Procalcitonin as preoperative marker for surgery in advanced parapneumonic empyema
Introduction
Thoracic surgical presentation of patients with advanced parapneumonic pleural empyema is often delayed due to late diagnosis and inconsequent antibiotic therapy of the underlying pneumonia (1). Hence, the optimal moment is missed for a minimal invasive procedure providing a relevant input of infection control (2,3). Length of antibiotic treatment or bacterial spectrum is often unknown. Pleural enhancement andand pleural thickening, fibrin septa and a trapped lung are the typical findings in computer tomography (CT) scan and sonography. Patients with pleural empyema show the clinical signs of infections consisting of fever, chest pain, dyspnea, leukocytosis and elevation of C-reactive protein. Under the mentioned circumstances a surgical procedure is intended to free the trapped lung enabling a normal lung function rather than providing a rapid infection control. Based on these requirements strictly minimal invasive procedures are not sufficient enough and therefore at least partial open procedures such as decortication and/or pleurectomy are needed (4,5). Stable condition of patients and extent of surgical procedure do not necessitate an operative urgency comparable to early empyema and allow for that reason the best possible preparation to major surgery. This consists in consequent antibiotic treatment of the systemic infection and—if necessary—in the drainage of relevant liquid portions. To evaluate the success of systemic treatment, white blood cells (WBC) and C-reactive protein (CRP) are not appropriate enough neither to recognize bacterial infections nor to distinguish between systemic and local infection. In contrast, the blood marker procalcitonin (PCT) has been successfully introduced as a marker for guidance of antibiotic therapy in lower respiratory tract infections (6,7). It correlates with severity and extent of bacterial infections and is only increased in systemic infections like pneumonia. In localized processes like empyema PCT-levels are usually not elevated. Thus, falling preoperative PCT (pPCT)-levels may be useful to evaluate a successful systemic treatment and are therefore a good precondition for major surgery (8). The aim of this retrospective study is to evaluate PCT as a preoperative marker in advanced parapneumonic empyema. We hypothesize a shorter postoperative length of stay and fewer complications when the surgical intervention takes place once PCT levels have dropped to normal ranges compared to early interventions with increased PCT levels.
Methods
Subjects and study design
This is a retrospective observational study at the Cantonal Hospital Aarau, Switzerland. Between June 2010 and April 2015, 38 consecutive patients were operated on for advanced parapneumonic pleural empyema and are included in this analysis. We did not consider patients with other than parapneumonic empyemas (i.e., traumatic, postoperative). This study was conducted in accordance with the amended Declaration of Helsinki. Local ethic committee (EKNZ 2014-401) approved the protocol and informed consent was obtained from all patients.
Definitions
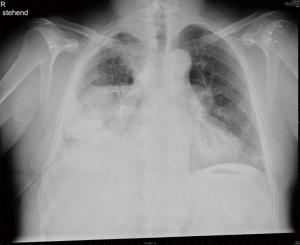
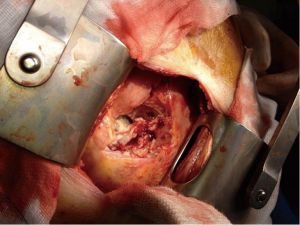
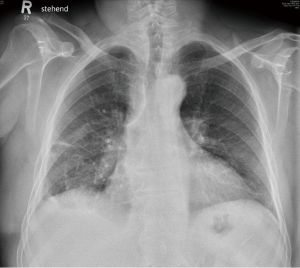
Initial diagnosis of pneumonia was related to clinical signs such as cough, chest pain, infiltrate on chest X-ray and no other sources for infection. The consecutive complicated pleural effusion was therefore diagnosed as parapneumonic. Definition of pleural empyema was based on clinical course after initialization of antibiotic treatment because of pneumonia and typical radiographic features in computer tomography scans (Figures 1,2). Diagnosis of advanced stage was done preoperatively due to the CT scan and was confirmed intra-operatively. According to the American Thoracic Society, advanced or stage III empyemas are defined as empyemas that show a loss of lung compliance due to fibrous peel, completely entrapping the parenchyma (Figure 3). Once the preoperative diagnosis of an advanced empyema was defined, patients were scheduled for surgery as soon as possible in accordance to the OR during the daily working time within the next days. There were no emergency operations. PCT values were obtained the day before surgery.

PCT cut-offs and surgical procedure
We identified 38 patients with available pPCT values who were assigned to two groups according to the PCT cut-off of 0.25 µg/L. This cut-off was chosen according to the ProHOSP study group (9). pPCT blood levels were routinely obtained the day before the scheduled surgery. All operations were performed by the same two thoracic surgeons. The main goal of every operation was complete pulmonary re-expansion. All operations were performed as an open decortication and pleurectomy. The procedure was performed with a lateral muscle-sparing thoracotomy in the sixth intercostal space with preservation of both the latissimus dorsi and the serratus anterior muscles. The operation consisted of complete removal of the fibrous peel trapping the lung and of resection of the parietal peel by an extra-pleural dissection. Two chest tubes were placed and the preoperatively started antibiotics were continued.
We retrospectively analyzed the following clinical variables: age, sex, preoperative CRP, preoperative WBC, pPCT, initial PCT at admission (if available), comorbidities, postoperative 30-day morbidity, postoperative 30-day mortality, postoperative and overall length of stay and CRP the day before hospital discharge, length of stay from admission to operation.
Chest roentgenograms 1 to 3 months postoperatively (Figure 4) were compared with the preoperative roentgenograms (Figure 1) and the radiological improvement was calculated using a 5-point percentage scale according to Casali et al. (5,10). Complete re-expansion (100%) and moderate improvement (75%) were considered as satisfactory results. The radiological estimation was conducted independently by two of the authors (C Caviezel and F Gambazzi) and the mean result of the observations was used for the analysis.
Statistics
The primary endpoint of this analysis was all total length of hospital stay within the index hospitalization and postoperative length of stay. Secondary endpoints included serious adverse events defined as death or surgery-related complications.
Discrete variables are expressed as counts (percentage) and continuous variables as medians and interquartile ranges (IQR). Frequency comparison was done using the chi-square test. The two-group comparison for continuous data was done with the students t-test. We used univariate and multivariate regression analysis to study the association between PCT level and primary and secondary outcomes adjusting the models for important confounding factors such as age, gender and comorbidities. Logarithmic transformation of non-normally distributed data was done prior to modeling (length of stay). Area under the receiver-operating-characteristics curve (AUC) was calculated to assess overall discrimination using STATA 9.2 (Stata Corp, College Station, Texas, USA). All statistical tests were two-tailed and P values less than 0.05 were considered to indicate statistical significance.
Results
Patient population
A total of 38 patients were included in this analysis with a median age of 64 years and 16 patients being males. Patients had a high burden of comorbidities including heart disease in 29%, diabetes in 10.5% and chronic renal failure in 13%. The median overall hospital stay was 17 days. Surgery-related complications occurred in 21% and mortality was 5.25%.
Thirty-four of the 38 patients had a satisfactory radiological improvement after decortication and pleurectomy (89%). In 13 patients (34%) the improvement was moderate and in 21 patients (55%) there was complete re-expansion of the lung.
PCT was measured preoperatively and these patients were divided into two groups based on the pPCT level at the 0.25 µg/L cut-off. Table 1 shows baseline and outcome data of the patients stratified based on their PCT levels <0.25 and ≥0.25 µg/L. The two populations were similar but showed significant differences in regard to chronic renal failure and heart disease. The median preoperative CRP levels were 132 mg/L (IQR 50–176) in the <0.25 µg/L group and 186 mg/L (IQR 144–272) in the ≥0.25 µg/L group (P=0.005). For WBC, the respective median values were 9.4 G/l (IQR 7.7–12.4) and 12.3 G/l (IQR 10.3–20.6) (P=0.015).

Full table
Association of initial PCT level at admission and of pPCT level
PCT level at admission was available in 28 patients. In these patients median initial PCT level was 2.25 µg/L (IQR 1–9.6) and dropped preoperatively to 0.445 µg/L (IQR 0.1–1, P<0.001). Patients with a pPCT level <0.25 µg/L (12/28) had a drop from initially 2.25 to 0.1 µg/L (P=0.002). Patients with a pPCT level ≥0.25 µg/L (16/28) had a drop from initially 2.36 to 0.99 µg/L (P=0.004). Initial PCT levels show no significant difference between the two groups (P=0.695).
Length of stay from admission to operation
Mean length of stay from admission to operation for all patients [38] was 5.8 days (IQR 2–8, range 1–15). Patients with a pPCT level <0.25 µg/L had a mean preoperative stay of 6.2 days (IQR 2–9.5). Patients with pPCT level ≥0.25 µg/L had almost the same preoperative length of stay (median 5.4 days, IQR 2.5–7, P=0.66).
Association of pPCT level and outcomes
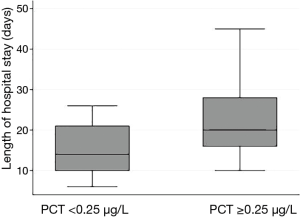
pPCT levels were available in all patients. Patients with a pPCT level ≥0.25 µg/L had a significantly longer total length of hospital stay [mean 22.4 vs. 15.0 days, difference −7.4 days (95% CI: −12.8 to −2.0), P=0.009]. This was also confirmed in linear regression analysis with an adjusted regression coefficient for log-transformed length of stay of −0.34 (95% CI: −0.10 to −0.58, P=0.008) when adjusting for age and gender and regression coefficient of −0.27 (95% CI: −0.02 to −0.52, P=0.037) after adjusting for age, gender and comorbidities. Results were similar for time from surgery to discharge (17.0 vs. 8.7 days, difference −8.2 days, 95% CI: −12.5 to −4.0, P<0.001) with again significant results in adjusted regression analysis [regression coefficient of −0.55 (95% CI: −0.29 to −0.81, P<0.001] after adjusting for age and gender and −0.48 (95%CI: −0.23 to −0.74, P=0.001) after adjusting for age, gender and comorbidities (Figure 5).
Overall, eight patients had postoperative complications, two of them died (mortality 5.25%). All complications occurred in patients with a pPCT level ≥0.25 µg/L (38% vs. 0%, P=0.004). We also compared CRP levels prior to hospital discharge between the two groups but did not find any significant difference (difference −19.8, 95% CI: −60.2 to 20.7, P=0.32).
Discussion
Surgical treatment of advanced parapneumonic empyema is widely accepted [14]. There is current literature focusing on minimal-invasive thoracic surgery and on the identification of clinical predictors to operate successfully with thoracoscopic surgery to avoid thoracotomy and therefore major thoracic surgery (5,11,12). However, advanced parapneumonic empyema still often needs thoracotomy for complete pleural decortication (4,5,13,14). Current literature quotes a mean postoperative length of stay between 8 and 20 days in cases of thoracotomy due to empyema. Postoperative morbidity ranges from 11% to 42% (2-5,15). Therefore, parapneumonic empyema is a disease with a high burden for the patient and the most appropriate therapy has to be selected as early as possible to decrease delay between diagnosis and surgery. Although nowadays early surgery is generally advised one should respect the patient’s recovering from pneumonia prior to the operation. PCT has been recently successfully introduced as a clinical marker for guiding antibiotic therapy in community-acquired pneumonia (8,9). In our retrospective study we analyzed 38 patients with parapneumonic empyema stage who needed thoracotomy for open decortication. The mean length of stay was postoperative 12.8 days and overall 18.7 days. These data are comparable with the current literature (2,3,5,14). Complications occurred in 21%, mortality was 5.25%, whereas the first is also well comparable with the values in literature, the second one is slightly lower.
All operations were performed by the same two thoracic surgeons which ensure some consistency of quality. Fifty-five percent of all patients presented complete radiological re-expansion of the lung and 34% presented moderate improvement. The radiological result is one of the only measurable indicators regarding quality after lung decortication besides complications and length of stay. Only performing decortication in chronic empyema (after a certain interval between empyema detection and surgery) may lung function tests make feasible. Bagheri and colleagues operated after a median of 63.25 days and showed significant improved postoperative pulmonary function (16).
Our measured CRP prior to hospital discharge (mean value 72 mg/L) reflects the usual course postoperatively (13) and did not significantly differ between the two pPCT groups.
The group with a pPCT <0.25 µg/L showed a significant better outcome than the group with pPCT ≥0.25 µg/L. The first group had a shorter overall and postoperative length of stay and no occurrence of either complications or mortality. This finding reinforces our approach of operating on patients presenting with advanced empyema as recently as they have completely recovered from pneumonia. Carboni et al. analyzed postoperative PCT with CRP after decortication of 17 parapneumonic and 5 traumatic empyemas (13). Two groups were compared, one with septic signs and one without septic signs postoperatively. The first group had higher PCT levels and higher CRP levels on postoperative days 1 and 7. Interestingly, the first group had a median PCT level of 0.29 µg/L preoperatively, whereas the second group a mean value of 0.12 µg/L. Further information than measured values until postoperative day 7 (i.e., length of hospital stay) are not available. These findings might confirm our hypothesis of a higher postoperative complication rate when parapneumonic empyema is operated on before PCT values have dropped.
In 28 patients initial PCT levels at time of admission to the hospital were known. There is no significant difference between the two groups but both groups show a significant PCT drop during the preoperative length of stay. Both groups had no significant difference in preoperative length of stay. As the pPCT ≥0.25 µg/L group had significantly more postoperative complications we assume a prolonged preoperative waiting time would have been justified to reach pPCT levels <0.25 µg/L.
Regarding the preoperative CRP and WBC values there is a significant difference between the two groups with the higher values in the pPCT ≥0.25 µg/L group. Like the elevated PCT we interpret these results as another effect of ongoing pneumonia but regard CRP and WBC as less specific markers for bacterial infections (17).
Besides the small number of patients the study’s retrospective manner is a clear limitation. In addition, it has always been the division’s approach to postpone empyema surgery in favor of a medically fitter patient using clinical signs. Since PCT is not routinely provided in our commuting area we do not know the development of PCT from the time of diagnosis of pneumonia until presentation to our division. Based on the numerous studies about pneumonia and PCT we assume that almost all of our patients had initially an even more elevated PCT due to pneumonia and therefore this bias might be of minimal matter. The exact onset of treatment before admission to our hospital was not taken into account in this study and therefore the exact length of antibiotic therapy is not considered, either. When early surgical management of parapneumonic empyema is discussed in literature, there are delays in operation between 5 and 92 days (5) and some authors confirmed a better outcome when the operation was performed within 11 days of admission (11). In our case, the 38 patients had a mean stay of 5.8 days before operation (range, 1–15) which is justified especially if initial PCT would be ≥0.25 µg/L. Another limitation is the restriction to surgically treated patients. Therefor the natural course of PCT in non-operatively managed empyema patients is not known. Neither the course of patients with early stage empyema and possibly minimal-invasively operated patients is taken into account.
Nevertheless, the time from diagnosis of parapneumonic empyema and reaching pPCT levels <0.25 µg/L under antibiotic treatment until final operation has to be shortened. Therefore, the initially declared dogma of early aggressive surgical management should only be advised when the patient’s condition has improved due to decay of pneumonia. One might question the operation itself considering these favorable results regarding control of infection. Although the main goal of decortication is curing the restrictive disease, there is no doubt that decortication in parapneumonic empyema inhibits recurrent empyema by completing control of (chronic) infection (18). High preoperative CRP and WBC levels confirm persistent local inflammation despite decreased SIRS due to cured pulmonary parenchyma invading pneumonia. This interpretation focuses on advanced parapneumonic empyema where open decortication is foreseen. Early stages still profit from thoracoscopic drainage as early as possible (1-3,19).
To our knowledge this is the first report on PCT as a possible marker for the timing of decortication in advanced parapneumonic empyema. It favors the continuation of antibiotic therapy until pPCT decreases to <0.25 µg/L. Therefore, the main goals of therapy in advanced parapneumonic empyema must be the treatment of pneumonia with antibiotics followed by correcting the restrictive disease and preventing chronic infection with decortication and pleurectomy. These results encourage us to conduct a prospective trial regarding timing of decortication.
Acknowledgements
None.
Footnote
Conflicts of Interest: P Schuetz received support from B·R·A·H·M·S AG (now Thermo Fisher Scientific Biomarkers) and bioMérieux to attend meetings and fulfill speaking engagements. The other authors have no conflicts of interest to declare.
Ethical Statement: This study was conducted in accordance with the amended Declaration of Helsinki. Local ethic committee (EKNZ 2014-401) approved the protocol and informed consent was obtained from all patients.
References
- Waller DA, Rengarajan A, Nicholson FH, et al. Delayed referral reduces the success of video-assisted thoracoscopic debridement for post-pneumonic empyema. Respir Med 2001;95:836-40. [Crossref] [PubMed]
- Wozniak CJ, Paull DE, Moezzi JE, et al. Choice of first intervention is related to outcomes in the management of empyema. Ann Thorac Surg 2009;87:1525-30; discussion 1530-1. [Crossref] [PubMed]
- Luh SP, Chou MC, Wang LS, et al. Video-assisted thoracoscopic surgery in the treatment of complicated parapneumonic effusions or empyemas: outcome of 234 patients. Chest 2005;127:1427-32. [PubMed]
- Lardinois D, Gock M, Pezzetta E, et al. Delayed referral and gram-negative organisms increase the conversion thoracotomy rate in patients undergoing video-assisted thoracoscopic surgery for empyema. Ann Thorac Surg 2005;79:1851-6. [Crossref] [PubMed]
- Stefani A, Aramini B, della Casa G, et al. Preoperative predictors of successful surgical treatment in the management of parapneumonic empyema. Ann Thorac Surg 2013;96:1812-9. [Crossref] [PubMed]
- Christ-Crain M, Stolz D, Bingisser R, et al. Procalcitonin guidance of antibiotic therapy in community-acquired pneumonia: a randomized trial. Am J Respir Crit Care Med 2006;174:84-93. [Crossref] [PubMed]
- Müller F, Christ-Crain M, Bregenzer T, et al. Procalcitonin levels predict bacteremia in patients with community-acquired pneumonia: a prospective cohort trial. Chest 2010;138:121-9. [Crossref] [PubMed]
- Schuetz P, Amin DN, Greenwald JL. Role of procalcitonin in managing adult patients with respiratory tract infections. Chest 2012;141:1063-73. [Crossref] [PubMed]
- Schuetz P, Christ-Crain M, Thomann R, et al. Effect of procalcitonin-based guidelines vs standard guidelines on antibiotic use in lower respiratory tract infections: the ProHOSP randomized controlled trial. JAMA 2009;302:1059-66. [Crossref] [PubMed]
- Casali C, Storelli ES, Di Prima E, et al. Long-term functional results after surgical treatment of parapneumonic thoracic empyema. Interact Cardiovasc Thorac Surg 2009;9:74-8. [Crossref] [PubMed]
- Hope WW, Bolton WD, Stephenson JE. The utility and timing of surgical intervention for parapneumonic empyema in the era of video-assisted thoracoscopy. Am Surg 2005;71:512-4. [PubMed]
- Shahin Y, Duffy J, Beggs D, et al. Surgical management of primary empyema of the pleural cavity: outcome of 81 patients. Interact Cardiovasc Thorac Surg 2010;10:565-7. [Crossref] [PubMed]
- Carboni GL, Fahrner R, Gazdhar A, et al. Comparison of procalcitonin and CrP in the postoperative course after lung decortication. Eur J Cardiothorac Surg 2008;33:777-80. [Crossref] [PubMed]
- Okiror L, Coltart C, Bille A, et al. Thoracotomy and decortication: impact of culture-positive empyema on the outcome of surgery. Eur J Cardiothorac Surg 2014;46:901-6. [Crossref] [PubMed]
- Colice GL, Curtis A, Deslauriers J, et al. Medical and surgical treatment of parapneumonic effusions: an evidence-based guideline. Chest 2000;118:1158-71. [Crossref] [PubMed]
- Bagheri R, Haghi SZ, Dalouee MN, et al. Effect of decortication and pleurectomy in chronic empyema patients. Asian Cardiovasc Thorac Ann 2016;24:245-9. [Crossref] [PubMed]
- Müller B, Harbarth S, Stolz D, et al. Diagnostic and prognostic accuracy of clinical and laboratory parameters in community-acquired pneumonia. BMC Infect Dis 2007;7:10. [Crossref] [PubMed]
- Ashbaugh DG. Empyema thoracis. Factors influencing morbidity and mortality. Chest 1991;99:1162-5. [Crossref] [PubMed]
- Lee H, Park S, Shin H, et al. Assessment of the usefulness of video-assisted thoracoscopic surgery in patients with non-tuberculous thoracic empyema. J Thorac Dis 2015;7:394-9. [PubMed]