Primary mediastinal myelolipoma: a case report and literature review
Introduction
Myelolipoma was first described in 1905 (1), and named “myelolipoma” in 1929 (2). It is composed of mature adipose and hemopoietic tissue, which is a benign tumor, and it is mainly found in the adrenal gland, while the mediastinal location is extremely unusual (3). Until now only 48 cases of mediastinal myelolipoma including our case have been reported (4-10). With the widespread application of the imaging examination method, its incidence has increased. Some of the patients are asymptomatic, while others suffer from a wide variety of symptoms, such as endocrine disorder, anemia, hypertension, etc. (9,10). Here we report a case of extra adrenal myelolipoma located in mediastinum, and the colony-forming units-megakaryocytes (CFU-M) of this patient present mild mature disturbance with a low platelet count in his bone marrow. We perform a tumor resection under video-assisted thoracic surgery (VATS) and review the literatures and summarize the characteristics of reported patients with mediastinal myelolipoma as well.
Case presentation
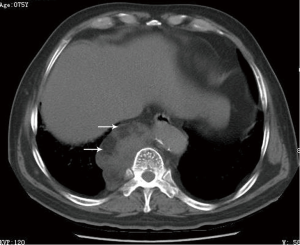
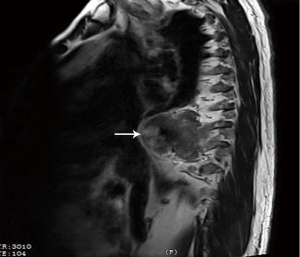
The patient was a 74-year-old male who was referred to our hospital for a routine health check, and detected a mediastinal neoplasm on chest radiography. He had a history of hypertension, and it’s stable to be controlled by medicine. He denied the following symptoms including the presence of chest pain, hoarseness, hemoptysis and cough. Physical examination was normal. Laboratory and equipment examination: chest computed tomography (CT) scan revealed that a lump mixed density shadow in the right posterior mediastinal, next to the spine, the sheet of fat density, whose realm was clear, and measured 75×50×30 mm3 (Figure 1). A little homogeneous enhancement can be seen after injection of contrast agent. Chest magnetic resonance (MR) scan showed that there are regular mass located right front side of the spine with mixed T1 and T2 signal, and we can see short T1 and long T2 signal within the part thoracic (Figure 2). Electrocardiograph (ECG) revealed sinus rhythm and P wave changes. Pulmonary function tests: forced vital capacity (FVC): 2.16 L (accounted for 57.6% of predicted value), forced exp volume in 1 s (FEV1): 1.63 L (accounted for 57.3% of predicted value) and maximum ventilatory volume (MVV): 52.35 L/min (percentage of predicted value of 44.5%), FEV1/FVC %: 75.28%. These results proved his pulmonary ventilatory function and exchange function were both moderately damaged. Echocardiography revealed left ventricular diastolic function decreased, as the left ventricular ejection fractions (LVEF) of this patient was 73% and ESV was 26 mL. Liver and kidney function, blood coagulation function, blood transmitted diseases examination showed normal performance. Routine blood test: leukocyte 3.55×109/L, platelet 50×109/L, hematocrit 0.04, and recheck the platelet still quite low (43×109/L). Then we consulted the doctor of hematology department, and decided further examine. The results presented that the morphology of red blood cells were almost normal, but part of these cells’ size were different. The morphology of platelets was normal, and the small or medium clusters of platelets could be seen. We continued to undertake citrate anticoagulation, the number of platelet became 120×109/L. The bone marrow aspirate examination revealed that there existed a high proportion of CFU-erythroid (CFU-E), while CFU-M were mildly mature disturbance with a low platelet count.
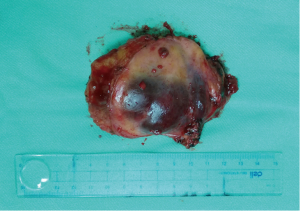
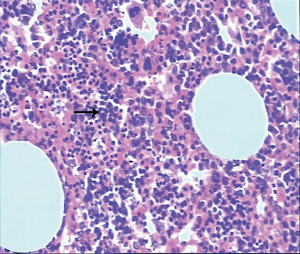
After full preoperative preparation, we carried out intravenous anesthesia with double lumen endotracheal intubation downward, and the lateral decubitus position was used. We performed a tumor resection under VATS. The incisions of triportal VATS included a 1-cm thoracoscopic port on the middle axillary line in the seventh intercostal space (ICS) and two 1.5-cm incisions on the anterior axillary line in the fourth and eighth ICS, respectively. During the VATS procedure, the surgeon stood on the ventral side of the patient to perform the operation with endoscopic suction and an electric coagulation hook. There were no adhesion and pleural effusion within the chest. The tumor was reddish brown and covered with parietal pleura, which was identified in posterior mediastinum. Its boundary was clear. The benign nature of each tumour was confirmed by an intraoperative frozen section. The surgical specimen was taken out completely, and it was approximately 75×50×30 mm3 as a tough, encapsulated texture, appearing a hemangioma (Figure 3). After careful attention to hemostasis, a chest tube was placed to drain the pleural cavity, and the right lung was reinflated under direct vision. All postoperative diagnoses were verified pathologically (Figure 4). The patient was discharged with no complications on the 7th operative day, and thereafter the patient was followed up as outpatient for 1 year. He doesn’t take any additional treatment and without recurrence.
Literatures review
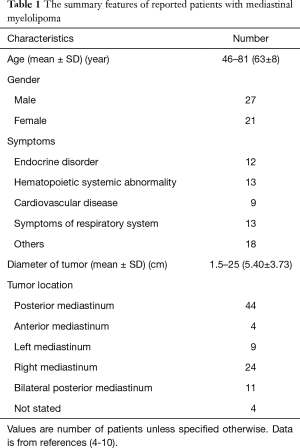
We searched “Mediastinal myelolipoma” as the MeSH terms in PubMed database, and excluded the duplicate cases. We detailed records of sex, age, neoplasm location, clinical symptoms, surgical procedures and other information. There are 33 relevant English literatures, and 48 patients are presented including 27 males and 21 females, their ages between 46 and 81 (64±8) years old. The diameter of tumor ranges from 1.5 to 25 (5.40±3.73) cm. Their clinical manifestations are varied, and there were 18 asymptomatic patients who were detected by imageological examination or autopsy, while 30 patients with atypical symptoms, including chest pain, back pain, cough, anema, etc. The demographic and clinical characteristics of these patients are listed in Table 1. There are 39 cases undergoing tumor resection surgery (Table 2), and without recurrence, malignant transformation and metastasis.
Full table

Full table
Discussion
The primary myelolipoma is a rare benign tumor with hematopoietic and mature adipose tissue composition, which was firstly reported by Gierke in 1905 (1), and named by Oberling in 1929 (2). Myelolipoma is a benign, nonfunctional tumor comprising extensive hematopoietic tissue and sparse fatty tissue. Most cases occur in the adrenal gland, the extra-adrenal location of myelolipoma is extremely unusual (4). These tumors have been reported in presacral region, perirenal, mediastinum, liver, stomach, where the incidence rate decreased. There are only 3% located in the mediastinum (3). Among all reports until now, myelolipoma is mostly located in the right posterior mediastinum (9). Mediastinal medullary lipoma is benign tumor with hormonally inactive, most asymptomatic, generally found incidentally. With the growth of tumor, it may lead to compression of adjacent organs, which result in several non-specific symptoms, such as back pain and coughing, etc. (4).
The etiology of myelolipoma is still unclear now. Here, we summarize several current popular views as follows: the first view was based on the clinical and animal experimental results. It revealed adipocyte cells and myeloid cells may be derived from the zona reticularis of adrenal cortex as the reaction to certain stimuli, such as necrosis, infection, oppression (3). This is currently the mainstream view that how the medullary lipoma formed; the second view is that it originated from the remnants of embryonic tissue, which is mainly is the marrow tissue residues (11); a third view is that the myelolipoma might come from blood-borne planted marrow emboli (12); the fourth view believes the occurrence of myelolipoma is connected with chromosomal abnormalities. Myelolipoma has the characteristic of chromosomal aberration, which presents as 3q25 translocation to 21p41, and partial deletion of 21 or 17 chromosome short arms (13). Thus the occurrence of myeloid lipoma is associated with sharp reduction in cell apoptosis (8,9); the fifth point of suggests that it may be associated with obesity, chronic diseases and adjustments to the hormone change. Obesity-related cases have been reported (14). The patient in our case with myelolipoma are not only examined with axial scan but also checked with MPRs on sagittal plane, because they can be useful in preoperative diagnosis.
Myelolipoma masses are generally round in shape, and the connective tissue formation fake capsule gathers outside. There’re two pathological types: the macroscopic observation of type I is light yellow or orange. Its microscopic examination shows mostly adipose tissue with small focal distribution of hematopoietic tissue, which contains red blood cells. The macroscopic view of Type II is red or reddish brown. Its microscopic examination shows myeloid components, which mainly contain the rich marrow hematopoietic tissue. Pathological confirmation was based on routine light microscopic sections stained by haematoxylin and eosin (H & E). The tumours were composed of adipose tissue and haematopoietic to type I (Figure 4). The tumor in our case is ovoid, well circumscribed, sometimes surrounded by a pseudocapsule. The cut surface typically has a variegated appearance, with areas of greasy-appearing soft yellow tissue alternating with irregular areas of dark red-brown friable tissue.
B ultrasound, CT and magnetic resonance imaging (MRI) are commonly used as a diagnostic method. CT and MRI can effectively diagnose adrenal myelolipoma, but can’t definitely diagnose it (7). CT shows a quasi-circular neoplasm located in the mediastinum and it contains mixed composition, such as calcification, hemorrhage, fat and pseudocapsule. The density of the tumor is approximately equal to adipose (CT value of 20–50 Hu), including fat components (−120– −20 Hu), and bone marrow components (15–40 Hu), while CT enhanced scan is characterized with no obvious strengthening. Pathological results prove the same components compared to the CT image. Calcification is rare, but it has been reported in the literature (11). MRI shows that a soft tissue with thin and sharp boundaries wraps around the masses. We can observe three structural features: (I) the density of the homogeneous mass is the same as surrounding fat tissue; (II) the density of the inhomogeneous mass is similar to the adrenal cortex; (III) the density is different from fat and is lower than the liver nodules (15). The biopsy of CT guided needle puncture combined with the pathological results can definitely diagnose (16). Some reports show that the application of flow cytometry in diagnosis has its characteristic significance (17).
The morphology of myelolipoma is quite typical, and it’s not difficult to identify the most cases. The differential diagnosis includes neurogenic tumors, lymphoma, teratoma, malignant non-seminomas, pleural mesothelioma, lymphadenectasis, malignant mesothelioma, angiolipoma, epidural lipomatosis, ectopic bone marrow and extramedullary hematopoietic tissue (18). The clinical imaging identification characteristics of part disease are summarized as follows: (I) mediastinal neurogenic tumors: there exists the impression trace beside the spine or ribs, and sometimes we can find the signs such as intervertebral foramen expanded and so on. The tumors are generally without the fat component. CT images showed a homogeneous density, rather than mixed a density shadow of myelolipoma (19,20); (II) mediastinal teratoma: the main components are fat and soft tissue, and the image is more difficult to identify when the mass is without bone structure. But the teratoma usually occurs in the anterior mediastinum, and it is generally a large solitary tumor. With the assistant of thoracoscopic or CT guided needle biopsy, the diagnosis is relatively easy (21-23). However, according to our table, mediastinal myelolipoma mostly occurring in posterior mediastinum (92%), it is difficult to biopsy accurately by fineneedle aspiration from anterior chest wall, which can be associated with a risk simultaneously, such as hemorrhage, pneumothorax etc. The spine blocks the fine-needle aspiration if entering from posterior chest wall. Therefore, fine-needle aspiration with posterior mediastinum is not be advocated in our opinion. In this case, we talked with the patient, and then he decided to take a surgery directly; (III) mediastinal lymph nodes intumescentia: it generally has characteristic manifestation. Malignant metastasis tumor often comes from its primary lesions, and may find multiple parts of the lymph node intumescentia. If the mediastinal lymph nodes are caused by tuberculosis, we may find typical tuberculosis lesions in pulmonary. Normally, the performance of lymphoma is a plurality of lymph nodes intumescentia, and may be associated with other parts of the lymph nodes. The sarcoidosis generally causes slight symptoms, and bilateral hilar lymph nodes involved mainly (24,25); (IV) adult extramedullary hematopoiesis: it often has chronic anemia manifestations, and CT scan identifies the spindle or irregularly shaped nidus without capsule. It is important to identify myelolipoma and extramedullary hematopoiesis. The microscopic features of extramedullary hematopoiesis are similar to myelolipoma. Despite extramedullary hematopoiesis, the patient with chronic anemia symptom is often due to the blood system diseases such as the mediterranean anemia and hereditary spherical. So it can be used to distinguish between myelolipoma and extramedullary hematopoiesis (14). The blood test of our case showed low platelets, bone marrow examination revealed a high proportion of CFU-E, while CFU-M were mild mature disturbance with a low platelet count. The morphology of red blood cells was almost normal, but part of these cells’ sizes were different. The morphology of platelets were normal, and the small or medium clusters of could be seen. After citrate anticoagulation, the number of platelets became normal. Microscopically, the tumor of this case is composed of a variable admixture of mature adipose tissue with islands and nests of hematopoietic elements of different percentages. In our patient, there were no bone spurs or hyperplasia of any hematopoietic component, and the adipose component did not present atypia. Considering no literature about primary thrombocytopenic has been reported, we think this symptom of our patient may be induced by immune factors. Hence, this hypothesis needs to be further research with more similar cases.
From our table, the tumor size ranges from 1.5 to 25 cm, which reveals that the myelolipoma has potential of continuous growth. Conventional treatments of the myelolipoma are observation and operation. There is no standard method for this disease. Mediastinal tumors is often difficult to determine whether benign or malignant before operation, but as the tumor increases, it may become malignant and oppress the adjacent organs, even causing blood vessel rupture and bleeding, secondary infection, etc. So most of the myelolipoma treatment is surgical resection currently. When the tumors gradually expand, or clinical symptoms appear, such as chest pain, pleural effusion or superior vena cava obstruction, the patients need to actively undertake surgery treatment. At present, many literatures point out that if the diameters of the asymptomatic tumors are less than 40 mm, the patients could choose dynamic observation rather than surgery temporarily. Since asymptomatic tumor diameter is greater than 7 cm, it’s more likely to lead to rupture and hemorrhage, or through dynamic observation tumor is found increasing gradually, or the patients suffer from clinical symptoms, in any one of which cases above they need an actively operative treatment (16). The surgical approach (VATS or thoracotomy) is determined according to the size and local invasion of each tumour. Minimally invasive thoracoscopic has been gradually and widely accepted. It is widely accepted that we can take VATS surgery to resect the tumor, the diameter of which is less than 80 mm (8). Triportal VATS was the most commonly used procedure. Compared with open thoracotomy, this minimally invasive procedure was related with many advantages, such as less trauma, faster recovery, etc. During operations, we also noted that primary mediastinal myelolipoma (PMM) was a tumour with rich blood supplies, which arose predominantly from the branches of the aorta or intercostal arteries. The main difficulty during resection of PMMs via VATS lies in how to safely divide these vessels, while an open thoracotomy was more suitable for the resection of tumours of larger size (9). In this study, we presented the case of PMM patient undergoing VATS resection successfully. In our table, more and more patients were operated by VATS. With the improvement of endoscopic techniques and equipments, minimally invasive thoracoscopic has gradually become an important method for the resection of mediastinal myelolipoma.
Conclusions
Mediastinal myelolipoma is a rare benign tumor of mesenchymal origin. The pathogenesis of myelolipoma still remains unclear. Most of the cases don’t feel discomfort and are just discovered by X-ray examination incidentally. However the tumors may cause some unspecific oppression symptoms as the tumors are growing up. Preoperative diagnosis is extremely difficult. CT and MRI are of some help for diagnosis of mediastinal myelolipoma, and the “golden standard” of diagnosis still needs postoperative pathologic examination. Therefore, once the mediastinal myelolipoma is found, especially unconfirmed behavior of the tumor, surgery is a preferred treatment for patient in our opinion. Particularly, the VATS is a promising alternative, and more studies are needed to better understand the features of PMM.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
References
- Gierke E. Uber Knochenmarksgwebe in der Nebenniere. Zeiglers Beitr Path Anat 1905;7:311-24.
- Oberling C. Les myelolipomamateuses. Bull Assoc Fr Etudes. Cancer 1929;18:234-46.
- Nakagawa M, Kohno T, Mun M, et al. Bilateral video-assisted thoracoscopic surgery resection for multiple mediastinal myelolipoma: report of a case. Korean J Thorac Cardiovasc Surg 2014;47:189-92. [Crossref] [PubMed]
- Xiong Y, Wang Y, Lin Y. Primary myelolipoma in posterior mediastinum. J Thorac Dis 2014;6:E181-7. [PubMed]
- Oliveira CC, Felisberto G. Myelolipoma of the posterior mediastinum in a patient with chronic dyserythropoietic anemia. Autops Case Rep 2016;6:35-9. [PubMed]
- Fonda P, de Santiago E, Guijarro M, et al. Mediastinal myelolipoma with leukocytosis. BMJ Case Rep 2013;2013. pii: bcr2013010349.
- Hosaka T, Hata Y, Makino T, et al. Mediastinal myelolipoma showing gradual enlargement over 9 years: a case report. J Cardiothorac Surg 2016;11:91. [Crossref] [PubMed]
- Himuro N, Minakata T, Oshima Y, et al. Video-assisted thoracic surgery for primary myelolipoma of the posterior mediastinum. J Cardiothorac Surg 2016;11:1. [Crossref] [PubMed]
- Lin F, Pu Q, Ma L, et al. Surgical treatment of primary mediastinal myelolipoma. Interact Cardiovasc Thorac Surg 2015;21:206-10. [Crossref] [PubMed]
- Shen C, Han Z, Che G. A bilateral neoplasm in chest: a case report and literature review. BMC Surg 2014;14:42. [Crossref] [PubMed]
- Vaziri M, Sadeghipour A, Pazooki A, et al. Primary mediastinal myelolipoma. Ann Thorac Surg 2008;85:1805-6. [Crossref] [PubMed]
- Krag D, Reich SB. Heterotopic bone marrow (myelolipoma) of the mediastinum. Chest 1972;61:514-5. [Crossref] [PubMed]
- Meyer A, Behrend M. Presentation and therapy of myelolipoma. Int J Urol 2005;12:239-43. [Crossref] [PubMed]
- Migliore M, Calvo D, Criscione A, et al. An unsual symptomatic case of mediastinal myelolipoma treated by VATS approach. Ann Ital Chir 2014;85:85-7. [PubMed]
- Kawanami S, Watanabe H, Aoki T, et al. Mediastinal myelolipoma: CT and MRI appearances. Eur Radiol 2000;10:691-3. [Crossref] [PubMed]
- Geng C, Liu N, Yang G, et al. Primary mediastinal myelolipoma: A case report and review of the literature. Oncol Lett 2013;5:862-4. [PubMed]
- Saboorian MH, Timmerman TG, Ashfaq R, et al. Fine-needle aspiration of a presacral myelolipoma: a case presentation with flow cytometry and immunohistochemical studies. Diagn Cytopathol 1999;20:47-51. [Crossref] [PubMed]
- Minamiya Y, Abo S, Kitamura M, et al. Mediastinal extraadrenal myelolipoma: report of a case. Surg Today 1997;27:971-2. [Crossref] [PubMed]
- Foster JB. Primary thoracic myelolipoma: case report. AMA Arch Pathol 1958;65:295-7. [PubMed]
- Gao B, Sugimura H, Sugimura S, et al. Mediastinal myelolipoma. Asian Cardiovasc Thorac Ann 2002;10:189-90. [Crossref] [PubMed]
- Franiel T, Fleischer B, Raab BW, et al. Bilateral thoracic extraadrenal myelolipoma. Eur J Cardiothorac Surg 2004;26:1220-2. [Crossref] [PubMed]
- Mohan K, Gosney JR, Holemans JA. Symptomatic mediastinal myelolipoma. Respiration 2006;73:552. [Crossref] [PubMed]
- Rossi M, Ravizza D, Fiori G, et al. Thoracic myelolipoma diagnosed by endoscopic ultrasonography and fine-needle aspiration cytology. Endoscopy 2007;39 Suppl 1:E114-5. [Crossref] [PubMed]
- Bastion Y, Coiffier B, Felman P, et al. Massive mediastinal extramedullary hematopoiesis in hereditary spherocytosis: a case report. Am J Hematol 1990;35:263-5. [Crossref] [PubMed]
- Schön HR, Emmerich B, Arnold H, et al. Hemolytic anemia with pyruvate kinase deficiency presenting as paravertebral myelolipoma. Klin Wochenschr 1984;62:133-7. [Crossref] [PubMed]


