Re-crossing the distal cell in bifurcation verified by using an enhanced stent visualization system and optical coherence tomography: a report of two cases
Introduction
Percutaneous coronary intervention (PCI) for coronary bifurcation diseases comprises 15–20% of all PCI procedures. The one-stent, provisional T technique has been more strongly recommended than the two-stent technique in most cases (1). Stent mal-apposition and overhanging stent struts in front of the side branch (SB) ostium are not uncommon after bifurcation stenting (2). The coronary guidewire re-crossing position before the final kissing balloon post-dilation is important to reduce the incidence of incomplete stent apposition (3). The 11th consensus document from the European Bifurcation Club recommends the use of the distal cell when re-wiring, which is beneficial to ensure optimal SB re-crossing (4), and the position of the wire re-crossing may be verified by using optical coherence tomography (OCT). The ClearStent Live technique is an enhanced stent visualization system, which can enhance the signal of the stent strut on radiography, and increase the visibility of the stent dramatically during PCI. In the procedure, we should use a balloon as a marker to delimit the enhanced area and the software can increase the visibility of the stent automatically. Here, we present two cases where the ClearStent Live system technique was used to estimate the wire location, which was verified by using OCT.
Case presentation
Case 1
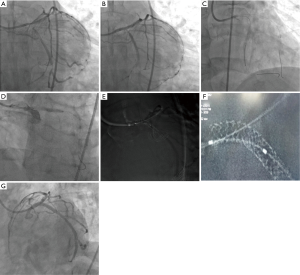
A 53-year-old man with a history of hypertension had worsening exertional angina for 1 week. The patient was pre-treated with aspirin 100 mg and clopidogrel 75 mg per day. The diagnosis was unstable angina pectoris (CCS grade III and Braunwald grade IA). He was referred to our hospital and underwent angiography, which revealed the severe stenosis located at the distal segment and ostium of the left circumflex (LCX) (Figure 1A,B). In addition, a middle segment stenosis was observed at the left main trunk. We have obtained written informed consent from patient before the procedure. After successful wiring and balloon angioplasty, a 2.5 mm × 24 mm stent (Partner, Lepu, China) was deployed in the distal LCX coronary artery and a 3.5 mm × 24 mm stent (PROMUS, Boston Scientific, USA) was deployed from the left main artery to the proximal LCX coronary artery (Figure 1C,D). After re-wiring from the left main artery to the LAD, we used the ClearStent technique, which could enhance the revolution of the strut to estimate the wire location, and found that the wire re-crossed the distal cell (Figure 1E,F). After the successful final kissing balloon and proximal optimal techniques, the final angiography was performed (Figure 1G). We used OCT to verify our hypothesis successfully after re-crossing the distal cell (Figure 2). The patient was discharged 2 days later. No complications occurred either during the hospital stay or during the follow-up (6 months).

Case 2
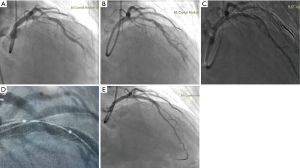
A 55-year-old woman with a history of hypertension and dyslipidaemia was admitted to our hospital because of recurrent chest pain with minimal effort for 1 month. She was pre-treated with aspirin 100 mg and ticagrelor 180 mg per day. The diagnosis was unstable angina pectoris (CCS grade III and Braunwald grade IA). The patient’s current coronary angiogram revealed severe stenosis at the middle segment of LAD, involving the ostium of diagonal artery (Figure 3A). We have obtained written informed consent from patient before the procedure. After successful wiring and balloon angioplasty, a 3.5 mm × 30 mm stent (Resolute, Medtronic, USA) was deployed in the LAD with provisional T technique (Figure 3B). After re-wiring from the LAD to the diagonal artery, we used the ClearStent technique to estimate the wire location (Figure 3C,D). After post dilation with a 4.0-mm balloon, we performed the final angiography (Figure 3E). We used OCT to verify our hypothesis successfully after re-crossing the distal cell (Figure 4). The patient was discharged 2 days later, and his symptom was relieved obviously. At a 1-year follow-up, the patient was asymptomatic and free from events.

Discussion
The European Bifurcation Club strongly recommends the use of the distal cell when re-wiring because crossing the distal cell of the strut, which leads to the SB ostium, has been shown to provide improved outcomes in bifurcations by displacing one to two struts towards the inner curvature of the SB and generating a metal flap to prevent plaque recoil in a segment prone to plaque formation (4). The strut mal-apposition is significantly reduced when wire re-crossing was performed in a distal cell of the SB (4). Currently, no gold standard has been established to judge whether the wire re-crosses the proximal or distal cell. Angiography and intravascular ultrasonography are unreliable at detecting the site of wire re-crossing. The study showed that patients treated with OCT-guided re-crossing had a significantly lower number of mal-apposed stent struts, especially in the quadrants towards the SB ostium [9.5% (range, 7.5–17.4%) vs. 42.3% (range, 31.2–54.7%) in the angiography-guided group, P<0.0001] (4). The high resolution of OCT offers the advantage of a precise assessment of construction in bifurcation. In particular, the emerging three-dimensional (3D) OCT technique offers more detailed detection of the position between the wire and strut, and provides new insights into the process of optimal re-wiring. However, the OCT technique still has some limitations, including the following: (I) the additional contrast required in the OCT procedure is greater than that required for the control group; (II) 3D OCT only can deal with data outside the laboratory; (III) the expense of the OCT technique is high for patients. In the cases reported herein, we used an enhanced stent visualization system, the ClearStent Live system (Siemens Healthcare, Munich, Germany), to estimate the wire location. The ClearStent Live system can enhance the signal of the stent strut on radiography and increase the visibility of the stent dramatically during PCI. The advantages of this technique are as follows: (I) the procedure for enhancement does not require contrast; only injection of 2 mL of contrast medium is needed to confirm the position of the SB. The contrast volume is less than that used for the procedure of the OCT technique; (II) The procedure only takes 1–2 minutes to complete and does not confer additional cost to the patients. Thus, it is superior to the intracoronary imaging techniques in some cases in terms of procedural time and economic benefit. This technique has been reported in the enhancing type and quality of information related to stent placement, expansion, overlapping, and integrity (5). In 2016, Biscaglia et al. (6) used this technique to detect stent fracture in 115 patients. Eventually, they found 136 stent fractures. Although they acknowledged that this technique had relevant limitations, mainly related to the 2D representation of a 3D structure, their results showed that none of these was related to a worse outcome. However, it was the first time that the ClearStent Live system was used in detecting the re-crossing wire. We have used this innovative technique in bifurcation lesions successfully. This technique also has several limitations, which includes the fact that the 2D image cannot expose the space structure clearly and may result in a mismatch in some cases, unlike 3D OCT. In the future, we plan to perform a head-to-head cohort study between OCT and the ClearStent Live system.
Conclusions
The two cases reported herein demonstrate that the ClearStent system could serve as a useful and efficient tool for interventional cardiologists. ClearStent can be used with or to replace intracoronary imaging techniques in selected cases.
Acknowledgements
The authors of this study thank Yang Ruan for her help in obtaining the images.
Funding: This research was supported by a grant from the Development of Capital Health Scientific Fund, China (No. 2014-2-2062).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patients for publication of this manuscript and any accompanying images.
References
- Katritsis DG, Siontis GC, Ioannidis JP. Double versus single stenting for coronary bifurcation lesions: a meta-analysis. Circ Cardiovasc Interv 2009;2:409-15. [Crossref] [PubMed]
- Tyczynski P, Ferrante G, Moreno-Ambroj C, et al. Simple versus complex approaches to treating coronary bifurcation lesions: direct assessment of stent strut apposition by optical coherence tomography. Rev Esp Cardiol 2010;63:904-14. [Crossref] [PubMed]
- Di Mario C, Iakovou I, van der Giessen WJ, et al. Optical coherence tomography for guidance in bifurcation lesion treatment. EuroIntervention 2010;6 Suppl J:J99-J106.
- Alegría-Barrero E, Foin N, Chan PH, et al. Optical coherence tomography for guidance of distal cell recrossing in bifurcation stenting: choosing the right cell matters. EuroIntervention 2012;8:205-13. [Crossref] [PubMed]
- Biscaglia S, Tumscitz C, Tebaldi M, et al. Enhanced stent visualization systems during PCI: A case series and review of literature. J Cardiol Cases 2015;12:1-5. [Crossref]
- Biscaglia S, Tebaldi M, Tumscitz C, et al. Prospective Identification of Stent Fracture by Enhanced Stent Visualization System During Percutaneous Coronary Intervention. Circ J 2016;81:82-9. [Crossref] [PubMed]


