The use of Jackson-Pratt silicone flat drains as prolonged pleural catheters for the management of pleural effusions
Introduction
Pleural effusion is the accumulation of fluid inside the thoracic cage between the visceral and parietal pleuras. It results from disruption of the balance between the secretion and resorbtion of pleural fluid, and can be an indicator of whether the underlying disease originates from the lung versus outside the lung, or acute versus chronic (1-3). A detailed history should be taken in every patient with pleural effusion because the presence of a systemic disease (for example cirrhosis, chronic hepatitis, history of alcohol intake, hepatic hydrothorax or alcoholic pancreatitis, chronic renal failure, or congestive heart failure) or malignancy in past medical history increase the possibility of a malignant pleural effusion.
The most common and practical method to detect pleural effusion is a chest X-ray in posteroanterior and lateral views. Ultrasonography (USG) is helpful in patients with pleural effusions, especially in determining the site of thoracentesis in patients with scarce amount of collection (4). The first procedure required after detection of pleural fluid is pleural drainage, performed by diagnostic and therapeutic thoracentesis (5). Recurrent pleural effusions may be due to malignancy, fluid overload, inflammation, liver failure, pulmonary embolus, pancreatitis, and pleural fibrosis.
Pleural effusion is named recurrent effusion if it reemerges following a prior pleural drainage on the ipsilateral or contralateral side. There are numerous approaches for treatment in recurrent pleural effusions, one of the most common is pleurodesis and often can be applied with a pleural catheter and tube thoracostomy (6). The use of prolonged pleural drainage catheters have been advocated in some studies due to easy application and use. Also, compared with repeated thoracenteses or pleurodeses this method was shown to be more successful in the elimination of symptoms, to have less mortality, lower costs and decreased length of stay (7,8).
The aim of this study was to perform an analysis of 18 patients with recurrent pleural effusions who were managed with prolonged Jackson-Pratt (JP) silicone flat drains due to their easy applicability and lower costs.
Materials and methods
In this study, 18 patients treated between 2011 and 2012 for recurrent pleural effusions due to various etiologies and who were considered to be unsuitable for surgical or other treatments were retrospectively analyzed. All patients were informed other possible treatment methods and consented for prolonged JP silicone flat drain insertion. Patients who had symptomatic or asymptomatic pleural fluids that did not respond to or recurred after treatment and underwent drainage were included into the study. The patients were referred to our unit from the respiratory medicine and medical oncology departments after they were diagnosed to have pleural effusion on radiologic studies [PA-Lateral chest X-ray, computer tomography (CT), chest ultrasound]. A 14F diameter Jackson Pratt silicone flat drain was used as a prolonged pleural catheter (PPC) was inserted easily under local anesthesia.
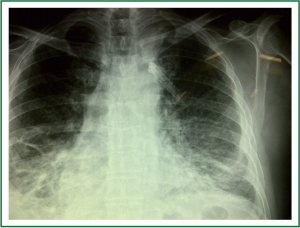
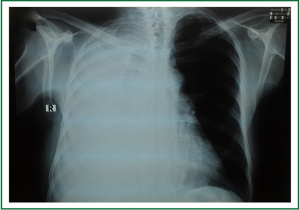
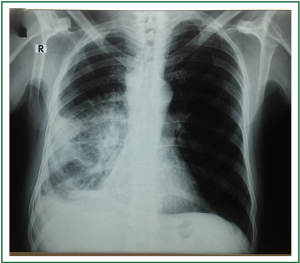
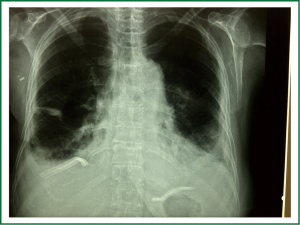
The insertion site for the PPC was determined using USG in order to ensure the correct site for entry and easy access. Twenty of the catheters were placed to the lateral chest wall. In 2 patients the location of the loculated fluid was determined by USG and the catheters were placed with an anterior approach in one and posterior approach in the other (Figures 1,2). After thoracentesis and local anesthesia, the perforated part of the drain was inserted through a 1-1.5 cm incision and subsequently advanced into the thorax, while a clamp occluded the part without the holes. Then a second incision, 0.5 cm long and placed approximately 2.5-3 cm under the first incision, was made. The drain was passed through a subcutaneous tunnel created between the two incisions, taken out through the lower incision and finally was clamped again. The flow of the fluid was assessed by connecting the drain to the negative pressured resorvoir. Once the flow was seen, the first incision was closed with two separate sutures. The drain exit site was also fixed to the skin (Figure 3). Mean operative time for PPC procedure was 10-15 minutes. The location of the catheter inside the thoracic cavity was assessed with postoperative control chest X-ray (Figures 4,5). All patients received sefuroxim 500 mg tablets bid for prophylaxis. Daily drainage was kept under 1,500 mL to avoid lung edema, also drainage was stopped before the onset of abnormal cough that would disturb the patient. Patients with good general conditions were instructed about use of the catheter and were sent either home or to the referring department. The catheters were removed in patients in whom lung expansion was achieved and drainage decreased to less than 50 mL/day.


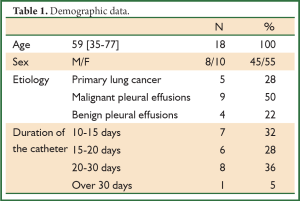
The age, sex, etiologic causes, duration of the catheter and complications were analyzed.
Results
Twenty two PPC (JP silicone flat drains) were inserted in 18 patients for the management of pleural effusions due to various causes. There were 10 females and 8 males, mean age of the patients was 59 [35-77]. The catheters remained for a average period of 19.0 days (10-40 days). The data of the patients are shown on Table 1.
Full Table
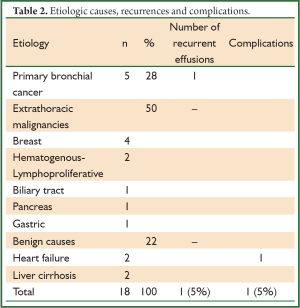
The most common etiology in pleural effusions was extrathoracic malignancies in 9 patients (50%), which was followed by primary bronchial cancer in 5 patients (28%). The etiologic causes are shown on Table 2. Four of the 18 patients underwent bilateral PPC insertion for bilateral pleural effusion (Figures 6,7). One patient with lung cancer developed a recurrent pleural effusion two months after removal of the catheter (5%) (Table 2). A JP drain was inserted again in this patient.
Full Table
In one patient the catheter was removed due to suspicion of empyema during the early period while drainage still continued (5%). This patient had congestive heart failure in the etiology of benign pleural effusion (Table 2). There were no other complications. Two patients died while the catheter was in place and drainage continued. One of these patients had breast cancer and the other biliary tract tumor.
Discussion
There is no standart treatment approach for recurrent pleural effusions. Current treatment alternatives include pleurodesis, pleuroperitoneal shunt, repeated thoracenteses, and insertion of pleural catheters. Pleurodesis requires a chest tube and videothoracoscopic methods, which increase hospital length of stay and costs. In contrast, pleural catheters used especially in recurrent malignant pleural effusions have lower costs and shorter length of stay, and also pleurodesis success rates reaching 81% in malignant pleural effusions (9). Pleuroperitoneal shunts can be used in recurrent pleural effusions, however the patient needs to control the pump and also approximately 1-2 cc of fluid is transferred to the peritoneal space with each use of the pump (10). The British Thoracic Society (BTS) report concluded that PPC was an effective alternative in the control of malignant effusions, minimized the length of stay and enable avoidance of hospital admission (11). Davies et al. found that both talc pleurodesis and indwelling pleural catheters were effective treatments for relieving dyspnea and improving patients’ quality of life but that indwelling catheters were not superior to talc pleurodesis for these outcomes (12). We preferred the PPCs due to their easy availability, lower costs, lower likehood of obstruction due to constant negative pressure, and practical use by the patients.
In previous studies the PPC has been especially preferred in malignant pleural effusions. The most commonly used tunneled pleural catheter is Pleurx catheter (Denver Biomaterials, Golden CO, USA), which is a 15.5 Fr diameter silicone tube measuring 24 inches long, has a perforated distal tip, and harbors a valve at the proximal tip for drainage purpose (7-9,13). It has been determined that the use of this prolonged catheter reduced the length of stay and cost (7-9). Other small catheters may be also used in recurrent pleural effusion, however they have a greater risk of pulling out due to their small diameters. A previous study found that the infection rate in patients with chronic indwelling catheters was 5%. In our series only one patient (5.5%) was diagnosed with an infection, which was similar to the literature.
The procedures for PPC insertion were shorter, therefore the patients were discharged on the same day. All of our patients could be discharged on the same day without any problems. A previous study reported that the rate of ipsilateral recurrences in follow up was 9.9% (8). One of our patients developed ipsilateral pleural fluid collection approximately two months after removal of the catheter (5%).
Prolonged pleural catheters have been suggested as the first line treatment in the management of patients who have developed trapped lung. The lungs in these patients cannot expand, and pleurodesis fails to prevent recurrent pleural effusion. Since decortication will be an invasive and major procedure in these patients, prolonged pleural catheter or pleuroperitoneal shunts are recommended (10,14). None of our patients had trapped lung syndrome.
PPC is a reliable and effective treatment method in recurrent pleural effusions (7,11). The success rate of self sclerosis with PPC is reported to be up to 81%, and may be even higher in gynecologic malignant pleural effusions (9,15). Recurrence was seen in only one patient in our study (5%).
Conclusions
Prolonged Jackson Pratt silicone flat drains for pleural drainage offer shorter length of stay and lower costs, and may be used as an alternative management for malignant, and not benign, pleural effusions in selected patients.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Diaz-Guzman E, Dweik RA. Diagnosis and management of pleural effusions: a practical approach. Compr Ther 2007;33:237-46. [PubMed]
- Sahn SA. Pleural effusions of extravascular origin. Clin Chest Med 2006;27:285-308. [PubMed]
- Light RW. The undiagnosed pleural effusion. Clin Chest Med 2006;27:309-19. [PubMed]
- McLoud TC, Flower CD. Imaging the pleura: sonography, CT, and MR imaging. AJR Am J Roentgenol 1991;156:1145-53. [PubMed]
- Porcel JM, Light RW. Thoracentesis. PIER, American College of Chest Physicians, 2004. Accesed date: October 28, 2004. Available online: http://pier.acponline.org
- Patz EF Jr, McAdams HP, Erasmus JJ, et al. Sclerotherapy for malignant pleural effusions: a prospective randomized trial of bleomycin vs doxycycline with small-bore catheter drainage. Chest 1998;113:1305-11. [PubMed]
- Putnam JB Jr, Light RW, Rodriguez RM, et al. A randomized comparison of indwelling pleural catheter and doxycycline pleurodesis in the management of malignant pleural effusions. Cancer 1999;86:1992-9. [PubMed]
- Tremblay A, Michaud G. Single-center experience with 250 tunnelled pleural catheter insertions for malignant pleural effusion. Chest 2006;129:362-8. [PubMed]
- Putnam JB Jr, Walsh GL, Swisher SG, et al. Outpatient management of malignant pleural effusion by a chronic indwelling pleural catheter. Ann Thorac Surg 2000;69:369-75. [PubMed]
- Ponn RB, Blancaflor J, D’Agostino RS, et al. Pleuroperitoneal shunting for intractable pleural effusions. Ann Thorac Surg 1991;51:605-9. [PubMed]
- Roberts ME, Neville E, Berrisford RG, et al. Management of a malignant pleural effusion: British Thoracic Society Pleural Disease Guideline 2010. Thorax 2010;65 Suppl 2:ii32-40. [PubMed]
- Davies HE, Mishra EK, Kahan BC, et al. Effect of an indwelling pleural catheter vs chest tube and talc pleurodesis for relieving dyspnea in patients with malignant pleural effusion: the TIME2 randomized controlled trial. JAMA 2012;307:2383-9. [PubMed]
- Pollak JS, Burdge CM, Rosenblatt M, et al. Treatment of malignant pleural effusions with tunneled long-term drainage catheters. J Vasc Interv Radiol 2001;12:201-8. [PubMed]
- Pien GW, Gant MJ, Washam CL, et al. Use of an implantable pleural catheter for trapped lung syndrome in patients with malignant pleural effusion. Chest 2001;119:1641-6. [PubMed]
- Warren WH, Kim AW, Liptay MJ. Identification of clinical factors predicting Pleurx catheter removal in patients treated for malignant pleural effusion. Eur J Cardiothorac Surg 2008;33:89-94. [PubMed]