Somatic cough syndrome or psychogenic cough—what is the difference?
Psychogenic cough
The traditional view of chronic cough was that it is due to medical conditions such as gastroesophageal reflux disease, asthma, rhinosinusitis, lung disease, non-asthmatic eosinophilic bronchitis, and Angiotensin Converting Enzyme inhibitors or environmental exposure such as tobacco smoking. Identifying and treating the underlying cause of the cough was thought to reduce or eliminate cough. The terms psychogenic cough and habit cough have been used to describe cough that has no obvious medical etiology, is refractory to medical management and is considered to have a psychiatric or psychological basis (1). In the early literature, chronic cough was considered to be psychogenic if it persisted despite medical treatment, demonstrated characteristics such as a honking or barking quality, was absent during sleep, or was associated with psychiatric illness. This review will discuss the evidence for the diagnosis and treatment of psychogenic cough. It will explore psychogenic cough as a unique phenotype of cough and examine psychomorbidity in relation to cough. Finally it will outline clinical implications for the diagnosis and management of psychomorbidity in chronic cough including strategies to assist managing the patient with suspected psychogenic cough.
Evidence for the diagnosis and treatment of psychogenic cough
There are limitations in the research regarding psychogenic cough. In 2014, Haydour et al. (2) conducted a systematic review of literature pertaining to psychogenic, habit and tic cough. Eighteen studies including 233 patients were identified. This review found that the methodological quality of the studies was poor. The diagnostic criteria for psychogenic cough were limited to the description of symptoms by the patient. Control groups and validated cough assessment tools were not employed. The studies involved retrospective case series or case studies with limited prospective analysis. There was a heterogeneity of definitions and diagnostic criteria and the possibility of reporting bias (2).
There are limited criteria for the diagnosis of psychogenic cough (2). For example, barking honking cough is thought to be a characteristic feature of psychogenic cough, however, only 8 out of the 18 studies in the systematic review (2) reported this particular cough characteristic. Barking cough has also been reported in medical conditions such as tracheomalacia (3) and bronchiectasis (4). Psychogenic cough is often reported to be absent at night (2) yet cough due to organic disease, such as bronchitis and gastroesophageal reflux disease (5,6), can be absent or reduced at night. Only 4 out of 18 studies reported comorbid psychiatric disorders and only three of these included a formal psychiatric diagnosis. It would appear that the features of psychogenic cough reported in the literature are not unique to psychogenic cough.
The etiology of chronic cough is not always easily identified despite systematic investigation (2) and cough can persist despite systematic assessment and treatment of the underlying cause (7). For example, while treatment for diseases associated with chronic cough such as gastroesophageal reflux disease or rhinosinusitis are effective in treating the underlying condition they may be less effective in treating cough. It is possible that the psychogenic cough label has been applied on the basis of cough being refractory to medical treatment without other supporting evidence.
Clinical practice guidelines
Following Haydour et al.’s systematic review, the 2006 American College of Chest Physicians (ACCP) guideline on psychogenic cough published by the American College of Chest Physicians was updated (8). Ten recommendations were made in the guideline and are listed in Table 1.
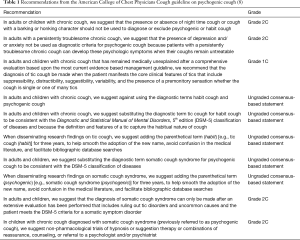
Full table
The guidelines replaced the term psychogenic cough with the term somatic cough syndrome (8), in order to be consistent with terminology used in the Diagnostic Statistical Manual of Mental Disorders, 5th edition (DSM-5). The term psychogenic has been removed from the DSM-5 classification of diseases because functional imaging studies have demonstrated cerebral correlates for disorders previously thought to be of a pure psychogenic nature (9). Psychogenic cough usually refers to a somatisation disorder and is distinct from malingering (10) and conversion disorder (11). Somatization refers to the transfer of psychological distress into a physical symptom (12).
The guideline also replaced the term habit cough with tic cough. A tic is defined as a repetitive movement involving discrete muscle groups. It is a fragment of a normal motor action that is misplaced in context (13). Key clinical features of tics include suppressibility, distractibility, suggestibility and variability (13).
The ACCP guidelines recommend that the presence or absence of nocturnal cough or barking/honking quality should not be used to diagnose or exclude somatic cough syndrome (psychogenic cough). These cough characteristics can be caused by a variety of diseases and lack specificity for a diagnosis (12). The presence of anxiety or depression should not be used as diagnostic criteria for somatic cough syndrome.
The ACCP guidelines recommended that the diagnosis of somatic cough syndrome (psychogenic cough) can only be made after extensive evaluation has been performed, uncommon causes of cough are excluded, and the patient meets the DSM-5 criteria for a somatic symptom disorder. These DSM-5 criteria include one or more somatic symptoms that are distressing or result in significant disruption to daily life. There may be disproportionate and persistent thoughts about the seriousness of the symptoms, high levels of anxiety about symptoms or excessive time and energy devoted to the symptoms (10). In patients diagnosed with somatic cough syndrome, non-pharmacologic trials of hypnosis, suggestion therapy, reassurance, counselling or a referral to a psychologist or a psychiatrist are recommended.
A small number of studies of psychogenic cough from Germany (14), Turkey (15), Italy (16) and Portugal (17) have been published after the systematic review and updated ACCP cough guidelines. These papers consisted of two case studies, a case series of four children with psychogenic cough, and a study of 563 children with all causes of chronic cough (16). In this latter study (16), children suspected of having a psychogenic cough were diagnosed by a psychiatrist based on a honking cough and reduction of cough when sleeping. A newly published Korean cough guideline (18) includes psychogenic cough and describes it as unconsciously persistent cough without an underlying diagnosis. It does not appear that ACCP cough guideline recommendations were incorporated in these publications. It is unclear whether this is due to the timing of submission and publication or that the authors held a different professional perspective regarding the condition.
Psychogenic cough/somatic cough syndrome as a unique phenotype
The concept of somatic cough syndrome as a unique entity may be incongruent with later developing concepts in cough such as idiopathic cough (19,20), unexplained cough (7), cough hypersensitivity syndrome (21,22) and laryngeal hypersensitivity (23,24). These concepts are also used to explain cough without obvious etiology, or that persists despite medical treatment. It is possible that, before these later concepts in chronic cough were developed, some patients with unexplained chronic cough or cough hypersensitivity syndrome would have been labelled as having psychogenic cough. The distinction between somatic cough syndrome (psychogenic cough) and other phenotypes of chronic cough is not entirely clear. For example, underling psychological issues may be contributing factors in the pathogenesis of chronic cough in some individuals, and yet unexplained cough can exist without psychomorbidity.
Psychomorbidity in chronic cough
Psychomorbidity can be increased in patients with chronic cough. Several studies have conducted prospective examination of psychomorbidity in chronic cough (24-27). McGarvey (25) examined levels of psychiatric morbidity in 57 patients referred for specialist evaluation of cough. Patients completed the Hospital Anxiety and Depression Scale (HADS) (28), the State Trait Anxiety Index and the Crown Crisp Experiential Index. Forty two patients had successfully treated cough and 15 had idiopathic chronic cough. Anxiety scores were in the abnormal range (>8) in 33%, while depression scores were in the abnormal range in 16 percent. Mean anxiety and depression scores were in the normal range. These results were similar to those found in other chronic respiratory diseases such as chronic airflow obstruction but less severe than in those with asthma. These results were similar to another study (26) that demonstrated mean anxiety and depression scores (HADS) in patients with chronic cough were in the normal range, however anxiety scores were outside the normal range in 33% of these patients. Trait anxiety, i.e., underlying tendency to anxiety, was moderate in 44% of patients and high in 4% (25). State anxiety, i.e., how anxious the individual is now, was moderate in 28% of patients (25). The Crown Crisp Experiential Index scores were elevated compared with published norms but lower than for psychiatric outpatient populations (25). French (27) reported anxiety scores in the mild range on the Depression, Anxiety and Stress Scale however depression and stress scores were in the normal range. These studies demonstrate that there is increased psychomorbidity in some but not all individuals with chronic cough.
A cross-sectional observational study of patients with a range of laryngeal hypersensitivity disorders including chronic cough, paradoxical vocal fold movement, globus pharyngeus and muscle tension dysphonia (24) examined symptoms, quantitative sensory testing, anxiety and depression. There was no significant difference in severity of symptoms or quantitative sensory testing results between the patient groups, however results were significantly worse than in healthy controls. Mean anxiety and depression scores (Table 2) were in the normal range for most patient groups, with the exception of anxiety scores in the globus pharyngeus group. There was no significant difference in mean scores for anxiety and depression between the patient groups and however mean scores were significantly higher than healthy controls (Table 2). There has been no systematic assessment of laryngeal hypersensitivity in previous studies of patients with psychogenic cough.
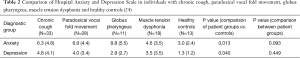
Full table
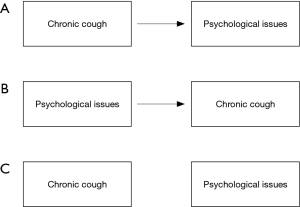
There is a complex relationship between psychomorbidity and chronic cough. The term psychogenic cough implies that psychological issues are an etiological factor in the development of chronic cough. Alternatively, psychomorbidity may be a result of chronic cough in some individuals. The management of chronic cough in primary care is variable and patients may undergo extended and unsuccessful investigations and treatment trials in attempt to diagnose and manage the symptoms (29). The protracted time taken to reach a firm diagnosis for chronic cough can lead to psychological distress in some patients. Furthermore, the numerous physical, social and emotional side effects to chronic cough such as avoidance of daily activities, difficulty with interpersonal relationships, stress urinary incontinence and avoidance of talking, could impact on psychological health (30-32).
Psychological symptoms can improve following successful treatment of chronic cough. For example, Dicpinigaitis (33) reported positive scores on the Centre for Epidemiological Studies Depression Scale (CES-D) in 53% of patients undergoing initial specialist evaluation for chronic cough. The mean CES-D score fell from 18.3±13.2 to 7.4±10.4 following 3 months of medical treatment for the cough. No antidepressant medication was used in any of the patients. This study shows that depressive symptomatology is common in patients with chronic cough but that it improvements following successful medical treatment. Similarly, French (27) administered the Depression, Anxiety and Distress scales to patients at baseline, three and six months following guideline based treatment of chronic cough. Significant improvements in depression and stress scores occurred at three and six months. Anxiety symptoms also improved between baseline and three months. The improvement in depression scores following successful treatment of chronic cough suggests that depression, if present, may often be a side effect rather than a cause of cough.
While psychological symptoms may be the result of chronic cough, cough and respiratory symptoms are more common in individuals with psychological morbidity (34,35). In a population cohort study (34) chronic cough was more common in those with psychomorbidity identified using the General Health Questionnaire-28. The most frequently reported domains were anxiety, insomnia, somatic symptoms, social dysfunction and severe depression. A study of 600 individuals (35) compared responses on the American Thoracic Society respiratory symptom questionnaire (ATS-Q) to the Ilfeld psychiatric Symptom Index (PSI) scores. There was a positive association between respiratory symptoms, including cough, phlegm, wheeze and dyspnoea, and PSI subscales of anxiety, anger, depression and cognitive disturbance. Psychological issues can exacerbate cough in patients with asthma, whereby cough frequency increases in situations that patients have learned to associate with asthma rather than in ones unrelated to asthma (36). These findings suggest that the presence of psychomorbidity does not exclude organic disease and that psychological issues can exacerbate disease severity.
It is possible that the relationship between psychological issues and chronic cough is different between individuals. A model proposing the complex relationship between psychological issues and chronic cough is presented in Figure 1. This figure suggests that co-existing psychological issues in chronic cough may a causal factor in the pathogenesis of cough, a side effect of chronic cough, or be unrelated.
Clinical implications: assessment and diagnosis
Several clinical issues need to be considered in the assessment diagnosis and management of chronic cough associated with psychomorbidity. According to the ACCP cough guidelines, somatic cough syndrome (psychogenic cough) should only be diagnosed if the patient meets the DSM-5 criteria. The diagnosis should not be made or excluded on the basis of nocturnal cough or a cough with barking/honking quality (12). This raises the question of whether it is helpful to diagnose somatic cough syndrome as a distinct phenotype of cough or whether it is sufficient to recognize that patients with chronic cough, such as unexplained chronic cough or cough variant asthma, may have increased psychomorbidity. The term somatic cough syndrome has been recommended to replace psychogenic cough. It is unlikely that these two terms refer to different conditions although perhaps the term somatic cough syndrome places more emphasis on somatic symptoms and incongruity between the distress experienced by the patient and disease severity.
It may be difficult to conceptualise how somatic cough syndrome (psychogenic cough) relates to other types of chronic cough. The level of evidence could make it tempting to dismiss the concept of somatic cough syndrome in favour of more recently developed paradigms such as unexplained cough and cough hypersensitivity syndrome. While diagnosing a patient as having somatic cough syndrome may be the subject of debate, it is helpful to recognize that psychological issues can impact on the perception of disease severity, the development and maintenance of cough symptoms, and upon self-management of symptoms in some individuals.
Patients presenting with chronic cough who have a history of mental health disorders pose a diagnostic dilemma. It is often unclear whether the psychological issues have contributed to the development of or maintenance of the cough symptoms or whether they are a separate coexisting problem. The nature of causality in this relationship needs to be confirmed and the co-existence of psychological issues should not be over-interpreted as being causal. The distinction may be helpful to identify contributing causes of the cough and facilitate referral to relevant mental health professionals.
Clinical implications: management
There is only low quality evidence to support any particular treatment approach for somatic cough syndrome (psychogenic cough). Trials of non-pharmacological therapy such as hypnosis, suggestion therapy, reassurance and counselling may be beneficial after adequate medical assessment (8). The effects of treatment should be measured using recognized outcome measures for cough (37). Referral to a psychologist or a psychiatrist is also recommended.
Some patients may resent being labelled as having a psychological disorder, and therefore sensitive and tactful discussion of psychological issues may be needed. Routine screening of anxiety and depression in patients with chronic cough, similar to screening for other comorbidities such as reflux, may normalize consideration of psychological issues in this population, and help to identify patients at risk.
It may be helpful to consider somatic cough syndrome (psychogenic cough) in a similar manner to the way in which other diseases associated with cough have conceptualised. Song (38) proposed that commonly associated conditions such as rhinosinusitis, esophinophilic bronchitis, asthma and gastroesophageal reflux disease may not be fundamental to the etiology of cough but may serve as triggers to the cough. Similarly, co-existing psychological issues could be viewed as triggers or exacerbating factors for cough in susceptible individuals; however further data would be required to test this hypothesis.
There are several strategies that may be helpful when managing a patient with suspected somatic cough syndrome (psychogenic cough) or with cough suspected of being associated with psychological issues. The process of assessment and clinical problem solving, particularly those used in non-pharmacological approaches, can be therapeutic as they facilitate the patient’s understanding of the contributing factors to their symptoms and their responses to precipitating stimuli. Once serious and commonly-occurring diseases associated with chronic cough have been excluded, it may be more appropriate to focus on symptom control rather than the cause of the cough. Approaches utilizing symptom control are commonly employed in behavioural treatments where patients are taught to identify precipitating sensations to the cough and implement a cough suppression strategy to inhibit the cough. It may be necessary to reassure the patient that there is no serious disease and that the cause of the cough is unable to be identified in many patients. Approaches that focus on symptomatic treatment may be successful in reducing coexisting psychological symptoms.
The therapeutic program should be designed to enable active participation from the patient. Behavioural management of chronic cough involves reassurance that there is no benefit to coughing and that the cough is safe to suppress despite a precipitating sensation. Many patients with chronic cough view their cough as a reflex over which they have no voluntary control (27,30). However, functional magnetic resonance imaging studies demonstrate the role of the supramedullary pathways including the cerebral cortex during cough, and changes in brain behaviour during active cough suppression (39), suggesting a voluntary component to cough. The therapy process aims to teach patients to exert voluntary control over their cough behaviour.
Future research
There is little evidence to guide the definition and diagnosis of somatic cough syndrome (psychogenic cough), and many questions about the condition remain unanswered. Further research is needed to distinguish between somatic cough syndrome and other types of chronic cough such as unexplained cough or cough hypersensitivity syndrome. The clinical and psychiatric profile of patients who are likely to have somatic cough syndrome has not been determined or differentiated from other forms of chronic cough. Prospective studies using standard diagnostic criteria for both excluding coexisting disease and establishing the somatic cough syndrome diagnosis is needed. It is unclear whether certain personality and psychiatric conditions magnify symptom severity and reduce ability to self-manage chronic cough regardless of whether it is classified as somatic cough syndrome.
Conclusions
Psychomorbidity is present in patients with chronic cough with a variety of etiologies, and tends to decrease following successful treatment. Psychogenic cough may have been used in the past as a way to explain refractory cough. Now, with more research, we might wonder whether there are better ways to describe and deal with refractory cough such as cough hypersensitivity syndrome. It might be more effective to consider psychological issues as a trigger or exacerbating factor in cough until further research is conducted to accurately identify the phenotype of somatic cough syndrome.
Acknowledgements
The author recognizes the work of the American College of Chest Physicians Guideline panel in the development of the guidelines that have underpinned this paper. The assistance of Catherine Banney for manuscript feedback and Mary Aldrich in the table and figure formatting is also appreciated.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Irwin R, Glomb W, Chang A. Habit cough, cough tic, and psychogenic cough in adult and paediatric populations: American College of Chest Physicians Evidence based Clinical Practice Guidelines. Chest 2006;129:174-9. [Crossref] [PubMed]
- Haydour Q, Alahdab F, Farah M, et al. Management and diagnosis of psychogenic cough, habit cough, and tic cough: a systematic review. Chest 2014;146:355-72. [Crossref] [PubMed]
- Chang AB, Gaffney JT, Eastburn MM, et al. Cough quality in children: a comparison of subjective vs. bronchoscopic findings. Respir Res 2005;6:3. [Crossref] [PubMed]
- Mello C, Irwin R, Curley F. Predictive values of the character, timing, and complications of chronic cough in diagnosing its cause. Arch Intern Med 1996;156:997-1003. [Crossref] [PubMed]
- Power JT, Stewart IC, Connaughton JJ, et al. Nocturnal cough in patients with chronic bronchitis and emphysema. Am Rev Respir Dis 1984;130:999-1001. [PubMed]
- Irwin RS, Zawacki JK, Curley FJ, et al. Chronic cough as the sole presenting manifestation of gastroesophageal reflux. Am Rev Respir Dis 1989;140:1294-300. [Crossref] [PubMed]
- Gibson PG, Vertigan AE. Management of chronic refractory cough. BMJ 2015;351:h5590. [Crossref] [PubMed]
- Vertigan AE, Murad MH, Pringsheim T, et al. Somatic Cough Syndrome (Previously Referred to as Psychogenic Cough) and Tic Cough (Previously Referred to as Habit Cough) in Adults and Children: CHEST Guideline and Expert Panel Report. Chest 2015;148:24-31. [Crossref] [PubMed]
- Beckmann CF, Jenkinson M, Smith S. General multi-level linear modelling for group analysis in fMRI. NeuroImage 2003;20:1052-63. [Crossref] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th: DSM-5 ed. Washington, DC: American Psychiatric Association, 2013.
- Feinstein A. Conversion disorder: advances in our understanding. CMAJ 2011;183:915-20. [Crossref] [PubMed]
- Wilkes J. ACCP Provides Updated Recommendations on the Management of Somatic Cough Syndrome and Tic Cough. Am Fam Physician 2016;93:416. [PubMed]
- Leckman JF, Bloch MH, King RA, et al. Phenomenology of tics and natural history of tic disorders. Adv Neurol 2006;99:1-16. [PubMed]
- Bonnet U, Ossowski A, Schubert M, et al. On the Differential Diagnosis of Intractable Psychogenic Chronic Cough: Neuropathic Larynx Irritable - Gabapentin's Antitussive Action. Fortschr Neurol Psychiatr 2015;83:568-77. [Crossref] [PubMed]
- Karakaya I, Sismanlar SG. Tic disorders in the differential diagnosis of chronic cough in children in relation to four cases. Turk Pediatri Ars 2015;50:176-9. [Crossref] [PubMed]
- Gedik AH, Cakir E, Torun E, et al. Evaluation of 563 children with chronic cough accompanied by a new clinical algorithm. Ital J Pediatr 2015;41:73. [Crossref] [PubMed]
- Oliveira R, Martins V, Moreira C. Psychogenic Cough: A Rare Cause of Chronic Cough Arch Bronconeumol 2015;51:604-5. [PubMed]
- Rhee CK, Jung JY, Lee SW, et al. The Korean Cough Guideline: Recommendation and Summary Statement. Tuberc Respir Dis (Seoul) 2016;79:14-21. [Crossref] [PubMed]
- Haque RA, Usmani O, Barnes P. Chronic idiopathic cough: A discrete clinical entity? Chest 2005;127:1710-3. [Crossref] [PubMed]
- McGarvey LP. Idiopathic chronic cough: a real disease or a failure of diagnosis? Cough 2005;1:9. [Crossref] [PubMed]
- Morice AS. The cough hypersensitivity syndrome: A novel paradigm for understanding cough. Lung 2010;188:S87-S90. [Crossref] [PubMed]
- Chung KF. Chronic 'cough hypersensitivity syndrome': a more precise label for chronic cough. Pulm Pharmacol Ther 2011;24:267-71. [Crossref] [PubMed]
- Hull JH, Menon A. Laryngeal hypersensitivity in chronic cough. Pulm Pharmacol Ther 2015;35:111-6. [Crossref] [PubMed]
- Vertigan AE, Bone SL, Gibson PG. Laryngeal sensory dysfunction in laryngeal hypersensitivity syndrome. Respirology 2013;18:948-56. [Crossref] [PubMed]
- McGarvey LP, Carton C, Gamble LA, et al. Prevalence of psychomorbidity among patients with chronic cough. Cough 2006;2:4. [Crossref] [PubMed]
- Vertigan AE, Theodoros DG, Gibson PG, et al. Voice and upper airway symptoms in people with chronic cough and paradoxical vocal fold movement. J Voice 2007;21:361-83. [Crossref] [PubMed]
- French CL. Examining change in symptoms of depression, anxiety, and stress in adults after treatment of chronic cough: a dissertation. University of Massachusetts, 2014.
- Zigmond AS, Snaith R. The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica 1983;67:361-70. [Crossref] [PubMed]
- Ringsberg KC, Segesten K, Akerlind I. Walking around in circles--the life situation of patients with asthma-like symptoms but negative asthma tests. Scand J Caring Sci 1997;11:103-12. [Crossref] [PubMed]
- French CL, Irwin RS, Curley FJ, et al. Impact of chronic cough on quality of life. Arch Intern Med 1998;158:1657-61. [Crossref] [PubMed]
- Birring SS, Prudon B, Carr A, et al. Development of a symptom specific health status measure for patients with chronic cough: Leicester Cough Questionnaire. Thorax 2003;58:339-43. [Crossref] [PubMed]
- French CT, Irwin RS, Fletcher KE, et al. Evaluation of a cough-specific quality-of-life questionnaire. Chest 2002;121:1123-31. [Crossref] [PubMed]
- Dicpinigaitis PV, Tso R, Banauch G. Prevalence of depressive symptoms among patients with chronic cough. Chest 2006;130:1839-43. [Crossref] [PubMed]
- Adams RJ, Appleton SL, Wilson DH, et al. Associations of physical and mental health problems with chronic cough in a representative population cohort. Cough 2009;5:10. [Crossref] [PubMed]
- Dales RE, Spitzer WO, Schechter MT, et al. The influence of psychological status on respiratory symptom reporting. Am Rev Respir Dis 1989;139:1459-63. [Crossref] [PubMed]
- Rietveld S, Van Beest I, Everaerd W. Psychological confounds in medical research: the example of excessive cough in asthma. Behav Res Ther 2000;38:791-800. [Crossref] [PubMed]
- Boulet LP, Coeytaux RR, McCrory DC, et al. Tools for assessing outcomes in studies of chronic cough: CHEST guideline and expert panel report. Chest 2015;147:804-14. [Crossref] [PubMed]
- Song WJ, Chang YS, Morice A. Changing the paradigm for cough: does 'cough hypersensitivity' aid our understanding? Asia Pac Allergy 2013;4:3-13. [Crossref] [PubMed]
- Leech J, Mazzone SB, Farrell MJ. Brain activity associated with placebo suppression of the urge-to-cough in humans. Am J Respir Crit Care Med 2013;188:1069-75. [Crossref] [PubMed]


