committee of the Chinese People’s Liberation Army General Hospital (No. S2016-03-012).
References
- Kamisawa T, Zen Y, Pillai S, et al. IgG4-related disease. Lancet 2015;385:1460-71. [Crossref] [PubMed]
- Stone JH, Zen Y, Deshpande V. IgG4-related disease. N Engl J Med 2012;366:539-51. [Crossref] [PubMed]
- Hamano H, Kawa S, Horiuchi A, et al. High serum IgG4 concentrations in patients with sclerosing pancreatitis. N Engl J Med 2001;344:732-8. [Crossref] [PubMed]
- Kamisawa T, Funata N, Hayashi Y, et al. A new clinicopathological entity of IgG4-related autoimmune disease. J Gastroenterol 2003;38:982-4. [Crossref] [PubMed]
- Zen Y, Kitagawa S, Minato H, et al. IgG4-positive plasma cells in inflammatory pseudotumor (plasma cell granuloma) of the lung. Hum Pathol 2005;36:710-7. [Crossref] [PubMed]
- Stone JH, Khosroshahi A, Deshpande V, et al. Recommendations for the nomenclature of IgG4-related disease and its individual organ system manifestations. Arthritis Rheum 2012;64:3061-7. [Crossref] [PubMed]
- Matsui S, Yamamoto H, Minamoto S, et al. Proposed diagnostic criteria for IgG4-related respiratory disease. Respir Investig 2016;54:130-2. [Crossref] [PubMed]
- Sun X, Liu H, Feng R, et al. Biopsy-proven IgG4-related lung disease. BMC Pulm Med 2016;16:20. [Crossref] [PubMed]
- Wibmer T, Kropf-Sanchen C, Rüdiger S, et al. Isolated IgG4-related interstitial lung disease: unusual histological and radiological features of a pathologically proven case. Multidiscip Respir Med 2013;8:22. [Crossref] [PubMed]
- Schneider F, Veraldi KL, Levesque MC, et al. IgG4-Related Lung Disease Associated with Usual Interstitial Pneumonia. Open Rheumatol J 2016;10:33-8. [Crossref] [PubMed]
- Baltaxe E, Shulimzon T, Lieberman S, et al. IgG4-Related Lung Disease - Three Untreated Cases with a Benign Outcome. Arch Bronconeumol 2016;52:e1-3. [PubMed]
- Umehara H, Okazaki K, Masaki Y, et al. Comprehensive diagnostic criteria for IgG4-related disease (IgG4-RD), 2011. Mod Rheumatol 2012;22:21-30. [Crossref] [PubMed]
- Khosroshahi A, Wallace ZS, Crowe JL, et al. International Consensus Guidance Statement on the Management and Treatment of IgG4-Related Disease. Arthritis Rheumatol 2015;67:1688-99. [Crossref] [PubMed]
- Inoue D, Zen Y, Abo H, et al. Immunoglobulin G4-related lung disease: CT findings with pathologic correlations. Radiology 2009;251:260-70. [Crossref] [PubMed]
- Fei Y, Shi J, Lin W, et al. Intrathoracic Involvements of Immunoglobulin G4-Related Sclerosing Disease. Medicine (Baltimore) 2015;94:e2150. [Crossref] [PubMed]
- Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J 2005;26:319-38. [Crossref] [PubMed]
- Wanger J, Clausen JL, Coates A, et al. Standardisation of the measurement of lung volumes. Eur Respir J 2005;26:511-22. [Crossref] [PubMed]
- Macintyre N, Crapo RO, Viegi G, et al. Standardisation of the single-breath determination of carbon monoxide uptake in the lung. Eur Respir J 2005;26:720-35. [Crossref] [PubMed]
- Pellegrino R, Viegi G, Brusasco V, et al. Interpretative strategies for lung function tests. Eur Respir J 2005;26:948-68. [Crossref] [PubMed]
- Wallace ZS, Deshpande V, Mattoo H, et al. IgG4-Related Disease: Clinical and Laboratory Features in One Hundred Twenty-Five Patients. Arthritis Rheumatol 2015;67:2466-75. [Crossref] [PubMed]
- Stone JH. IgG4-related disease: nomenclature, clinical features, and treatment. Semin Diagn Pathol 2012;29:177-90. [Crossref] [PubMed]
- Campbell SN, Rubio E, Loschner AL. Clinical review of pulmonary manifestations of IgG4-related disease. Ann Am Thorac Soc 2014;11:1466-75. [Crossref] [PubMed]
- Sah RP, Chari ST. Serologic issues in IgG4-related systemic disease and autoimmune pancreatitis. Curr Opin Rheumatol 2011;23:108-13. [Crossref] [PubMed]
- Tabata T, Kamisawa T, Takuma K, et al. Serum IgG4 concentrations and IgG4-related sclerosing disease. Clin Chim Acta 2009;408:25-8. [Crossref] [PubMed]
- Hui P, Mattman A, Wilcox PG, et al. Immunoglobulin G4-related lung disease: a disease with many different faces. Can Respir J 2013;20:335-8. [Crossref] [PubMed]
- Kamisawa T, Okamoto A, Funata N. Clinicopathological features of autoimmune pancreatitis in relation to elevation of serum IgG4. Pancreas 2005;31:28-31. [Crossref] [PubMed]
- Lin W, Lu S, Chen H, et al. Clinical characteristics of immunoglobulin G4-related disease: a prospective study of 118 Chinese patients. Rheumatology (Oxford) 2015;54:1982-90. [Crossref] [PubMed]


