Factors associated with treatment outcome in 64 HIV negative patients with multidrug resistant tuberculosis
Introduction
Drug resistant tuberculosis is the consequence of poor tuberculosis control programmes and today a global health problem (1,2). Drug resistance develops as a result of spontaneous genetic mutations in Mycobacterium tuberculosis, which are selected if antituberculosis drugs are used inappropriately or inconsistently (3). Multidrug resistant tuberculosis (MDR TB) is defined as resistance to at least two important drugs as isoniazid (H) and rifampicin (R) (4). MDR TB results from an organism that acquires drug resistance either because of inadequate therapy or from transmission of an already resistant organism (5).
Previous studies have shown that patients with drug resistant tuberculosis have lower response rates than those with drug susceptible isolates. Rifampicin and isoniazid are the most active antituberculosis drugs. When R resistance occurs in the presence of resistance to H, the prospects for successful chemotherapy greatly decrease (6-8). MDR TB among previously untreated patients is mostly related to human immunodeficiency virus (HIV) co-infection (9). Also, in patients severely immunosuppressed by HIV infection have lower response rate and high fatality rate than HIV negative cases for MDR TB treatment (6). In this study we aimed to determine the factors associated with treatment outcome in HIV negative patients with MDR TB.
Material and methods
Patients
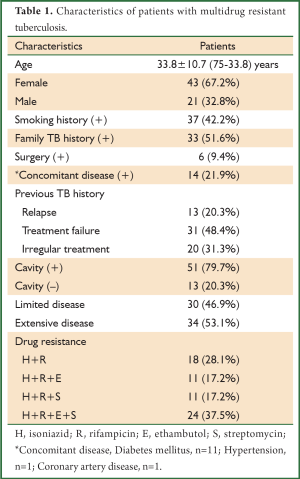
The study comprised 64 patients hospitalized in a reference hospital between 1998-2006 with a diagnosis of MDR TB. All cases were negative for HIV serologic test. Each patient’s demographic profile, medical history, clinical, radiological findings, sputum smear examination, complete blood count, drug susceptibility pattern and previous treatment details were recorded. The characteristics of the patients were shown in Table 1. The diagnoses were performed with the documentation of acid fast bacilli (AFB) through Ziehl-Neelsen (ZN) staining of sputum and the isolation of Mycobacterium tuberculosis in sputum culture in liquid medium (BACTEC) and/or Lowenstein-Jensen solid medium. Drug susceptibility test was performed routinely for all cases using Lowenstein-Jensen medium and the method of proportions.
All patients had a history of receiving firstline antituberculosis treatment. According to the previous TB history patients were classified as relapse (recurrence of positive smear or culture after achievement of cure), treatment failure (persistent smear or culture positivity in the 5th month of the treatment) and irregular treatment. Patients who met these criteria and also having resistance to both H and R in the drug susceptibility test were diagnosed as MDR TB. Also, the disease was classified as extensive or limited on the basis of the radiological findings. Extensive disease was defined as the infiltrates involving at least 75% of the lung fields or the presence of cavities totaling at least 15 cm in diameter (10).
Treatment regimen
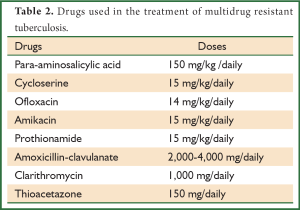
After the diagnosis of MDR TB drugs (para-aminosalicylic acid, cycloserine, ofloxacin, amikacin, prothionamide, thioacetazone, amoxicillin-clavulanate and clarithromycin) were included into the treatment regimen. The administration of all drugs was initiated at the same time with dose intervals adjusted according to the patients’ tolerance. All patients took their drugs regularly in directly observed treatment (DOT) programme and hospitalized until sputum AFB smears were negative for 3 consecutive days. Drugs that had serious side effects were withdrawn from the regimen. Surgical resection was considered after 2 months of the medical treatment. Follow up evaluations included sputum smear and culture examinations and the chest radiography obtained every month. Treatment was continued for at least 18 months after the first negative culture had been obtained. Achievement of sputum AFB negativity in the 3rd month of the treatment was accepted as the bacteriologic response (6).
Statistical analysis
Statistical analysis was performed using Statistical Package for Social Sciences (SPSS Inc, Chicago, IL) for windows release 11.0. The difference between the variables based on bacteriologic response was analyzed by Fisher’s Exact test. Logistic regression analysis was performed to determine the factors predicting bacteriologic response. The Odds ratios (OR) and 95% confidence intervals (CI) were determined. A value of P<0.05 was considered as statistically significant.
Results
In this study there were 43 (67.2%) female and 21 (32.8%) male patients with a mean age of 33.8±10.7 (75-33.8) years. The characteristics of the patients were shown in Table 1. Patients were classified according to their previous TB history as 13 (20.3%) with relapse, 31 (48.4%) with treatment failure and 20 (31.3%) patients with irregular treatment. Also, 51 (79.7%) patients had cavity and 34 (53.1%) patients had extensive disease whereas, 30 (46.9%) patients had limited disease. Drug susceptibility test was obtained from all patients. Eighteen (28.1%) patients had H+R resistance, 11 (17.2%) had H+R+E resistance, 11 (17.2%) had H+R+S resistance and 24 (37.5%) had H+R+E+S resistance.
Full Table
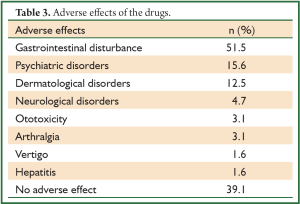
The mean duration time of the treatment was 16.4±8.2 months. The MDR TB drugs and the doses used were listed in Table 2. In our clinic usually we prefer para-aminosalicylic acid, cycloserine, ofloxacin, amikacin, prothionamide and thioacetazone combination (6 drugs) for MDR TB treatment. However in our study only 45 (70.3%) patients received this combination, 14 (21.9%) patients could not receive thiocetazone because of economic problems. Also in 5 (7.8%) patients amoxicillin-clavulanate and clarithromycin were included into this combination if one or more drugs were withdrawn because of side effects. In 39 (60.9%) patients adverse effects of the drugs were seen with the frequency of gastrointestinal disturbance (51.5%), psychiatric disorders (15.6%), dermatological effects (12.5%), neurological disorders (4.7%), ototoxicity (3.1%), arthralgia (3.1%), vertigo (1.6%) and hepatitis (1.6%) (Table 3). In 3 patients cycloserine was withdrawn because of psychiatric and neurological disorders, in 1 patient prothionamide caused hepatitis and the drug was withdrawn, in 2 patients amikacin treatment was not completed because of ototoxicity.
Full Table
Full Table
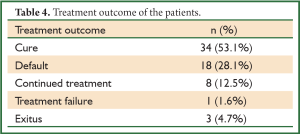
The mean time of sputum smear negativity was determined as 3±2.2 months. In our manuscript 34 (53.1%) patients were cured and the cure was defined as negative smears and cultures throughout treatment for at least 18 months. Treatment outcome of the other patients was determined as default in 18 (28.1%), treatment failure in 1 (1.6%) and exitus in 3 (4.7%) patients. Also, 8 (12.5%) patients in whom bacteriologic response was achieved in the 3rd month had incomplete treatment (Table 4).
Full Table
Patients who received MDR TB treatment for at least 3 months were evaluated and the achievement of sputum AFB negativity in the 3rd month was accepted as the bacteriologic response. In our study bacteriologic response was determined in 47 (73.4%) patients. Older age (P=0.04), absence of cavity (P=0.011) and extensive disease (P=0.000) were found higher in patients with bacteriologic response (Table 5).
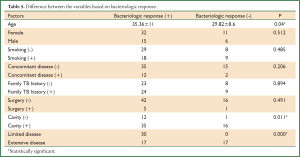
Full Table
In logistic regression analysis only presence of cavity and the extensive disease were found as the predictors of bacteriologic response (OR=1.5, 95% CI: 1.23-1.82, P=0.01 and OR=2, 95% CI: 1.42-2.79, P=0.00, respectively). However age, sex, previous TB history and drug resistance pattern did not show any association with the bacteriologic response (Table 6).
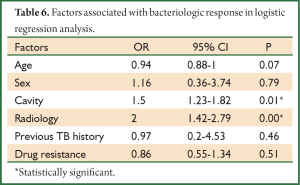
Full Table
Discussion
MDR TB is a growing public health problem in all over the world. The treatment of MDR TB is very important because of the risk of transmitting virtually untreatable drug resistant disease. Many factors may affect the treatment outcome. In our study cure was achieved in 34 (53.1%) patients and bacteriologic response was determined as 73.4%.
Treatment response rates in MDR TB were determined different in the previous studies. HIV positive patients were found to have lower response rate than HIV negative patients (6). Park et al. evaluated 173 patients with MDR TB of whom over half were known to be HIV infected. They found mortality significantly greater for HIV positive patients than for HIV negative group (11). In another study of Park et al., only 63 HIV negative patients with MDR TB were analyzed and 82.5% of the patients were found to have microbiologic responses (6). In addition, Goble et al. reported an overall response rate of 56% and the mortality 22% in 171 patients with MDR TB (10), whereas Telzak et al. found 96% clinical response in 25 HIV negative MDR patients (12). In our study as all of the patients were HIV negative, we could not have the chance to compare the HIV negative and the HIV positive patients.
Tahaoglu et al. reported bacteriologic response rate of 95% in MDR TB and a successful outcome achieved in 73% of cases with medical therapy alone. Also they found resistance to more than five drugs associated with poor outcome, whereas younger age and absence of ofloxacin in the previous treatments were found as associated with successful outcome (13). In our study presence of cavity and extensive disease were found to be associated with bacteriologic response. Chan et al. analyzed the outcomes in 205 patients with MDR TB and compared the results with the previous series. They found greater long-term success rates, 75% versus 56%, and lower tuberculosis death rates, 12% versus 22%, than the earlier study. They also reported surgical resection and fluoroquinolone therapy associated with improved microbiological and clinical outcomes (14). All of our patients had ofloxacin in the MDR treatment and this may be an important reason for the high rate of bacteriologic response.
MDR TB treatment is both toxic and expensive. The drugs have many side effects which cause to interrupt the therapy. In our patients gastrointestinal disturbance (51.5%), psychiatric disorders (15.6%) and dermatological effects (12.5%) were determined as the most frequent adverse effects. Also Torun et al. evaluated 263 patients for the adverse effects of MDR TB treatment retospectively. They found ototoxicity (41.8%), psychiatric disorders (21.3%), gastrointestinal disturbance (14.0%) as the most frequent side effects. These effects led the clinicians to withdraw one or more drugs from the treatment regimen in 146 (55.5%) cases (15).
In conclusion, although radiological findings might affect the bacteriologic response, MDR TB is a treatable disease if regular and appropriate treatment regimen is administered. However treatment is difficult because of toxicity of the drugs and the length of the therapy.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Churchyard GJ, Corbett EL, Kleinschmidt I, et al. Drug-resistant tuberculosis in South African gold miners: incidence and associated factors. Int J Tuberc Lung Dis 2000;4:433-40. [PubMed]
- Pablos-Méndez A, Raviglione MC, Laszlo A, et al. Global surveillance for antituberculosis-drug resistance, 1994-1997. World Health Organization-International Union against Tuberculosis and Lung Disease Working Group on Anti-Tuberculosis Drug Resistance Surveillance. N Engl J Med 1998;338:1641-9. [PubMed]
- Quy HT, Lan NT, Borgdorff MW, et al. Drug resistance among failure and relapse cases of tuberculosis: is the standard re-treatment regimen adequate? Int J Tuberc Lung Dis 2003;7:631-6. [PubMed]
- Bengisun JS, Karnak D, Palabiyikoglu I, et al. Mycobacterium tuberculosis drug resistance in Turkey, 1976-97. Scand J Infect Dis 2000;32:507-10. [PubMed]
- Friedman CR, Stoeckle MY, Kreiswirth BN, et al. Transmission of multidrug-resistant tuberculosis in a large urban setting. Am J Respir Crit Care Med 1995;152:355-9. [PubMed]
- Park SK, Kim CT, Song SD. Outcome of chemotherapy in 107 patients with pulmonary tuberculosis resistant to isoniazid and rifampin. Int J Tuberc Lung Dis 1998;2:877-84. [PubMed]
- Vall-Spinosa A, Lester W, Moulding T, et al. Rifampin in the treatment of drug-resistant mycobacterium tuberculosis infections. N Engl J Med 1970;283:616-21. [PubMed]
- Mitchison DA, Nunn AJ. Influence of initial drug resistance on the response to short-course chemotherapy of pulmonary tuberculosis. Am Rev Respir Dis 1986;133:423-30. [PubMed]
- Robert J, Trystram D, Truffot-Pernot C, et al. Twenty-five years of tuberculosis in a French university hospital: a laboratory perspective. Int J Tuberc Lung Dis 2000;4:504-12. [PubMed]
- Goble M, Iseman MD, Madsen LA, et al. Treatment of 171 patients with pulmonary tuberculosis resistant to isoniazid and rifampin. N Engl J Med 1993;328:527-32. [PubMed]
- Park MM, Davis AL, Schluger NW, et al. Outcome of MDR-TB patients, 1983-1993. Prolonged survival with appropriate therapy. Am J Respir Crit Care Med 1996;153:317-24. [PubMed]
- Telzak EE, Sepkowitz K, Alpert P, et al. Multidrug-resistant tuberculosis in patients without HIV infection. N Engl J Med 1995;333:907-11. [PubMed]
- Tahaoğlu K, Törün T, Sevim T, et al. The treatment of multidrug-resistant tuberculosis in Turkey. N Engl J Med 2001;345:170-4. [PubMed]
- Chan ED, Laurel V, Strand MJ, et al. Treatment and outcome analysis of 205 patients with multidrug-resistant tuberculosis. Am J Respir Crit Care Med 2004;169:1103-9. [PubMed]
- Törün T, Güngör G, Ozmen I, et al. Side effects associated with the treatment of multidrug-resistant tuberculosis. Int J Tuberc Lung Dis 2005;9:1373-7. [PubMed]


