Trans-tracheostomy repair of tracheo-esophageal fistula under endoscopic view in a 75-year-old woman
Introduction
Tracheoesophageal fistula (TEF) is an abnormal communication between the esophagus and the trachea which can be congenital and acquired. Congenital TEF is a relatively rare condition that occurs in 1 of 2,400–4,500 births (1). It is caused by an abnormal septation of the caudal foregut during the fourth and fifth weeks of embryonic development. Most of the patients with TEF are diagnosed following birth or during infancy. Acquired TEF is distinct in malignant and benign. Malignant TEF occurs secondary to several malignancies (i.e., esophageal cancer). Internal trauma (i.e., from cuff pressure of endotracheal tube or nasogastric tube or combination of both) or external trauma (i.e., from penetrating foreign bodies, open or closed aero-digestive tract injuries) are the main causes of benign TEF (2,3). Contamination of the tracheobronchial tree and interference with nutrition are life threatening aspects of this condition. Surgery is the treatment of choice (4). Unfortunately, the most of patients are not surgical candidate due to poor clinical conditions. Despite several endoscopic procedures have been reported as alternative to surgery for closing TEF, the ideal strategy is yet to be determined.
Herein, we reported a new minimally invasive treatment of acquired benign TEF as its trans-tracheotomy closure under endoscopic view (Figure 1).
Case presentation
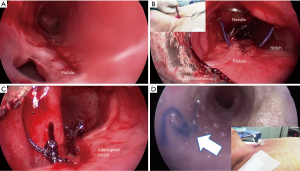
A 75-year-old-woman was referred to our attention for management of TEF. One month before, she was intubated for acute respiratory failure and a naso-gastric tube was also placed; ten days later a percutaneous tracheostomy was performed. After weaning from mechanical ventilation, she complained episodes of coughing with feedings, recurrent pneumonia and bodyweight loss. Bronchoscopy showed the presence of a TEF fistula localized 3.5 cm below the vocal folds and extended 3 cm distally (Figure 2A). Esophagography confirmed the TEF without esophageal stricture. The patient’s poor clinical condition contraindicated surgery while the large dimension of fistula prevented any successful repair with standard endoscopic procedures as placement of fibrin glue, clipping, or stenting. Thus, she was scheduled for the following minimally invasive procedure.
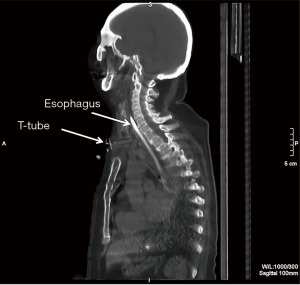
Under general anaesthesia, the patient was intubated with a rigid tracheoscopy that was advanced at the level of proximal end of the fistula. The cannula was removed and a standard needle-holder was inserted through the tracheotomy (Figure 2B). Under endoscopic view the tear was closed from the distal to the proximal ends with vycril 4/0 interrupted stitch (Figure 2C). The knot was started extra corporeally and the suture was pushed and tied inside the trachea, through the tracheostomy, with the needle-holder giving the right tension to the ligature. After closure, a Montgomery T tube was inserted in a standard manner to protect the suture and maintain the air-way patency (Figure 2D). Esophagography and chest computed tomography scan confirmed the complete healing of the fistula (Figure 3). At the last follow-up (7 months after the procedure), the patient was alive and tolerated a full diet.
Discussion
TEF can be classified into congenital and acquired condition. Acquired origin can be subdivided into benign or malignant forms. In the malignant category of TEF, esophageal tumor accounts for three-fourths of total cases. Among the benign conditions, prolonged mechanical ventilation is the most common (47%), followed by injury (17%), prior laryngectomy (17%), and prior esophagostomy (17%) (4). The rate of TEF in tracheostomy patients is 0.5% and high cuff pressure, excessive motion of the tube, infection, steroid therapy, diabetes and the use of nasogastric tube are all risk factors for its development. If left untreated, TEF can be fatal due to poor nutrition and severe pulmonary complications caused by tracheobronchial contamination. Surgery is the treatment of choice involving repair of fistula and resection with reconstruction of trachea, if necessary; in patients unfit for surgery, endoscopic treatment is a valid alternative to surgery to restore the patient’s normal breathing and oral intake while spontaneous healing of TEF is an exceptional event.
In the present case, the combination of tracheostomy cuff pressure and nasogastric tube caused the erosion of the tracheal and esophageal walls with development of TEF. The clinical condition of the patient needed an emergent intervention that resulted particularly challenging; surgery was unfeasible due to poor patient’s clinical condition while standard procedures of endoscopic repair as application of fibrin glue (6), clipping (7), or stenting (8) resulted to be not indicated for the characteristics of the TEF. The application of fibrin glue (6) alone or in association with clipping (7) is reported to close congenital small TEF (<1 cm) but it would have had a high failure rate in this case due to the large size of fistula (3 cm). Esophageal or airway Self-expanded metallic stent (SEMS) are also used for closing TEF (8). However, we decided against the insertion of esophageal stent for the high risk of migration due to the normal esophageal lumen. Also the use of air-way stent was not-indicated because the radial force of the stent could avoid the opposition of the margin of the fistula preventing its healing. In addition, airway stent closed the tracheotomy making challenging an urgent ventilation in case of acute respiratory distress due to the underlying lung disease of patient. Recently, endoscopic chemocauterization using trichloroacetic acid (TCA) has been reported as minimally invasive treatment of TEF. The chemical burn created a scar at the cauterized site with healing of fistula. In 2008, Sung et al. (1) firstly reported the full closure of recurrent TEF after open repair in three cases with endoscopic application of TCA. Following, Lelonge et al. (9) confirmed these results, reporting the complete closure of 14 TEFs with the same technique. The median follow-up was 41 months (8–72 months). No recurrences were found and all patients were asymptomatic. Despite these encouraging results, the lack of familiarity with this technique discouraged us to use it. Thus, we planned a minimally invasive strategy, not been reported before, as the direct suture of the tear through the tracheotomy. The entire procedure was performed with rigid bronchoscopy that allowed to ventilate patient, to guide in real-time the surgical maneuvers inside the trachea, and to insert T tube after closure of fistula (10).
For the success of our procedure, standard needle should be bent to a 90 degree angle to facilitate the surgical maneuvers into a tight and angled anatomical district as the trachea. In addition, we recommended to close the tear with interrupt sutures from the distal to the proximal edge of the tear. Obviously, our procedure is indicated for repair fistula localized at level of tracheotomy or few millimeters below it while fistula involving the carina or extending below it cannot be treated with our technique.
In closure, our technique is simple, safe and indicated also in unfit patient due to its limited invasiveness. Thus, it could be useful for surgeon in management of tracheotomy related tears when an opening in the trachea already exists. Larger series with longer follow-up are required before recommending its standard use.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
References
- Sung MW, Chang H, Hah JH, et al. Endoscopic management of recurrent tracheoesophageal fistula with trichloroacetic acid chemocauterization: a preliminary report. J Pediatr Surg 2008;43:2124-7. [Crossref] [PubMed]
- Fiorelli A, Esposito G, Pedicelli I, et al. Large tracheobronchial fistula due to esophageal stent migration: Let it be! Asian Cardiovasc Thorac Ann 2015;23:1106-9. [Crossref] [PubMed]
- Caronia FP, Fiorelli A, Arrigo E, et al. Management of subtotal tracheal section with esophageal perforation: a catastrophic complication of tracheostomy. J Thorac Dis 2016;8:E337-9. [Crossref] [PubMed]
- Muniappan A, Wain JC, Wright CD, et al. Surgical treatment of nonmalignant tracheoesophageal fistula: a thirty-five year experience. Ann Thorac Surg 2013;95:1141-6. [Crossref] [PubMed]
- Caronia FP, Fiorelli A, Reginelli A, et al. Patient was intubated and ventilated with rigid bronchoscopy. Asvide 2017;4:116. Available online: http://www.asvide.com/articles/1426
- Gutierrez C, Barrios JE, Lluna J, et al. Recurrent tracheoesophageal fistula treated with fibrin glue. J Pediatr Surg 1994;29:1567-9. [Crossref] [PubMed]
- Propst EJ, Ling SC, Daneman A, et al. Endoscopic clip for closure of persistent tracheoesophageal fistula in an infant. Laryngoscope 2014;124:2182-5. [Crossref] [PubMed]
- Ke M, Wu X, Zeng J. The treatment strategy for tracheoesophageal fistula. J Thorac Dis. 2015;7:S389-97. [PubMed]
- Lelonge Y, Varlet F, Varela P, et al. Chemocauterization with trichloroacetic acid in congenital and recurrent tracheoesophageal fistula: a minimally invasive treatment. Surg Endosc 2016;30:1662-6. [Crossref] [PubMed]
- Fiorelli A, Mazzone S, Di Crescenzo VG, et al. A simple technique to control placement of Dumon stent in subglottic tracheal stenosis. Interact Cardiovasc Thorac Surg 2014;18:390-2. [Crossref] [PubMed]


